HomeChildren's clinicCardiologyCarditis
Carditis is an inflammatory lesion of the heart of various etiologies that is not associated with rheumatism or other systemic diseases. In pediatrics, the expediency of using the term “carditis” is justified by the possibility of simultaneous damage to two or three membranes of the heart (endo-, myo- or pericardium).
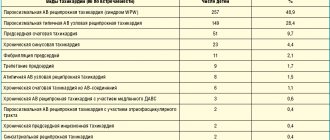
The classification of non-rheumatic carditis, used in pediatric practice, involves identifying the period of occurrence [congenital (early, late) and acquired], etiology, nature of the course (acute, subacute, chronic), severity, severity of heart failure, possible outcomes and complications of the disease.
Symptoms
- Acute carditis
Manifestations of intoxication (pallor, fatigue, sweating, decreased appetite, slight increase in body temperature, etc.); pain in the heart area; weak, rapid, often arrhythmic pulse; expansion of the boundaries of the heart; decreased blood pressure; disturbance of cardiac rhythm, presence of systolic murmur; pericarditis (in some young patients). - Subacute carditis
Manifestations of intoxication (pallor, increased fatigue, irritability, etc.); dystrophy; heart failure, which develops gradually; arrhythmias, systolic murmur; increase in heart size. - Early congenital carditis
Low birth weight; fatigue when feeding; causeless anxiety; sweating, pallor; cardiomegaly, dull heart sounds; “heart hump” (protrusion of the heart area); progressive heart failure. - Late congenital carditis
Disorders of cardiac rhythm and conduction; moderate cardiomegaly; loud heart sounds; mild heart failure.
Recognition of non-rheumatic carditis in children should be carried out with the mandatory participation of a pediatric cardiologist. The diagnosis of non-rheumatic carditis in children is helped by a set of clinical and instrumental data: electrocardiography, radiography, ultrasound of the heart, immunological blood test.
Viral carditis
Treatment of viral carditis consists of two stages: inpatient (acute period or exacerbation) and outpatient or sanatorium (period of maintenance therapy). When treating children with carditis, it is necessary to carry out etiotropic, pathogenetic and symptomatic therapy aimed at restoring impaired functions and normalizing hemodynamics.
In the acute period of viral carditis, it is recommended to limit the child’s physical activity for 1-2 weeks (sometimes in severe cases this restriction is extended). However, bed rest should not be prescribed for a long time, since detraining negatively affects the cardiovascular system and the course of non-rheumatic carditis.
The nutrition of patients in the acute period in the absence of signs of circulatory failure should be complete, with a sufficient content of vitamins, proteins, fats and carbohydrates. If there are signs of circulatory failure, the content of table salt is limited to 3-5 g/day, and the amount of liquid - to 1 - 1.5 liters, or the drinking regime is determined based on the amount of urine excreted: the child receives 200-300 ml less fluid than diuresis. As circulatory failure is eliminated, the amount of liquid and table salt is increased to the age norm.
Products with increased amounts of potassium salts (raisins, dried apricots, figs, nuts, prunes, baked potatoes) must be included in the diet, especially when diuretics and glucocorticoids are prescribed. In the acute period of non-rheumatic carditis, foods that have a stimulating effect on the cardiovascular system are completely excluded from the diet: coffee, strong tea, spices, horseradish, garlic, etc.
Treatment for viral infections has not yet been considered successful. The effectiveness of existing antiviral drugs , in particular interferon, is low, and it should be prescribed only at the early stage of carditis, when viruses are in the myocardium.
Pathogenetic therapy is more active , aimed at inhibiting the inflammatory process and eliminating immune disorders. Non-steroidal anti-inflammatory drugs are widely used: salicylates, derivatives of pyrazolone (reopyrin), indoleacetic acid (indomethacin, methindol), phenylpropionic acid (brufen, naproxin), phenylacetic acid (voltaren). These drugs exert their anti-inflammatory effects through several mechanisms. They reduce the energy supply to inflammation, inhibiting the formation of ATP in inflammatory foci, reduce the formation of prostaglandins, histamine and other inflammatory mediators, and improve microcirculation by inhibiting platelet aggregation.
Non-steroidal anti-inflammatory drugs are prescribed according to the usual regimens: acetylsalicylic acid in a dose of 0.15-0.2 g per 1 year of life per day or 50 mg per 1 kg of body weight, indomethacin 1-2 mg per 1 kg of body weight per day, ibuprofen (Brufen) 10 mg per 1 kg of body weight per day, voltaren 2-3 mg per 1 kg of body weight per day for 3-6 weeks.
Glucocorticoids are indicated for diffuse carditis and the presence of heart failure, carditis with predominant damage to the conduction system of the heart. Corticosteroids are also required in the treatment of carditis that occurs due to allergies and systemic diseases. Prednisolone is used orally at the rate of 1 -1.5 mg per 1 kg (within 30-45-60 mg) for 4 weeks, followed by a gradual reduction by 1/3-1/4 tablets (1 tablet - 5 mg) in 3 - 4 days in children of the first three years of life and 1/2 tablet in older children. If the effect is insufficient, a maintenance dose of prednisolone (0.5 mg per 1 kg per day) is used for several weeks. If, despite treatment, the process becomes subacute or chronic, it is recommended to prescribe drugs of the aminoquinoline series (delagil, plaquenil). These drugs have anti-inflammatory (stabilize lysosomal membranes and inhibit nucleic acid metabolism) and anti-sclerotic effects. Initially, they are used at a dose of 10 mg per 1 kg of body weight, then - 5 mg per 1 kg once a day after dinner for 6-8 months.
Since kinins play a certain role in the pathogenesis of viral carditis, preventing the damaging effects of kinins formed during activation by antigen-antibody complexes is achieved by prescribing antikinin drugs: parmidine (anginin, prodectin), contrical, etc. Parmidine is used at 0.25-0.75 g/day for 3-4 weeks.
If there are changes in the microcirculatory system (slowing down the speed of blood flow with the formation of stasis and microthrombi), anticoagulants are used: heparin (120-150 units per 1 kg of body weight), chimes or dipyridamole (5 mg per 1 kg of body weight per day).
To improve impaired metabolism in myocardial cells, cardiotropic therapy is prescribed. Polarizing mixture (10% glucose solution 10-15 mg per 1 kg, 1 unit of insulin per 3 g of administered sugar, panangin 1 ml per year of life, 2-5 ml of 0.25% novocaine solution).
In addition, to improve coronary blood flow, increase the bioenergetic activity of the myocardium, and stimulate redox processes at the cellular level, riboxin (ATP precursor) is used, which penetrates cells and has virtually no side effects. The drug is prescribed 1-2 tablets (1 tablet - 0.2 g) 3 times a day (before meals) for 1 month, then 1/2 - 1 tablet 2 times a day for another 1 month.
For the same purpose, phosphaden (AMP drug) is used, which regulates redox processes, has a vasodilating effect, has anti-aggregation properties and improves tissue trophism. At the onset of the disease, it is advisable to administer the drug intramuscularly at 0.25-1 ml of a 2% solution 2 times a day (for 2 weeks), then administer 1/2 - 1 tablet orally (1 tablet - 0.05 g) 2 -4 times a day (for 2 weeks) depending on the age and severity of the disease.
Previously, ATP was widely used for the same purpose. However, it has now been established that a large amount of energy is required for the penetration of ATP through cell membranes. This calls into question the role of ATP as an energy source for ensuring myocardial contractility and improving metabolic processes in it.
It has been established that the myocardium receives most of the required energy through beta-oxidation of fatty acids. Therefore, for non-rheumatic carditis, it is advisable to use carnitine chloride (carnicor, dolotin, etc.), which is a cofactor in the system that transports fatty acids across the inner mitochondrial membrane. The drug is prescribed as a 20% solution orally: for children under 1 year old - 0.03-0.075 g (4-10 drops) 3 times a day, from 1 year to 6 years - 0.1 g (14 drops) , from 6 to 12 years - 0.2-0.3 g (28-42 drops) 2-3 times a day. The duration of treatment is 4-8 weeks (with severe severity of the disease and the presence of heart failure).
Some researchers recommend using anabolic steroids to stimulate metabolism in the myocardium. It is advisable to prescribe these drugs to children with asthenia. Anabolic steroids (Nerobol, Retabolil) should be administered no earlier than 1.5-2 months from the onset of the disease to avoid exacerbation. The dose of Nerobol is 2-5 mg 2-3 times a day for 3 weeks, Retabolil 3-4 injections of 0.3-0.5 ml intramuscularly once every 3 weeks. Repeated courses after 4-6 months.
Therapy aimed at restoring impaired myocardial functions is purely symptomatic and depends on the specific manifestation of the disease. Cardiac glycosides, diuretics and antiarrhythmic drugs are used.
The main goal of therapy for all forms of carditis is to eliminate the symptoms of heart failure. To improve myocardial contractile function, cardiac glycosides are used, with preference given to digoxin. Only in case of development of pulmonary edema or pre-edema should strophanthin K or corglycon be used.
A saturation dose of digoxin (0.03-0.05 mg per 1 kg of body weight) is administered evenly over 3 days every 8 hours under ECG monitoring. If there is no saturation effect, the drug can be administered 3 times a day for 1-2 days. Such a slow administration of digoxin helps to avoid “intolerance” (intoxication), which occurs in patients with carditis with forced administration of the drug and its large doses. In mild to moderate cases of non-rheumatic carditis, digoxin is prescribed orally, and in severe cases - intramuscularly. Intravenous administration of glycosides is indicated in the most acute process with pulmonary edema.
After administration of a saturation dose of digoxin, a maintenance dose is used, the choice of which has its own characteristics. If the patient satisfactorily tolerates saturation with digoxin with a clear effect (normalization of heart rate, reduction of shortness of breath and reduction in liver size), then the maintenance dose is 1/5 of the saturation dose. If there is a tendency to bradycardia, the dose should be reduced to 1/6-1/8, and with constant tachycardia - increased to 1/4. A maintenance dose of digoxin is administered orally in two doses every 10-12 hours; if it is insufficiently effective, it is administered intramuscularly, and then orally.
The administration of glycosides should be careful, especially with anuria and oliguria. In such cases, treatment begins with diuretics (Lasix, intravenous furosemide) and, after diuresis is restored, cardiac glycosides are included. The selected effective dose of digoxin is used for a long time. The indication for discontinuation of the drug is the normalization of data from clinical and instrumental studies.
Diuretics are of great importance in the treatment of patients with acute carditis and heart failure. Depending on the stage of heart failure, the following plan for prescribing diuretics for carditis can be recommended: left ventricular failure stage 1-IIA - veroshpiron; left ventricular stage IIA + right ventricular stage IIA-B - oral furosemide and veroshpiron; total IIB-III - furosemide or lasix parenterally in combination with veroshpiron; if ineffective, brinaldix or uregit is administered. Doses of furosemide - 2-4 mg per 1 kg, veroshpiron - 1-4 mg per 1 kg, brinaldix and uregit - 1-2 mg per 1 kg of body weight. In order to increase diuresis in refractory heart failure, it is possible to prescribe aminophylline (0.1-0.2 ml per 1 kg of body weight, but not more than 3 ml of a 2.4% solution). In the hospital, diuretics are prescribed daily for 1 - 1.5 months. If left ventricular, and even more so total heart failure remains within stage IIA-B, then they continue to be used at home with a possible subsequent transition to taking them 2-3 times a week.
In patients with viral carditis, various heart rhythm disturbances are observed, which are caused by a disorder of the functions of automaticity, excitability and conductivity. Therefore, antiarrhythmic drugs are introduced into complex therapy, most often panangin (asparkam) and others.
2. Reasons
As the name obviously implies, the direct cause of inflammation in this case is the vital activity of pathogenic viruses, and the range of possible viral pathogens in this case is very wide (measles, enteroviruses, Coxsackie virus, rubella, etc.). A risk factor for congenital viral carditis, which can clinically manifest itself years later, is an infection suffered by the mother during pregnancy.
Penetrating into the structures of the myocardium, the virus multiplies in myocytes - cells that form the basis of the parenchymal muscle tissue of the heart. Myocytes die in this case; in addition, an immune response is triggered, and infected myocytes are destroyed by killer T cells and macrophages. In some cases, a dynamic balance is established between the virus and immune factors, and the disease becomes chronically recurrent and/or autoimmune in nature. The mechanisms of such “autoimmunization” have not been sufficiently studied to date.
But even if the immune system manages to completely suppress the activity of the pathogen, disturbances in the metabolism of proteins and nucleic acids persist in the myocardial tissue for a long time.
Visit our Cardiology page
Tests and diagnostics
There is a special rule: the more acute the process, the higher the nonspecific indicators will be, reflecting the course of the inflammatory process:
- C-reactive protein;
- ESR;
- alpha-2-globulin;
- leukocytosis;
- fibrinogen.
In carditis that occurs with minimal activity, an increase in the level of organ-specific enzymes is important in the differential diagnosis. Enzymes that are recorded in the blood during the death of a cardiomyocyte:
- lactate dehydrogenase (1 and 2 cathodic fractions);
- troponins (I or T);
- creatinine phosphokinase.
Today, the current diagnostic method is myocardial biopsy. This procedure is considered quite complicated and completely unsafe. Great importance is attached to the degree of sclerosis and the degree of lymphoid infiltration:
- granulomatous;
- eosinophilic;
- neutrophilic;
- giant cell.
The use of an injection of antimyosin antibodies during antimyosin scintigraphy makes it possible to identify inflammation of the heart muscle with high sensitivity. The sensitivity is 91-100%, but the specificity of the method is extremely low - only 31-40%. The extent and severity of cellular infiltration is determined by gallium scintigraphy.
The extent of the inflammatory process can be determined using magnetic resonance imaging with gadolinium (this method is under development).
General information
The frequency of non-rheumatic carditis per 100 thousand population is 110 cases. According to some data, 15% of patients who suffered from acute respiratory viral infections experienced symptoms of myocarditis . Carditis can occur at any age; much more often the disease affects young people and children. In adolescents and young men, a slight predominance of cases of the disease is recorded; in boys and girls, the frequency is almost the same. Non-rheumatic carditis is a lesion of the myocardial heart muscle; the lesion is based on a classic inflammatory process.
1.General information
Epicarditis, pericarditis, endocarditis - these terms summarize a large group of cardiovascular diseases in which certain membranes of the heart become inflamed. The etiology can be either infectious (the cause is viral or bacterial pathogens), or other - allergic, rheumatic, secondary (with any lesion and subsequent infection), or idiopathic, i.e. unidentified.
The term “viral carditis” thus indicates an infectious-inflammatory process in the membranes of the heart caused by viruses. There are no exact epidemiological data (estimates of incidence) regarding this pathology.
A must read! Help with treatment and hospitalization!
Diet for non-rheumatic carditis
Diet for heart failure
- Efficacy: therapeutic effect after 20 days
- Timing: constantly
- Cost of products: 1700-1800 rubles. in Week
Nutrition should be complete and meet age needs: limiting carbohydrates with acidic valences (pasta, cereals) and table salt in the acute period. Carbohydrates can be replenished with vegetables and fruits. When using glucocorticosteroids, foods high in animal protein, fruits and vegetables rich in potassium, dairy and other foods high in calcium are added to the diet. During the period of decompensation with the addition of edema, the drinking regime is sharply reduced by 200-300 ml per day (calculation is made taking into account the volume of daily urine). In severe cases of carditis, oxygen therapy .
Pathogenesis
The pathology is based on a genetically determined defect in antiviral immunity. In chronic and acute carditis, the pathogenesis differs.
In the acute form, the action of a certain triggering factor is important, namely an infectious agent, after exposure to which inflammatory factors ( histamine , bradykinin , prostaglandins , leukotrienes ) and an immediate reaction develops. Acute immune inflammation is most often caused by immune complexes and cytotoxic antibodies.
In the chronic form, the infectious agent as a pathogen has no significance. It is based on one’s own autoimmune reactions to delayed-type hypersensitivity, for example, with inferiority of the thymus gland and deficiency of suppressors. Cardiomyocytes are damaged as a result of autoimmune processes.
Forecast
The majority of patients with mild symptoms recover completely and subsequently show no signs of cardiac dysfunction. Every third patient develops a complication - dilated cardiomyopathy . The annual mortality rate from myocarditis with traditional treatment is 20%. In patients with an ejection fraction of less than 45% and symptoms of congestive heart failure, the 4-year mortality rate reaches 56%.