How to distinguish heart pain from others?
If unpleasant sensations appear in the area of the heart, pay attention to where it hurts, where it radiates, how exactly and for how long it hurts
.
Localization and irradiation of pain.
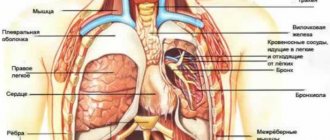
Heart pain occurs in the chest region and, as a rule, radiates to the left shoulder and left arm. Less commonly, it radiates to the jaw, upper wall of the stomach and to the area between the shoulder blades.
Duration and nature of pain.
An attack of heart pain lasts from 5 to 10 minutes. Most often it occurs after physical activity: before a trip, say, you loaded heavy bags into the trunk or changed a tire along the way. As for the nature of the sensations, the “prick” and “shot” are definitely not about the heart. Heart pain is pressing, burning. It is sometimes confused with heartburn. If something seems to be “gurgling and turning over” in your chest, it may be due to a heart rhythm disorder.
Cardiac dyspnea: causes of development and treatment methods
Shortness of breath is a sign of heart failure. They appear after lifting weights or doing physical exercise. In healthy people it is a temporary phenomenon, not a pathology. In patients with heart failure, shortness of breath is a frequent, obsessive symptom that varies in type, intensity and duration. As a rule, it is a sign that you need to take action and seek help from doctors.
Cardiac dyspnea, types
According to the classifier, cardiac dyspnea has a 4-stage course.
- Stage 1 – low-intensity, unnoticeable.
- Stage 2 with the appearance of increasing shortness of breath during intense physical activity.
- Stage 3 with the appearance of unpleasant symptoms even at rest, with moderate loads.
- 4 – severe stage with disturbing shortness of breath at night in a supine position, when blood flow to the heart is increased, which clearly indicates heart failure, stagnation of blood in the vessels and lungs.
There are 2 types of cardiac dyspnea.
- Physiological shortness of breath during exertion, excessive physical activity, but quickly passing when a person is at rest.
- Pathological, as a consequence of diseases of the cardiovascular system, changes in the depth and frequency of breathing. The patient begins to breathe rapidly, swallowing air, but does not feel complete satisfaction. Hypoxia and oxygen starvation develop.
Shortness of breath and weakness become obsessive phenomena during the course of chronic heart failure. Spasms of small halos and failure of heart function occur against the background of increased pressure in the lungs. The condition begins to negatively affect peripheral circulation, leading to a decrease in oxygen saturation or a complete cessation of oxygen supply to the brain.
8
24/7
A feature of CHF in patients is the appearance of shortness of breath even at rest. Additional signs:
- blueness of lips, lower extremities;
- cough;
- swelling on the face.
Symptoms intensify at night against the background of redistribution of blood from the peritoneal cavity and lower extremities to the chest and creating excessive stress on the heart, specifically in a supine position.
Complications of chronic heart failure:
- pulmonary edema, bronchospasm, signs of suffocation in case of fluid accumulation and blood stagnation, blockage of the airway;
- multiple organ failure or Cheyne-Stokes, when breathing periodically increases or becomes intermittent.
4th degree of cardiac shortness of breath, pain in the heart - a serious condition. The patient is forced to take a sitting position to reduce the symptoms of attacks and the load on the heart. Breathing becomes intermittent and uneven. Oxygen starvation and brain asphyxia are harbingers of stroke and heart attack.
Risk factors
The risk group includes elderly people, or those diagnosed with congenital heart disease or mitral valve prolapse.
Cardiac dyspnea can be provoked by:
- left heart failure;
- congestion in the lungs;
- decreased cardiac output;
- psychovegetative factors: fear, anxiety, neuroses, depression, excitement;
- disorders of the autonomic system.
Causes
The main causes of occurrence are physiological or cardiac:
- lifting weights;
- climbing stairs;
- grueling runs over long distances;
- excessive sweating;
- VSD, psychovegetative syndrome during vegetative-vascular crisis;
- obesity with a feeling of suffocation and lack of oxygen;
- tachypnea, shallow rapid breathing due to complications of a viral infection the day before;
- deformation, curvature of the spine;
- scoliosis of the chest;
- anemia;
- pregnancy (3rd trimester) as the load on the heart and the body as a whole increases;
- cardiopathy;
- cardiac ischemia;
- narrowing of the mitral valve (stenosis);
- arterial hypertension;
- acquired (congenital) heart defect;
- myocardial infarction.
8
24/7
Symptoms
Cardiac shortness of breath is a sign of circulatory failure, irritation of the respiratory center, and the development of heart failure. If you ignore and do not consult a doctor, you can expect:
- decreased oxygen supply to the blood;
- violation of pulmonary ventilation;
- development of tissue hypoxia, oxygen starvation;
- attacks of arrhythmia, tachycardia, angina pectoris.
The main symptom of cardiac dyspnea is difficulty in inhaling, first after physical exertion, and over time - at rest, in a supine position. Additional signs:
- wheezing in the lungs;
- chilly hands;
- swelling of the legs, increasing in the evening;
- increased heart rate.
Heart failure is characterized by arthopnea (shortness of breath in the lying position) or a paroxysmal form of development in severe disease with the appearance of signs:
- paroxysmal cough with discharge of foamy (transparent) sputum and cold sweat;
- cyanosis of the skin;
- weakness;
- brokenness.
Signs indicate stagnation of blood in the pulmonary circulation, swelling of the mucous membrane, effusion of fluid from the vessel into the lumen of the pulmonary alveoli.
Diagnostics
A cardiologist can recognize the true causes of shortness of breath, and you should turn to him for help and treatment.
Help: Pulmonary and cardiac dyspnea are different symptoms. In pulmonary cases, phlegm accumulates in the lungs; in cardiac cases, blood circulation in the pulmonary circulation is disrupted.
The task of doctors is to identify the primary causes of the manifestation and listen to complaints of shortness of breath in patients. Diagnosis is differential. Methods:
- EchoCG;
- isotope ventriculography: a study that reveals the measurement of blood fractions during emissions during the patient’s physical activity or while at rest;
- coronary angiography;
- chest x-ray;
- electrocardiogram.
It is important to create a complete picture of the disease and identify possible damage to the vessel in order to develop the correct treatment tactics.
Treatment at different stages
If breathing is shallow due to ARVI or influenza, which often happens in children, then the condition normalizes as the incubation period of the underlying disease passes. But the insidiousness of viral infections is complications, the transition of the inflammatory process to the bronchi, which leads to breathing problems, bronchospasms, shortness of breath, and wheezing.
If shortness of breath occurs when walking and is caused by respiratory failure, then the main goal is to reduce the load on the heart and expand the bronchial ducts to remove accumulated mucus.
Medicines:
- methylxanthines (Eufillin);
- anticholinergics (Platifillin);
- antihistamines (Fenistil, Pipolfen, Claritin);
- antispasmodics (No-Shpa);
- anticholinergics (Berodual, Atrovent);
- adrenomimetics (Clenbuterol, Salbutamol);
- glucocorticoids in inhalations;
- glycosides (Digoxin, Korglykon);
- ACE inhibitors for the prevention of heart failure;
- diuretics (Furosemide) to reduce the load on the cardiovascular system.
If laryngospasms are detected in children with the appearance of shortness of breath, as a complication of influenza infection (bronchitis), leading to impaired respiratory functions, then gentle therapy is prescribed:
- mustard plasters;
- anticholinergics (Platifillin);
- drugs for thinning sputum (ACC, Ambroxol, Mucaltin, Bromhexine);
- diuretics (Hypothiazide, Veroshpiron, Furosemide, Diacarb) to reduce congestion;
- calcium antagonists (Nitrosorbide, Captopril) in the treatment of pulmonary hypertension;
- expectorants to reduce the load on the heart, dilate the bronchi, relieve shortness of breath.
Additionally, oxygen therapy is carried out by supplying humidified oxygen to regulate respiratory functions. Patients are recommended breathing exercises and physiotherapy.
It is important to understand that cardiac dyspnea is a symptom. Treatment should be aimed at eliminating the underlying causes that led to the condition. If it is not possible to compensate for heart failure and eliminate shortness of breath with medications, then surgery to install a pacemaker, transplant the ventricles of the heart, and eliminate valve defects is indicated.
Surgical methods are not used if shortness of breath is a temporary phenomenon, and disturbances in the cardiovascular system after diagnosis are minor.
Complications
Chronic heart failure (CHF) is dangerous when gas exchange and metabolism are impaired. If the underlying disease is not treated at an early stage, shortness of breath will become a constant concern and lead to complications:
- cardiac cardiac asthma with attacks of suffocation;
- feeling of lack of air;
- drop in blood pressure;
- swelling in the lungs.
As pressure increases in the pulmonary vessels and pulmonary circulation, the following are observed:
- attacks of suffocation;
- bubbling in the region of the heart;
- swelling of the pericardial veins;
- cold sweat;
- emphysema due to congestion in the pulmonary circulation;
- pneumosclerosis due to decreased elasticity of blood vessels and tissues in the lungs;
- cyanosis;
- suffocation, coughing at night;
- hemoptysis;
- luminal obstruction, pulmonary embolism.
Forecast
Shortness of breath is not an independent disease, but a sign of cardiac pathology and impaired gas exchange in the lungs. It is impossible to get rid of shortness of breath until the underlying disease is cured. Cardiac pathology leads to mortality in the case of dystrophic changes in 60% of patients. It is possible to compensate for deficiency and prolong life at the initial stages of development.
Disease prevention
Cardiac dyspnea is associated with impaired cardiac function. Pathology can be avoided if:
- lead a healthy lifestyle;
- to refuse from bad habits;
- move more, walk in the fresh air;
- eliminate stress, nervousness, overexertion;
- dose physical activity;
- limit your intake of table salt;
- keep blood pressure levels under control;
- ventilate the room more often;
- raise the head of the bed by 5° so that your head rises slightly during sleep;
- do not delay diagnosis or go to the doctors if shortness of breath has become an obsessive phenomenon even at rest.
Heart failure and pulmonary edema are complex diseases with negative consequences. If shortness of breath appears at rest, this is a signal that it is no longer possible to remain idle. You need to make an appointment with a doctor and undergo a full diagnosis so that the specialist can draw up an effective treatment plan.
8
24/7
Pain in the heart area. note
Heart pain is one of the most common reasons people seek emergency care. So, every year, several million people seek emergency medical help with this symptom.
Pain in the heart area is not always pain in the heart. Often it is not associated with heart problems. However, if you are experiencing chest pain and are not aware of the state of your cardiovascular system, the problem may be serious and it is worth taking the time to find out the cause of the pain.
Causes
Pain in the heart area can be very different. It is not always possible to describe it. The pain can be felt as a mild burning sensation or as a severe blow. Since you cannot always determine the cause of pain on your own, there is no need to waste time on self-medication, especially if you belong to the so-called “risk group” for heart disease.
Pain in the heart area has many causes, including those that require close attention. The causes of pain can be divided into 2 large categories - “cardiac” and “non-cardiac”.
"Heart" reasons
(Tegiocardial infarction - a blood clot that blocks the movement of blood in the arteries of the heart can cause pressing, squeezing pain in the chest that lasts more than a few minutes. The pain can radiate to the back, neck, lower jaw, shoulders and arms (especially the left). Other symptoms may include shortness of breath, cold sweats, and nausea.
(Angina pectoris Over the years, fatty plaques can form in the arteries of your heart, restricting the flow of blood to the heart muscle, especially during exercise. It is the restriction of blood flow through the arteries of the heart that causes attacks of chest pain - angina. Angina pectoris is often described by people as a feeling of pressure or squeezing in the chest. It usually occurs during exercise or stress. The pain usually lasts about a minute and stops with rest.
Other cardiac causes. Other causes of chest pain include inflammation of the lining of the heart (pericarditis), most often due to a viral infection. Pain with pericarditis is most often acute, stabbing in nature. Fever and malaise may also occur. Less commonly, the pain may be caused by a dissection of the aorta, the main artery in your body. The inner layer of this artery can separate under blood pressure and the result is sharp, sudden and severe pain in the chest. Aortic dissection can be the result of chest trauma or a complication of uncontrolled hypertension.
"Non-heart" reasons
Heartburn. Acidic stomach acid that flows from the stomach into the esophagus (the tube that connects the mouth to the stomach) can cause heartburn, a painful burning sensation in the chest. It is often combined with a sour taste and belching. Heartburn chest pain is usually associated with food intake and can last for hours. This symptom most often occurs when bending or lying down. Taking antacids relieves heartburn.
Panic attacks. If you experience attacks of unreasonable fear, combined with chest pain, rapid heartbeat, hyperventilation (rapid breathing) and profuse sweating, you may be suffering from “panic attacks” - a unique form of dysfunction of the autonomic nervous system. Pleurisy. Sharp, localized chest pain that gets worse when you inhale or cough may be a sign of pleurisy. The pain occurs due to inflammation of the membrane lining the inside of the chest cavity and covering the lungs. Pleurisy can occur with various diseases, but most often with pneumonia.
Tietze syndrome. Under certain conditions, the cartilaginous parts of the ribs, especially the cartilage that attaches to the sternum, can become inflamed. Pain in this disease can occur suddenly and be quite intense, simulating an attack of angina. However, the location of pain may vary. With Tietze syndrome, pain may increase when pressure is placed on the sternum or ribs near the sternum. Pain during angina pectoris and myocardial infarction does not depend on this.
Osteochondrosis of the cervical and thoracic spine leads to so-called vertebrogenic cardialgia, which resembles angina pectoris. In this condition, there is intense and prolonged pain behind the sternum, in the left half of the chest. Irradiation to the arms and interscapular area may be observed. The pain increases or decreases with changes in body position, head turns, and arm movements. The diagnosis can be confirmed by performing an MRI of the spine.
Pulmonary embolism. This type of embolism occurs when a blood clot enters the pulmonary artery, blocking the flow of blood to the heart. Symptoms of this life-threatening condition may include sudden, sharp chest pain that occurs or gets worse with deep breathing or coughing. Other symptoms are shortness of breath, palpitations, anxiety, loss of consciousness.
Other lung diseases. Pneumothorax (collapsed lung), high pressure in the blood vessels supplying the lungs (pulmonary hypertension), and severe asthma may also cause chest pain. Muscle diseases. Pain caused by muscle diseases usually begins to bother you when you turn your body or raise your arms. Chronic pain syndrome such as fibromyalgia. May cause persistent chest pain.
Damage to ribs and pinched nerves. Bruises and fractures of the ribs, as well as pinched nerve roots, can cause pain, sometimes very severe. With intercostal neuralgia, pain is localized along the intercostal spaces and intensifies with palpation.
Diseases of the esophagus. Some diseases of the esophagus can cause difficulty swallowing and therefore chest discomfort. Esophageal spasm can cause chest pain. In patients with this disease, the muscles that normally move food down the esophagus work uncoordinated. Since esophageal spasm can resolve after taking nitroglycerin - just like angina - diagnostic errors often occur. Another swallowing disorder known as achalasia can also cause chest pain. In this case, the valve in the lower third of the esophagus does not open as it should and does not allow food to pass into the stomach. It remains in the esophagus, causing discomfort, pain and heartburn.
Shingles. This infection, caused by the herpes virus and affecting the nerve endings, can cause severe chest pain. The pain can be localized in the left half of the chest or be of a girdling nature. This disease can leave behind a complication - postherpetic neuralgia, which causes prolonged pain and increased skin sensitivity.
Diseases of the gallbladder and pancreas. Gallstones or inflammation of the gallbladder (cholecystitis) and pancreas (pancreatitis) can cause pain in the upper abdomen that radiates to the heart. Because chest pain can have many different causes, do not self-diagnose, self-medicate, or ignore severe or prolonged pain. The cause of your pain may not be so serious - but in order to establish it, you need to contact a specialist.
When should you see a doctor?
If you experience sharp, unexplained, long-lasting chest pain, perhaps in combination with other symptoms (such as shortness of breath) or pain that radiates to one or both arms. Under the shoulder blade - you need to urgently consult a doctor. Perhaps this will save your life or calm you down if no serious problems with your health are found.
Diagnostics
Pain in the heart area does not always indicate heart disease. Tests that can help determine the cause of pain include: (Electrocardiography (ECG)) This test helps your doctor diagnose heart disease. It records the electrical activity of the heart through electrodes placed on the skin. Heart impulses are recorded as "waves". Because damaged heart muscle cannot conduct electrical impulses normally, an ECG may show that the patient has heart disease.
Blood tests. Your doctor may order tests to look for elevated levels of certain enzymes. Damage to heart cells during myocardial infarction leads to the release of these enzymes and their entry into the bloodstream. Myocardial scintigraphy. This method helps doctors determine the “heart cause” of pain, for example. Narrowing of the coronary arteries. A small amount of a radioactive substance (such as thallium) is injected into the bloodstream. Special cameras capture the radioactive substance and track its passage through the heart and lungs.
(Angiography) This test helps to see the arteries of the heart and any obstructions in them. A liquid contrast agent is injected into the arteries of the heart through a special catheter - a long, hollow tube that is passed to the heart through an artery (usually the femoral one). X-rays make the arteries visible. (Echocardiography (ECHO CG)) This method uses ultrasound waves to obtain an image of the beating heart.
Electron beam tomography (CRT). This unique method allows, by identifying microcalcifications in the wall of the coronary arteries, to detect the early stages of the development of coronary heart disease even before symptoms appear.
Magnetic resonance imaging of the spine will help determine the cause of pain in the chest if it is caused by pinched nerve roots or the presence of herniated intervertebral discs.
*Materials from the website www.corallcenter.ru
“Fuzzy head” is one of the main signs of astheno-neurotic syndrome
If “fuzzy head”, “cloudy head” is the feeling with which you get up and lie down, and if increased irritability, fatigue and poor sleep are added to this, most likely we are talking about astheno-neurotic syndrome
.
Main symptoms:
Many people complain of “fog in the head”, “head like cotton wool”, “fuzzy head” and similar symptoms.
If you notice fatigue, sleep disturbances, and constant irritability, then you may have a mental disorder called astheno-neurotic syndrome.
Prevalence:
This disease is one of the most common “diseases of civilization.” It is often called "managers' flu."
Educated and successful people are susceptible to the disease. The most typical age is from 20 to 40 years. These are entrepreneurs, managers, doctors, teachers. People whose work involves increased responsibility, such as air traffic controllers, are at particular risk.
In the past, astheno-neurotic syndrome was called “nervous exhaustion”
Creative individuals are also at risk.
Causes:
The main causes are stress, prolonged nervous excitement, chronic lack of sleep, and constant overwork. Also factors contributing to the occurrence of astheno-neurotic syndrome are previous diseases, including colds, some viruses, poisoning, and poor environmental conditions.
Similar symptoms:
What diseases can manifest themselves as “foggy head”, poor sleep, weakness and irritability, except neurasthenia? First of all, these are asthenic conditions with the onset of serious illnesses. The second is masked depression, which at the beginning can easily be confused with astheno-neurotic syndrome. And chronic fatigue syndrome can manifest itself in a similar way.
So only a psychotherapist or psychiatrist can make a correct diagnosis. To make a diagnosis, professional psychological diagnostics (psychotests) are usually used, which you can take yourself (follow this link).
How the disease develops:
The syndrome occurs gradually, with a combination of emotional and physical stress, constant fatigue. Most often, patients complain of loss of strength, general weakness, increased irritability, “fog” in the head, and inability to cope with normal amounts of work.
If a person continues to be exposed to stress and does not seek medical help, his condition worsens - the usual set of complaints about a “cotton” head is joined by tearfulness, complaints about the heart, and fog in the head. Irritability increases to an extreme degree, but irritation quickly gives way to weakness. Sleep is usually unstable, does not bring a feeling of rest, and after sleep the head feels like cotton wool. Appetite worsens, constipation or diarrhea may bother you. Sexual desire decreases in both men and women. The condition worsens before a change in weather (so-called “meteosensitivity”). In the absence of treatment at this stage, apathy, lethargy, severe weakness and persistent depression of mood are further added. Interest in life decreases, the patient thinks only about his painful condition, about his “fuzzy” head.
Left untreated, psychotic disorders may develop.
Treatment:
The prospects for treatment are positive; usually psychotherapeutic methods give excellent results, including complete recovery. In severe cases, a combination of psychotherapy and psychopharmacotherapy is used.
Self-medication usually worsens the condition and leads to progression of the disease.
At the initial stage of the disease, in order to make a correct diagnosis, a psychotherapist needs to exclude all diseases that exhibit similar symptoms, because the more accurate the diagnosis, the more successful the treatment will be.
Different diseases with similar symptoms must be treated differently. Therefore, you should definitely consult a psychotherapist. A good psychotherapist selects therapy that matches the specific manifestations of the disease and the individual characteristics of each patient.
Astheno-neurotic syndrome is one of the most common “diseases of civilization.” It is often called "managers' flu."
Treatment of the syndrome depends on the severity of painful symptoms, but is primarily aimed at eliminating psychotraumatic factors. It is necessary to reduce both mental and physical stress. This is the most important condition for treatment; without such measures it will not be possible to defeat the disease. In the early stages of the disease, normalizing the rhythm of life, eliminating stress and psychotherapy may be enough to significantly improve health. And, of course, at this stage, psychotherapy methods that do not use drugs - cognitive-behavioral, psychoanalysis - have a very good effect, and group psychotherapy methods are very effective.
In any case, you need to see a psychotherapist.
In more advanced cases, additional psychopharmacotherapy may be required. General strengthening drugs, tranquilizers, and, if necessary, sleeping pills and antidepressants are used. Psychotherapy is also actively used in the treatment of advanced astheno-neurotic syndrome.
The first indicator of improvement is the normalization of sleep and the disappearance of the feeling of “fog” in the head. With timely treatment, the problem can usually be completely overcome, however, if the tense environment and stress at work and in personal life continue to persist, various complications are possible.
Terminology and other names:
In the past, astheno-neurotic syndrome, together with diseases of similar symptoms, was called “nervous exhaustion.”
In modern psychiatry, the term “neurasthenia” is more often used to refer to neuro-asthenic syndrome (synonyms). In the everyday sense, neurasthenia is usually perceived as a painful, nervous, unbalanced state, characteristic of weak-willed people, easily susceptible to various influences and moods, and in a state of acute mental crisis. And in the medical sense, this is a state of depression, irritability, “fuzzy head.”
Intercostal neuralgia: symptoms, diagnosis and treatment
Chest pain is always alarming. As a rule, the first thing a person thinks about is the heart. Statistics, widely revealed thanks to the media, also echo such fears: deaths from cardiovascular diseases confidently remain at the top of the sad list.
However, it is not only the heart that can hurt in the chest. Natalya Vladimirovna Umerenkova, a neurologist and leading specialist in the neurology department at the Expert Clinic Kursk, told us about intercostal neuralgia, one of the symptoms of which is chest pain.
— Unexpected chest pain is always alarming. What can hurt your chest?
Such pain is a signal for both the doctor and the patient. Many anatomical structures can hurt in this area. This is the heart in case of ischemic disease (angina pectoris, heart attack), large vessels (in case of dissecting aortic aneurysm). Pain occurs with tracheitis, pneumonia, accumulation of air in the pleural cavity (pneumothorax) and its inflammation, tumors of the lungs and mediastinal organs, pulmonary embolism, mediastinitis, pathology of the esophagus (inflammation, peptic ulcer).
You can read about the symptoms, diagnosis and treatment of pneumonia here
Pain can also be “reflected” into the chest when the pancreas, gall bladder, or stomach pathology are affected (peptic ulcer).
Sometimes pain can be of a psychogenic nature - for example, with an imbalance of the autonomic nervous system (also known as vegetative-vascular dystonia).
Vegetative-vascular dystonia - diagnosis or fiction? Read here
Accompanied by chest pain and diseases of the osteochondral structures of the chest and nerve trunks - including intercostal neuralgia.
— How do you understand that chest pain is threatening and an ambulance should be called immediately?
Here it is important not to miss, in particular, such pathologies as unstable angina, myocardial infarction, pulmonary embolism, and thoracic aortic aneurysm.
For this group of diseases there are common manifestations - “alarm signals” that you should definitely pay attention to. This is most often a fairly severe, acute pain, which differs from the pain noted earlier (if it was noted), and does not go away while taking nitrates. The pain may be accompanied by nausea, vomiting, sweating, and pale or bluish skin. Rapid heartbeat often develops, shortness of breath, suffocation, hemoptysis, drop in blood pressure, pre-syncope or fainting are possible. These signs are a reason to immediately call an ambulance.
— What is intercostal neuralgia?
Intercostal neuralgia is a complex of manifestations that develops when the intercostal nerve or nerves are irritated or compressed. There are doctors who regard it as an independent disease with a clearly defined picture, while others consider it a syndrome that can be caused by a variety of disorders. In any case, intercostal neuralgia is coded in ICD 10 (code G58.0).
— What kind of pain occurs with intercostal neuralgia? By what signs can it be distinguished from other pain?
Intercostal neuralgia is often characterized by a unilateral location of pain (right or left), which is semi-encircling in nature. The patient can describe it quite clearly, i.e. indicate its location, the course of distribution (usually along the intercostal space).
The pain is quite acute, can be constant (with periods of worsening) or paroxysmal. Longer than that with stable angina (with the latter, the pain usually goes away after 3-5 minutes at rest).
Pain with intercostal neuralgia has periods of worsening/improving, is quite clearly associated with physical activity, changes in body position, and can be provoked by coughing, sneezing, or deep breathing. In addition to pain, symptoms such as numbness, burning, pulsation, and involuntary muscle contraction are often encountered in the intercostal space.
The difference between pain in intercostal neuralgia and cardiac pain (in particular angina) also lies in the absence of irradiation to the left arm and lower jaw; no fluctuations in blood pressure; The duration of the pain syndrome also differs (with neuralgia, pain can be bothersome for a long time), there is no effect from taking nitrates, there are no symptoms signaling a serious pathology of the heart and blood vessels. The provoking factors in the occurrence of pain also differ (awkward movement and a deep breath can trigger an attack of pain with intercostal neuralgia); Adopting a pain-relieving position minimizes it in case of intercostal neuralgia, but does not affect the intensity of “heart” pain.
How to avoid running to a hospital bed? What do you need to know about health before buying a gym membership? Read more
— Can there be an increased body temperature with intercostal neuralgia?
No. If such a manifestation occurs, you need to look for another cause of pain in the chest.
— Why does intercostal neuralgia occur?
The mechanisms leading to intercostal neuralgia may be irritation or compression of the intercostal nerve. This may be due to osteochondrosis of the spine, curvature of the spinal axis, spondylosis, damage to the transverse costal joints; after injury to the ribs and chest, excessive muscle tension (in particular intercostal muscles); with excessive mobility of parts of the ribs on the lateral and anterior surface of the chest; Infringement of the 7th-12th nerves in the connective tissue sheaths of the rectus abdominis muscle is less common.
Does osteochondrosis exist? Find out here
Sometimes the cause of intercostal neuralgia can be the herpes zoster virus. In this case, it is coded in a different section of ICD-10, but the manifestations will be generally the same.
In some cases, intercostal neuralgia can occur after suffering from influenza and a number of infectious diseases.
Additional risk factors for the occurrence of intercostal neuralgia may include diabetes mellitus, alcoholism, and impaired absorption of B vitamins.
“Triggering” moments can be a combination of factors: hypothermia, sudden and/or awkward movement, interventions on the thoracic spine (not entirely correct manual therapy, surgery, etc.).
— Can intercostal neuralgia go away on its own or does it need to be treated?
Sometimes it can go away on its own. However, in the absence of treatment, it is likely that the duration of the disease and the treatment time will increase (with therapy, the period of temporary disability is usually 7-14 days), and the process may become chronic, when the pain can last for weeks, and in the case of the herpetic nature of the disease - for months and years.
The question is also that during self-diagnosis, i.e. when the patient decided that he had intercostal neuralgia and did not go to the doctor to prescribe treatment, you can “miss” some other, often serious, diagnosis that resembles neuralgia in its manifestations. At the same time, the consequences without treatment may not be so harmless, and, in addition, time will be lost.
— What is the risk of intercostal neuralgia if it is not treated? How dangerous is this diagnosis?
If left untreated, recovery time may increase or the pain may become chronic.
— Which doctor should you contact for symptoms of neuralgia?
Since intercostal neuralgia can be confused with much more serious, life-threatening diseases, you should first immediately consult a physician or general practitioner. And only after excluding these pathologies, see a neurologist.
You can make an appointment with a therapist here
Please note: consultations are not available in all cities
Occasionally, when there is a need for therapeutic blockades, the help of a neurosurgeon or traumatologist may be needed.
— How is intercostal neuralgia diagnosed?
An ECG and chest x-ray are required, and body temperature is measured.
Are x-rays dangerous? Yulia Aleksandrovna Rutskaya, head of the radiation diagnostics department, tells
"Clinics Expert Kursk"
According to indications - radiography or MRI with myelography of the thoracic spine. Sometimes tests are prescribed to confirm/exclude an acute inflammatory process.
— What should you never do if you have intercostal neuralgia? For example, is it possible to warm the area of pain with a heating pad? Exercise? Go to the bathhouse?
None of the above.
— What is the prognosis for this disease? Is intercostal neuralgia successfully treated?
With correct diagnosis and timely treatment, the prognosis is favorable. This pathology is highly treatable.
— What needs to be done to prevent the development of intercostal neuralgia?
For prevention, it is necessary to avoid hypothermia, sudden and awkward movements (especially if they are unfamiliar, insufficient training or “warming up” before training; within the framework of the work performed); optimize body position in the workplace; engage in physical therapy; undergo regular medical examinations; do not hesitate to consult a doctor if any health symptoms appear.
For reference:
Umerenkova Natalya Vladimirovna
In 2004 she graduated from Kursk State Medical University.
In 2004-2005, she completed an internship in neurology at the above-mentioned university.
Since 2015, he has been working at Clinic Expert Kursk LLC, and is a leading specialist in the neurology department. Receives at the address: st. Karl Liebknechta, 7
Reasons for appearance
The pain may occur intermittently. Sometimes it is a regular spasm, and in some cases it is attacks of pain. Also, unpleasant feelings can begin during inhalation and exhalation, sudden body movements, such as coughing or sneezing. Doctors distinguish between primary and secondary causes of intercostal neuralgia.
Primary:
- problems with the spine. This may be loss of elasticity of the intervertebral discs, infection or inflammation in the roots and joints of the vertebra;
- incorrect posture. Also one of the primary reasons, it occurs in most people who lead an inactive lifestyle, constantly sit in one position, and slouch;
- rib fractures. This includes deformation of the thoracic region, its pathology or tumor.
Secondary causes include:
- hypothermia of the human body;
- long periods of sitting in drafts;
- infectious diseases associated with the lungs: pneumonia, tracheobronchitis;
- heart disease: myocardial infarction, ischemia, dissecting aortic aneurysm;
- problems with the mammary glands in women, such as swelling or inflammation;
- improper functioning of the gastrointestinal tract. For example, peptic ulcer, pancreatitis.
But the main and most common cause of intercostal neurosis is stress. People who are constantly stressed experience stiffness in their movements and muscle spasms. That is why any sudden movement causes pain and can provoke intercostal neuralgia.