Addison's disease - what is it?
Photos of Addison Birmer's disease usually show thin people with a pained expression on their faces.
The type of patients directly depends on the degree of insufficiency of adrenal hormones. Pathology is more common in middle age (between 20 and 40 years). Characterized by a progressive severe course. It is diagnosed equally in both men and women.
Forms of Addison's disease
Based on the causative factor, Addison's disease is classified into:
- primary failure (more than 95% of the cells of the cortex that produce hormones are destroyed);
- secondary and tertiary failure (due to the pituitary gland/hypothalamus, there is a deficiency of hormones that stimulate adrenal function);
- Iatrogenic failure (develops as a result of discontinuation of glucocorticoids after prolonged use).
According to the time criterion, Addison's disease can occur in two forms:
- acute (the adrenal cortex is quickly destroyed due to hemorrhage, surgical treatment, trauma);
- chronic (the result of autoimmune damage, tuberculosis).
Classification
Depending on the mechanism of development of Addison's or otherwise bronze disease, the following are distinguished:
- primary insufficiency of the adrenal cortex - the basis of the pathology is damage to the glandular structures directly;
- secondary failure - as a result of a violation of the hypothalamic-pituitary system , which normally should stimulate the adrenal cortex.
Acute adrenal insufficiency is called hypoadrenal or Addison's crisis .
Features of Addisonian crisis
Addisonian crisis develops suddenly and can threaten a person’s life. Low concentrations of hormones (cortisol, aldosterone) in the bloodstream lead to loss of consciousness or psychosis, confusion, delirium, fever , severe vomiting and diarrhea , mineral and water imbalances, pain in the legs, lower back, abdomen, low blood pressure and even cause shock .
Addison's disease - causes
Doctors identify the following causes of Addison's disease:
- autoimmune damage to the adrenal glands (the body begins to produce antibodies against its own tissues);
- congenital genetic diseases (for example, autoimmune polyglandular syndrome type 1);
- metastasizing tumors (breast cancer, lung cancer);
- tuberculosis of the adrenal glands (infection can be introduced from the bones, lungs, kidneys);
- removal of the adrenal glands due to the occurrence of tumor tumors;
- tumors of the hypothalamic-pituitary region;
- irradiation/removal of the pituitary gland for cancer;
- long-term use of glucocorticosteroids, which inhibits the functions of the adrenal cortex;
- necrosis of the adrenal glands at the last stage of HIV, with scarlet fever, complicated by influenza;
- uncontrolled use of cytostatics, causing toxic damage to the adrenal glands.
Tests and diagnostics
To confirm Addison's disease you need to do:
- ultrasound examination of the adrenal glands to identify lesions, for example in tuberculosis ;
- blood test to determine the level of adrenal hormones (cortisol), ACTH, glucose, potassium, sodium, renin ;
- CT scan of the adrenal glands, which allows you to detect adrenal infarction, reduction in size, tumor metastases, amyloidosis;
- MRI of the brain to study the hypothalamic-pituitary region and detect destructive, tumor or granulomatous processes.
The basis for diagnosing Addisonian crisis is:
- a decrease in sodium concentration in the bloodstream below 130 mmol/l, excretion in urine - less than 10 g per day;
- an increase in potassium concentration in the bloodstream over 5 mmol/l;
- a drop in the ratio of sodium to potassium ions to 20 units (normally 32);
- low glucose levels;
- development of acidosis;
- high concentrations of urea , residual nitrogen in blood plasma tests.
Addison Birmer's disease - symptoms
Signs of Addison Birmer's disease vary.
Skin and mucous membranes
From the mucous membranes and skin the following are observed:
- decreased elasticity;
- thinning of the skin;
- pallor;
- the appearance of pigmentation first in open areas, later in the folds of the skin (the greatest darkening is diagnosed on the lips, in the perineum, near the nipples).
Changes in skin color in Addison's disease are explained by the release of large amounts of adrenocorticotropic hormone, which normally stimulates the adrenal glands. Since this hormone is similar in structure to melanostimulating (increases pigmentation in melanocytes), its excess leads to the skin becoming brown or dark brown. Spots of unusual color often form on the gums and the inner surface of the cheeks.
Reproductive system and sexual desire
From the reproductive system, Addison's disease is manifested by the following symptoms:
- Cessation of monthly menstrual flow in women, dry skin, decreased elasticity. Hair loss in the pubic bone and armpits.
- Impotence and decreased libido in men.
These symptoms are explained by the fact that the adrenal cortex synthesizes sex hormones that affect the development and functioning of the genital organs and are responsible for sexual function in both sexes.
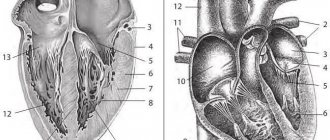
The cardiovascular system
From the side of the cardiovascular system, Addison Birmer's disease reveals:
- Violation of the heart rhythm, failure of the transmission of nerve impulses that contribute to the contraction of the heart muscle. These signs are due to the fact that potassium ions accumulate in myocardial and blood cells. Sodium ions, on the contrary, are intensively excreted in the urine. Due to the imbalance of these elements, both the heart rhythm and nerve transmission in other organs are disrupted.
- Decreased heart rate and strength. If Addison's disease is diagnosed in children, then it is pointless to expect that the heart will develop normally. In the future, the patient may even show signs of cardiovascular failure, swelling of the lower extremities, pallor and decreased skin temperature.
- Hypotension. Blood pressure in patients decreases due to increased excretion of sodium ions in the urine. This process provokes dehydration of the body. Along with weak heart contractions, the tone of blood vessels is significantly reduced. Arterial hypotension develops.
Gastrointestinal tract
In Addison-Biermer disease, the metabolic rate decreases. As a consequence, insufficiency of the function of the secretory glands of the intestines and stomach occurs. Over time, the villi of the gastrointestinal mucosa begin to die, and normal absorption of nutrients becomes impossible. This is fraught with:
- vomiting, nausea, diarrhea (signs of adrenal hormone deficiency);
- stomach and duodenal ulcers;
- hypoacid gastritis (the mucous membrane of the stomach becomes inflamed, the production of pepsin and hydrochloric acid, necessary for high-quality digestion of food, decreases).
Other organs and systems
Addison's disease is associated with dehydration. The fact is that regulation of water-salt metabolism is impossible without aldosterone. If there is a shortage of it, chlorine and sodium ions are quickly removed from the body along with the liquid. Blood pressure drops, the skin becomes very dry, the cheeks and area around the eyes become hollow. The stomach is drawn in. But most of all, dehydration affects the central nervous system and brain:
- Severe neurological disorders occur. The patient becomes very lethargic and passive. He reacts poorly to external stimuli. Delayed treatment can cause coma, seizures and death. Mental disorders in Addison's disease cannot be excluded.
- The transmission of nerve impulses is disrupted. Sensitivity is upset, numbness of the limbs and severe muscle weakness occur.
Due to lack of fluid, the blood becomes thick and circulation is impaired. The blood supply to peripheral organs deteriorates. Blood clots may form. The amount of urine produced also decreases.
Addison's disease also affects the immune system. The patient easily becomes infected with infectious diseases, often suffers from pneumonia and bronchitis.
If you notice similar symptoms, consult a doctor immediately. It is easier to prevent a disease than to deal with the consequences.
Anemia is a clinical and hematological syndrome characterized by a decrease in the concentration of hemoglobin per unit volume of blood. Anemia affects the population of both underdeveloped and economically developed countries. It develops in people of any age, but children and pregnant women suffer from it much more often [1, 2]. In children, hemoglobin levels should be assessed depending on age. Anemia is diagnosed when hemoglobin decreases below 110 g/l in children under 5 years of age, below 115 g/l - between the ages of 5 and 12 years, below 120 g/l - over 12 years of age [2, 3] (Table 1 ).
Based on the analysis of erythrocyte indices, all anemias are divided into microcytic (hypochromic), normocytic (normochromic) and macrocytic (hyperchromic) (Table 2) [4].
Anemia is a nonspecific symptom; it can be a manifestation of many pathological conditions, both associated with the primary lesion of the hematopoietic system and independent of it.
Despite the variety of variants of anemia, there are only three mechanisms for its development:
- Violation of erythropoiesis (production of red blood cells by red bone marrow).
- Shortening the life of red blood cells or their hemolysis (destruction).
- Acute or chronic bleeding.
In some types of anemia, a combination of these mechanisms is possible. Anemia in children with chronic pathology of the gastrointestinal tract (GIT) is common, sometimes being the only first sign of a chronic disease. The frequency of anemia in gastrointestinal pathology, according to various sources, ranges from 6 to 74% [5] (Table 3).
In children with chronic gastrointestinal pathology, anemia due to deficiency of iron and vitamins (B12, folic acid), posthemorrhagic anemia (acute and chronic), and anemia of chronic diseases are most often observed. These conditions can be triggered by both blood loss (more often chronic against the background of erosive and ulcerative processes of the gastrointestinal tract, polyposis, microdiapedetic bleeding), and a lack of supply and absorption of microelements and vitamins.
According to WHO, iron deficiency anemia (IDA) ranks first among all anemias. It is characterized by impaired erythropoiesis due to iron deficiency due to a discrepancy between iron intake and consumption, and a decrease in the filling of hemoglobin with iron [4, 6].
The main reasons for the development of iron deficiency states:
- nutritional disorders (impaired intake of iron from food);
- helminthic infestations (increased iron consumption, microblood loss);
- pathology of the gastrointestinal tract (restricted intake of iron from food due to diet, chronic blood loss - erosions, ulcers, microdiapedetic bleeding; impaired absorption of iron due to atrophic changes in the gastrointestinal mucosa).
The most common cause of the development of IDA in children with chronic pathology is blood loss, which can arise from the upper and lower gastrointestinal tract. The cause of blood loss in 85% of cases is pathology of the upper gastrointestinal tract (esophagus, stomach, duodenum), in 14% - the large intestine, and only in 1% of cases - the small intestine. Pathology in the upper gastrointestinal tract (erosive and ulcerative lesions, varicose veins of the esophagus) more often leads to the development of massive acute blood loss, which is manifested by acute posthemorrhagic anemia [7–9]. In acute posthemorrhagic anemia, a large volume (more than 10%) of blood is lost simultaneously. This is an urgent condition that requires immediate elimination of the source of bleeding. Chronic posthemorrhagic anemia is defined as a long-term loss of small volumes of blood, exceeding the body’s ability to restore lost blood loss [10, 11]. The development of chronic posthemorrhagic and IDA in pathology of the upper gastrointestinal tract is much less common than in chronic pathology of the small and large intestine [11]. In 35–90% of cases, bleeding from the colon stops on its own, but often resumes, leading to the development of persistent anemia of mixed origin (posthemorrhagic and iron deficiency) [12]. Chronic IBD often occurs under the guise of functional intestinal disorders, and anemia in these children is considered a separate disease.
Clinical example 1. A boy of 1 year 10 months consulted a gastroenterologist due to weight deficiency, complaints of stool with a tendency to constipation and selective appetite. Pregnancy and childbirth proceeded normally. Breastfeeding to date. Mom ate a large amount of dairy products. In a child from 2 months of age, there was a decrease in hemoglobin level to 105 g/l, color index to 0.8. From the age of 5 months, the child developed skin rashes in the form of manifestations of atopic dermatitis, and blood in the form of dots and dark streaks was periodically detected in the stool. Mom eliminated all products based on cow's milk and beef meat from her diet, but introduced up to 1 liter of whole goat milk into her diet. After 2 weeks, the child experienced an increase in anxiety, regurgitation (immediately after meals and “delayed”), and vomiting up to 5 times a day.
From that moment on, there was a lag in weight gain, a constant admixture of blood and mucus in the stool in larger quantities. By the age of one year, the blood test showed hemoglobin - 77 g/l, color index - 0.7. The doctor recommended taking an iron supplement. After 10 days of iron therapy, the mother independently canceled the treatment due to the fact that the stool became dark. At the age of 1 year 10 months, the child has a weight deficiency of 23%, hemoglobin level – 103 g/l, color index – 0.79, serum iron level is reduced – 6.8 µmol/l (normal – 6.9–29), ferritin low – 7 ng/ml (normal – 30–130). Based on the results of the examination, IDA was diagnosed, which was the result of microdiapedetic bleeding due to the gastrointestinal form of food allergy, which subsequently led to eating disorders, selectivity of appetite (the boy refused meat), and the development of functional constipation.
By following dietary recommendations (complete elimination of dairy products, administration of the amino acid mixture Neocate Advance), the symptoms of atopic dermatitis were stopped, the child’s well-being improved, in a month the weight gain was 500 grams, the appetite increased, and stool was independent once a day. After a course of therapy with an iron preparation based on the hydroxide-polymaltose complex Maltofer orally at the rate of 5 mg per kg of body weight per day, after 3 months there was complete normalization of hemoglobin, serum iron and blood ferritin levels.
Inflammatory bowel diseases are often accompanied by the development of anemia. Anemia in IBD is detected in 35–50% of cases; it develops somewhat more often in ulcerative colitis (UC) than in Crohn’s disease (CD) [11–13]. According to our data, IDA was detected in 37.6% of children with chronic colitis, but latent iron deficiency was detected in 97% [14, 15]. The mechanism of development of anemia in IBD is associated not only with blood loss, impaired iron supply to the body (against the background of a strict diet, inflammation of the intestinal mucosa), but also due to a long-term increase in the level of pro-inflammatory cytokines (TNF-α, interleukins-1, -6, -10, γ-interferon), which leads to disruption of iron metabolism and inhibition of bone marrow hematopoiesis, i.e. to the development of anemia of chronic diseases (ACD) [13].
The role of hepcidin as a missing link in the complex mechanism of erythropoiesis is currently being investigated. Hepcidin is a 20–22 or 25 amino acid small peptide synthesized in the liver and detected in serum and urine. It has an antimicrobial effect, its level increases in any inflammatory diseases. Hepcidin is a direct mediator in the pathogenesis of ACD, directly reducing the absorption of iron in the small intestine and blocking its release from macrophages [16, 17]. Anemia of chronic diseases occurs in chronic inflammatory processes of various organs (lungs, kidneys, liver, gastrointestinal tract), incl. caused by infectious agents, with systemic diseases of connective tissue, endocrine pathology and with neoplasms of various localizations, allergic and autoimmune diseases of the gastrointestinal tract. Normochromic anemia or moderately hypochromic anemia is more common [18]. In terms of prevalence, ACD in patients with chronic gastrointestinal pathology ranks second after IDA [19]. Anemia of chronic diseases is characterized by a decrease in the level of serum iron, THC, transferrin and an increase in serum ferritin. Ferritin is an acute-phase protein of inflammation, therefore, an increased level of serum ferritin in ACD is a manifestation of inflammation, which does not allow its use as an indicator of iron reserves [20].
Erroneous diagnosis of IDA in ACD can lead to the prescription of iron supplements (parenterally) with the subsequent development of secondary hemosiderosis. Currently, a new laboratory parameter, the soluble transferrin receptor (sTfR) is used for the differential diagnosis of IDA and ACD [21]. Research results indicate the high diagnostic value of this test [22].
Not all hypochromic anemias are iron deficiency. The presence of hypochromic anemia does not exclude hypochromic anemia of another origin. It is necessary to carry out a differential diagnosis between IDA and sideroachrestic anemia, in which the iron content in the body is within normal limits or even has an excess [3]. For various reasons, iron is not used to build heme in the hemoglobin molecule, which leads to the formation of hypochromic red blood cells with a low hemoglobin content. Unused iron is stored by the body and deposited in organs and tissues, leading to the development of hemosiderosis. The differential diagnosis of hypochromic anemia should be made between IDA, ACD, thalassemia, anemia due to chronic intoxication with drugs or salts of heavy metals. In pediatric practice, IDA and ACD are the most common; the differential diagnosis between them is given in Table. 4 [23].
Diseases of the small intestine, accompanied by the development of malabsorption syndrome, lead to a deficiency of protein, microelements and vitamins that regulate erythropoiesis (iron, copper, cyanocobalamin, folic acid, etc.), as a result of which deficiency anemia is a natural process in celiac disease and exudative enteropathy. In pathology of the wall of the small intestine (exudative enteropathy), anemia is of an iron deficiency nature due to the chronic loss of serum iron and transferrin with the lymph through ectatic intestinal lymphatic vessels. Anemia in celiac disease is detected in 40–67% of children [24, 25]. Due to atrophy of the small intestine, there is a significant impairment in the absorption of iron, folic acid, vitamin B12, amino acids and other nutrients necessary for full erythropoiesis. However, anemia itself is accompanied by the development of enteropathy in the form of degenerative-dystrophic processes in the digestive canal, leading to achlorhydria, decreased activity of pepsin, amylase, trypsin, disruption of digestion and absorption processes, creating a vicious circle for patients with celiac disease. It has been proven that iron absorption is most affected, which determines the predominantly iron deficiency nature of anemia in celiac disease [26]. With latent celiac disease, IDA is detected in 2.8% of patients as the first sign of the disease [27].
Clinical example 2. A 4.8-year-old girl is observed in the Children's Children's Hospital of Moscow (chief physician - Professor I.M. Osmanov). A child from physiological pregnancy and childbirth was born with normal weight and height parameters. Breastfed until three months of life, then the child received adapted milk formulas and gluten-containing cereals were introduced into the diet from 5–6 months. Until 3.5 years of age, the child’s development corresponded to his age. At the age of 3.5 years, type 1 diabetes was diagnosed, the child was observed in the endocrinology center, insulin therapy was selected with stable glycemic compensation. However, after 4 months from the onset of the disease, the child exhibits an increase in the volume of the abdomen, frequent, loose stools, and then a lag in weight and height (see figure). Weight – 14.7 kg (10.8 perc, -1.24 SD), height – 95 cm (0.4 perc, -2.66 SD). An ultrasound examination of the abdominal organs revealed diffuse changes in the pancreas, which the pediatrician regarded as pancreatitis, and therefore the child was prescribed pancreatin-based enzyme preparations, which did not lead to the expected effect. A blood test after 7 months revealed moderate hypochromic, microcytic anemia (Hb 80 g/l), caries of primary teeth was noted. By the age of 4.5 years, a perversion of taste began to be noted.
Taking into account the increasing clinical manifestations of malabsorption, delayed physical development, and the development of persistent anemia, a blood test was performed to exclude celiac disease. Antibodies to tissue transglutaminase IgA > 500 (with a norm of 0–10 U/ml), antibodies to endomysium Ig G > 1:5 were detected, which served as an indication for endoscopic examination with a biopsy from the duodenum. According to the morphological study, atrophic entropy Marsh 3B–3C was identified, which confirmed the diagnosis of celiac disease in this child. In addition, we carried out genotyping using the HLA system and discovered the DQ2o genotype. Due to confirmed celiac disease and the presence of moderate iron deficiency anemia, Maltofer was prescribed intramuscularly.
Megaloblastic anemia occurs in gastrointestinal pathology and is a group of diseases characterized by impaired DNA synthesis, resulting in disruption of the division of all rapidly proliferating cells (hematopoietic, skin cells, gastrointestinal tract, mucous membranes). Hematopoietic cells are among the most rapidly multiplying elements, so anemia, as well as often neutropenia and thrombocytopenia, come to the fore in the clinic [10]. The main cause of megaloblastic anemia is a deficiency of cyanocobalamin or folic acid.
Pernicious anemia (from the Latin perniciosus - disastrous, dangerous), or B12-deficiency anemia, or megaloblastic anemia, or Addison-Biermer disease, or (outdated name) “malignant anemia” - a disease caused by impaired hematopoiesis due to a deficiency in the body vitamin B12. Bone marrow and tissue of the nervous system are especially sensitive to deficiency of this vitamin. The disease is more common among older people with atrophic gastritis due to insufficient intake of vitamin B12. Vitamin B12 stores range from 2000 to 5000 mcg, more than half of which is stored in the liver. Liver reserves increase progressively with age, but between 1 and 4 mcg of vitamin B12 are lost daily through the biliary tract.
In accordance with the International Statistical Classification of Diseases, Injuries and Conditions Affecting Health, 10th revision [28], the following forms of anemia associated with vitamin B12 deficiency are distinguished:
- D 51.0. Vitamin B12 deficiency anemia due to intrinsic factor deficiency;
- D 51.1. Vitamin B12 deficiency anemia due to selective malabsorption of vitamin B12 with proteinuria;
- D 51.2. Transcobalamin II deficiency;
- D 51.3. Other vitamin B12 deficiency anemias associated with diet;
- D 51.8. Other vitamin B12 deficiency anemias;
- D 51.9. Vitamin B12 deficiency anemia, unspecified.
The main reasons for the development of B12 deficiency anemia are presented in table. 5.
Clinical example 3. A 15-year-old girl consulted a doctor with complaints of a metallic taste in her mouth and the sensation of a hair on her tongue. Notes general weakness, numbness of the fingertips, dizziness and numbness of the feet during physical activity. The girl has been following a vegetarian diet for the last 6 months; for the last month she has been bothered by constipation, alternating with diarrhea. From the anamnesis it is known that at the age of 12 the child suffered an abdominal injury, a resection of part of the ileum (15 cm) and an appendectomy were performed. After 3 years, a blood test revealed a decrease in hemoglobin to 72 g/l, a decrease in red blood cells to 2.5 × 1012, color index, normal - 0.86. A biochemical blood test revealed an increase in total bilirubin to 48 µmol/l (norm - up to 21), a decrease in the level of total protein to 6.0 g/dl (norm - 6.6-9.0 g/dl), ferritin and serum levels iron is within normal limits. Esophagogastroduodenoscopy revealed superficial duodenitis. Ultrasound of the abdominal organs revealed signs of hypomotor dysfunction of the gallbladder.
A large amount of mucus, some undigested plant fiber and soap were found in the coprogram. A blood test revealed antibodies to roundworms in a diagnostically significant titer. The condition was assessed as normochromic anemia of moderate severity, ascariasis.
The girl received antihelminthic therapy with Nemazol 400 mg once. The pediatrician prescribed the iron drug Actiferrin in an age-appropriate dosage orally for 2 months, treatment continued for two months without effect. Taking into account the lack of effect from the therapy, the level of vitamin B12 in the blood was determined, which confirmed the presence of B12-deficiency anemia in the child (resection of 15 cm of the ileum in early childhood). The B12 level was reduced by 1.5 times the norm. After intramuscular administration of vitamin B12, a significant improvement in the child’s condition was noted after 2 weeks. The girl became more active, fatigue decreased, and abdominal pain stopped. After 4 weeks from the start of therapy, paresthesia persisted only during physical activity, the hemoglobin level rose to 114 g/l, the color index was 1.0.
This clinical observation shows errors in the management of this child, since the possibility of B12-deficiency anemia was not taken into account. With normal values of the color index, ferritin and serum iron levels, a diagnosis of IDA was made and treatment with iron supplements was started, which turned out to be ineffective.
Folate deficiency anemia is a disease characterized by the megaloblastic type of hematopoiesis as a result of impaired DNA synthesis (Table 6). It develops more often in young people, children, and pregnant women [30]. Folates are absorbed in the duodenum and upper jejunum. In epithelial cells, polyglutamates are reduced to dihydro- and tetrahydrofolates, which bind to proteins and are transported in the form of methyltetrahydrofolate, where they participate with cyanocobalamin in the biosynthesis of purine and pyrimidine nucleotides and in the transformation of amino acids (histidine into glutamic acid) necessary for the formation of DNA. The total amount of folic acid in the human body is about 70 mg, the third part is represented by liver reserves. Under conditions of folic acid deficiency, the process of erythropoiesis is disrupted and the megaloblastic type of hematopoiesis develops [31].
In accordance with the International Statistical Classification of Diseases, Injuries and Conditions Affecting Health, 10th revision [28], the following forms of anemia associated with folic acid deficiency are distinguished:
- Folate deficiency anemia (D 52).
- D 52.0. Diet-related folate deficiency anemia.
- Megaloblastic nutritional anemia.
- D 52.1. Folate deficiency anemia is drug-induced (if it is necessary to identify the drug, use an additional code for external causes [class XX]).
- D 52.8. Other folate deficiency anemias.
- D 52.9. Folate deficiency anemia, unspecified.
Clinical example 4. A 10-month-old boy was admitted to the gastroenterology department of the Children's Children's Hospital (head of the department - L.A. Kataeva) due to delayed motor development. Lethargy, refusal to eat, and periods of anxiety were noted. The child from a physiological pregnancy was born weighing 3100 grams and 50 cm tall, and was breastfed for up to three months. In the summer, the mother and child went to the village to visit relatives, where, due to hypogalactia, they fed the baby with whole goat milk. No complementary foods were introduced. At the age of 10 months, they first went to the clinic. The child's weight was 7100 grams (underweight - 26.7%), marked pallor of the skin, and a crimson-colored tongue without overlaps. The skin turgor is sharply reduced, the abdomen is increased in volume. In the blood test, hemoglobin is 78 g/l, red blood cells are 2.05 × 1012, color index is 1.14. Biochemical analysis revealed a decrease in protein levels to 6.0 g/dL (normal range: 6.4–8.4 g/dL). Serum iron is normal. Taking into account improper feeding of the child, medical history indicating feeding with whole goat milk, which can lead to the development of folate-deficiency anemia of Jaksh-Gayem, the child was assessed for the content of vitamins B12 and folic acid in the blood. The level of vitamin B12 was within normal limits, the content of folic acid in erythrocytes was reduced to 58 ng/l (normal is 100–450 ng/l). Thus, the child was diagnosed with folate deficiency anemia, which was a natural consequence of feeding the child with whole goat milk in the absence of complementary feeding. The content of folic acid in goat's milk is extremely low - 6 ng/g, while in cow's and women's milk it is significantly higher - 50 ng/g [33]. The child was prescribed a mixture based on the hydrolysis of whey proteins Nutrilon Pepti allergy, oral folic acid in a dose of 5 mg once a day for a month, vitamin D3 Aquadetrim. As a result of the therapy, a month later the child gained 900 grams in weight, became active, walked independently without support, and decreased anxiety and moodiness. In the blood test, hemoglobin was 105 g/l, red blood cells – 3 × 1012. In the biochemical blood test, the level of total protein rose to 6.8 g/dl.
Treatment of anemia in children with gastrointestinal pathology is impossible without treatment of the underlying disease that caused it. The severity of anemia correlates with the degree of disease activity (this is especially pronounced in patients with IBD). In this case, it is necessary to take into account all possible mechanisms for the development of anemia: blood loss, redistribution of iron, dietary features of the diet, impaired absorption of micronutrients in the intestine. Most often, in children with gastrointestinal pathology, anemia is of a combined nature. For example, in patients with IBD at the beginning of the disease, anemia may be normochromic and posthemorrhagic in nature.
Over time, iron deficiency occurs, and then ACD develops. In patients with Crohn's disease in combination with celiac disease, it is possible to develop not only iron deficiency conditions, but also B12-deficiency anemia, especially after intestinal resection [13, 35, 36].
Treatment of the underlying disease should include elimination (reduction) of inflammatory activity, normalization of gastrointestinal motility, digestion and absorption processes in the intestinal lumen. In cases of severe posthemorrhagic anemia, blood transfusions may be used. In this case, first of all, it is necessary to stop the bleeding and then correct the anemia. Due to the temporary effect, high risk of complications and the possibility of iron overload, their use is limited.
Treatment of anemic conditions in gastrointestinal diseases should include the administration of iron supplements due to the predominant iron deficiency nature of anemia (Table 7). With the development of IDA, it is impossible to compensate for iron deficiency without medicinal iron-containing drugs [37]. The effectiveness of treatment with iron supplements depends on the severity of the anemia, the chosen iron supplement and the method of its administration. For small intestinal atrophy, the administration of oral iron supplements is ineffective, because due to disruption of absorption processes, iron is not transferred from the intestinal lumen to the blood. The maximum adsorption capacity of the intestine for absorbing iron is on average 1–2 mg per day, which is clearly not enough for the effective correction of anemia [3]. Oral medications can independently cause or aggravate inflammatory changes in the intestinal mucosa, because their excess in the intestinal lumen promotes the development of free radical reactions, including oxidative stress. More than 20% of patients stop taking iron supplements due to complications from taking them, without achieving correction of IDA [38]. To the greatest extent, these complications are observed when using divalent iron salts (ferrous sulfate, etc.). Ferric hydroxide-polymaltose compounds do not cause such complications and can be used from a safety point of view, but their effectiveness is limited in cases of inflammation of the intestinal wall.
Thus, it is often advisable for patients with gastrointestinal pathology to use parenteral forms of iron in the acute period of the disease, with a further transition to oral forms. Intravenous iron preparations have a great advantage - iron sucrose (Venofer), which do not depend on absorption and are able to quickly and effectively replenish iron deficiency and its reserves (increased transferrin levels). Enteral iron supplements are indicated for patients with gastroenterological pathology for the correction of iron deficiency and the treatment of mild to moderate iron deficiency anemia in the absence of bleeding in the upper gastrointestinal tract and severe intestinal absorption disorders [39, 40].
Prescribing oral medications to children with gastroenterological pathology requires compliance with certain conditions:
- Iron preparations must be safe and not cause toxic and oxidative reactions, incl. and due to uncontrolled absorption.
- Iron preparations should not have an irritating effect on the mucous membranes of the gastrointestinal tract.
- Iron preparations should have high bioavailability and be well absorbed.
- At the moment, there are many iron preparations on the market, both divalent and trivalent.
For the use of iron supplements in pediatrics, only a few meet all the requirements. It is optimal to use hydroxide-polymaltose compounds of ferric iron (Maltofer), which have different release forms, which makes it easy to dose the drug for children of different ages. However, the use of only iron supplements for children with chronic gastrointestinal pathology will be effective only if the predominant nature of iron deficiency anemia is present [41]. In other cases, especially with a long-term recurrent course of IBD and the development of not so much iron deficiency as ACD, it does not lead to a significant and lasting correction of anemia, but is also fraught with iron overload with the development of hemosiderosis [41].
Step-by-step therapy for ACD in IBD:
Step 1. Treatment of the underlying disease. The success of therapy will depend on the degree of compensation of IBD [42].
Step 2. Treatment with iron preparations parenterally, because due to incomplete absorption, oral forms will have a toxic effect and aggravate changes in the intestinal mucosa [36, 43, 44].
Step 3. The most effective and pathogenetically justified for the correction of ACD is the administration of erythropoietin, which compensates for its insufficient endogenous production and helps to increase the sensitivity of red bone marrow cells to erythropoietin. However, it must be remembered that the administration of erythropoietin inevitably leads to high iron consumption by erythroid precursors and rapid depletion of its reserves in the body [42]. The result is iron deficiency erythropoiesis, which returns us to step 2. In parallel with erythropoietin, intravenous iron supplements are required, which is especially indicated for patients with mixed genesis of anemia. The use of erythropoietin in combination with iron supplements leads to a faster achievement of normal hemoglobin levels [18, 36].
The dosage for the course of administration of iron is calculated using the Ganzoni formula [45, 46, 48]. Iron deficiency (in mg) = body weight (in kg) × 0.24 × (proper hemoglobin - actual hemoglobin in g/l) + 500 mg.
Indications for the use of parenteral iron supplements [48, 49]:
- severe anemia;
- high activity of IBD;
- simultaneous therapy with erythropoietin;
- intolerance to oral forms of iron;
- insufficient effect from the use of oral forms of iron;
- patient preferences (rare).
In this case, first of all, it is necessary to stop the bleeding and then correct the anemia.
Patients with mixed genesis of anemia due to malabsorption syndrome are advised to use vitamin B12 and folic acid [47]. With adequate treatment, an increase in the number of reticulocytes in the blood is observed within the first 3 days; on the 7th–10th day, a reticulocyte crisis (peak reticulocytosis) is observed. By the 3rd–4th weeks of treatment, there is an increase in hemoglobin level by 20 g/l. Taking iron supplements should be continued for another 3–6 months after normalization of hemoglobin levels - until transferrin saturation with iron exceeds 30% and ferritin concentration reaches 50 ng/ml (an indicator of restoration of tissue iron reserves) [48, 49].
Diagnosis of Addison's disease
Diagnosis of Addison's disease is based on laboratory tests and special tests. Instrumental methods are used if it is necessary to determine the degree of changes in the adrenal glands during a long-term pathological process.
Laboratory tests for Addison Birmer's disease
The patient must submit:
- complete blood count (usually increased hematocrit);
- blood biochemistry (sodium concentration is reduced, potassium concentration is increased);
- general urine analysis (the concentration of metabolic products of testosterone (17 ketosteroids) and glucocorticoids (17 oxyketosteroids) is reduced).
Laboratory tests also show a decrease in testosterone, aldosterone, and cortisol levels.
Diagnostic tests for Addison's disease
Diagnostic tests for Addison's disease are aimed at determining which endocrine organ is primarily affected. If the pathology concerns only the adrenal glands and does not affect the pituitary gland and hypothalamus, a decrease in the level of hormones of the adrenal cortex is diagnosed against the background of an increase in the concentration of hormonally active substances produced by the pituitary gland and hypothalamus.
The patient may be prescribed the following tests:
- Using adrenocorticotropic hormone (ACTH). ACTH is a pituitary hormone responsible for the production of hormones by the adrenal cortex. In healthy people, the concentration of aldosterone and cortisol doubles half an hour after its administration. If Addison's disease is present, the numbers do not change.
- Test with synacthen depot. Synacthen is a synthetic analogue of adrenocorticotropic hormone. Normally, it increases the secretion of cortisol, but this does not happen in patients, since the affected adrenal glands are not able to respond to the stimulating effect. Accordingly, the hormones cortisol and aldosterone remain at the same level.
Instrumental diagnostics for Addison-Birmer's disease
Instrumental diagnostic methods for Addison's disease include:
- Computed tomography, magnetic resonance imaging. If the problem is caused by tuberculosis, enlarged adrenal glands are found. In this case, deposits of calcium salts in the affected areas are clearly visible. If the disease is caused by autoimmune processes, the pictures show reduced adrenal glands.
- Electrocardiogram (changes in the functioning of the heart due to disturbances in electrolyte and water-salt metabolism are detected).
- X-ray of the skull bones. The examination is carried out if disorders in the hypothalamus or pituitary gland are diagnosed. X-rays are directed directly to the area of the sella turcica (where the pituitary gland is located). If there is hemorrhage or swelling, the images will show clearly visible darkening or lightening of the affected areas.
Taking into account the clinical picture of the disease, the results of laboratory and instrumental examinations, the doctor can make an accurate diagnosis and confirm or deny the presence of Addison Birmer disease in the patient.
Differential diagnosis
Most often, Addison's disease is differentiated (distinguished) from the following diseases:
- secondary adrenal insufficiency caused by a decrease in the production of adrenocorticotropic hormone by the pituitary gland;
- congenital adrenal hyperplasia (a group of hereditary pathologies arising due to impaired cortisol biosynthesis);
- adrenoleukodystrophy (hereditary degenerative disease of the central nervous system, which is transmitted in an X-linked recessive manner and is associated with adrenal insufficiency);
- autoimmune polyendocrine syndrome type 2 (Schmidt syndrome, a rare autoimmune disease in which there is a sharp decrease in the function of several endocrine organs: adrenal glands, thyroid gland, parathyroid glands, gonads, pancreas);
- autoimmune polyendocrine syndrome type 1 (a rare genetic syndrome APECED, which is characterized by lesions of the skin and mucous membranes by Candida fungi, decreased function of the parathyroid glands and autoimmune insufficiency of adrenal function).
Treatment of Addison's disease
Since mineralocorticoids (aldosterone), glucocorticoids (cortisol) and other important hormones in the human body are produced only in the adrenal glands, therapy is aimed mainly at the selection of effective replacement drugs, mineralocorticoids and glucocorticoids of synthetic origin.
Cortisone is most often used in the treatment of Addison-Birmer's disease. The dose of the drug is selected individually. The following factors are taken into account:
- It is important to start taking it with minimal doses and gradually increase the amount until the condition of the systems and organs is normalized.
- The amount of synthetic hormone must be equal to the physiological level of hormones that a healthy body can produce.
- Cortisone is recommended to be taken in descending order. The highest dose is in the morning, the average dose is in the afternoon, and the smallest dose is in the evening. This is explained by the fact that in the morning the adrenal cortex is most active, after which it gradually decreases and becomes minimal closer to the night.
- During crises of Addison's disease, the hormone is administered intramuscularly or intravenously. If the patient is in a state of stress or severe emotional shock, the administered dose can be increased.
Relieving symptoms of Addison's disease
- In order to normalize the disturbed electrolyte balance and replenish the volume of lost fluid, physiological sodium chloride solution is injected intravenously.
- If the glucose level is low, a five percent glucose solution is administered intravenously.
Also, during treatment of the pathology, the doctor must monitor the patient’s body weight, monitor his blood pressure, and periodically prescribe a urine test for the concentration of 17-KS and 17-OX.
In a situation where Addison's disease is caused by tuberculosis, it is recommended to take anti-tuberculosis drugs, for example, Streptomycin or Isoniazid.
Addisonian crisis
If Addison's disease is left untreated, the levels of cortisol and aldosterone in the body will gradually decrease. This will cause progressive worsening of symptoms and will eventually lead to a situation known as Addisonian crisis.
An Addisonian crisis is when the symptoms of Addison's disease come on very quickly and very strongly. The condition may develop when the above symptoms become worse.
Addisonian crisis is a medical emergency. If left untreated, it can be fatal. If you or someone you know has Addison's disease and any of the symptoms listed below occur, call an ambulance (numbers: 103, 112).
Symptoms of Addisonian crisis:
- severe dehydration;
- severe hypotension;
- shock (when organs and tissues do not receive enough blood);
- severe vomiting and diarrhea;
- extreme muscle weakness;
- headache;
- extreme drowsiness or coma;
- death.
Diet for Addison Birmer's disease
Comprehensive treatment for Addison's disease uses a nutrient-rich diet. It is important that the patient’s daily diet contains increased amounts of proteins, fats and carbohydrates. Vitamin C (cabbage, onions, apples), B vitamins (egg yolk, beans, carrots, liver) and others are also needed. If they are deficient, patients' metabolism is disrupted.
Since a lack of aldosterone leads to the accumulation of potassium ions in the body, doctors advise patients to limit foods that contain a lot of this trace element (potatoes, peas, bananas, nuts).
Prevalence
Primary adrenal insufficiency is rare: according to domestic authors, it occurs in 1 in 4000-6000 hospitalized patients. American endocrinologists provide data on 39-60 cases of adrenal insufficiency per 1 million population. Chronic adrenal insufficiency (CAI) is more common in men; The ratio of men to women suffering from this disease is 2:1. According to German doctors - Oelkers and his colleagues - the average age at which the disease is diagnosed is 40 years (from 17 to 72).
B12 anemia: treatment
Treatment tactics for B12-deficiency anemia are developed by CELT specialists according to diagnostic results and individual patient indications. If the diagnosis is confirmed, treatment will be carried out for life, and every five years an endoscopic examination of the gastric mucosa will be required, eliminating the risk of developing malignant neoplasms.
In order to compensate for the deficiency of the vitamin, the patient is prescribed intramuscular administration. Treatment of diseases and disorders that initiated the development of anemia is carried out:
- elimination of helminths;
- taking digestive enzymes;
- operations for diverticula and malignant tumors;
- food with a high content of animal protein;
- taking glucocorticoids for disorders of the production of internal factor.
If you start treating anemia in a timely manner, your blood counts will return to normal in one and a half to two months. Neurological symptoms persist for up to six months; if treatment was started at an advanced stage, they are irreversible and cannot be cured.
The Department of Hematology at CELT welcomes candidates, doctors and professors of medical sciences with over twenty-five years of practical and scientific experience. You can make an appointment with them online or by contacting our operators. No less experienced and qualified specialists perform septoplasty in the otolaryngology department.
At CELT you can consult a hematologist.
- Initial consultation – 3,500
- Repeated consultation – 2,300
Make an appointment
By making an appointment with a hematologist, you can get a comprehensive consultation. The doctor is competent to treat various blood diseases, most of which can be identified in the early stages and prescribe timely treatment to cope with the disease quickly and easily.
Laboratory findings
The most common abnormalities in blood tests are increased levels of potassium (above 5 mmol/l) and creatinine with decreased levels of sodium (up to 110 mmol/l) and chlorine (below 98.4 mmol/l). Serum calcium levels are rarely elevated. Hypercalcemia in such cases is combined with hypercalciuria, thirst, polyuria and hyposthenuria. Patients may also develop normocytic normochromic anemia; peripheral blood smears show eosinophilia and relative lymphocytosis. A slight increase in TSH levels is often recorded (usually < 15 μU/ml). It remains unclear whether this increase in TSH is due to concomitant autoimmune thyroid disease, lack of TSH suppression by endogenous steroids, or the development of a euthyroid pathological syndrome.
Impaired renal function is observed: glomerular filtration rate and renal blood flow decrease.
Metabolic disorders and electrolyte metabolism disorders lead to changes in the ECG. Usually, an enlarged and pointed T wave is detected, which in some leads can even exceed the QRS complex in height. Possible slowing of atrioventricular or intraventricular conduction.
The diagnosis is based not only on clinical findings and laboratory tests, but also on direct confirmation of a decrease in the functional activity of the adrenal glands. If the level of corticosteroids in blood taken at 8-10 a.m. is less than 170 nmol/l (6 mcg/100 ml), then the diagnosis of adrenal insufficiency is beyond doubt. The presence or absence of pigmentation indicates the primary or secondary nature of the disease. In primary CIU, ACTH levels are usually elevated, while in secondary CIU, ACTH levels are usually decreased. Also, to clarify the diagnosis, a series of pharmacodynamic tests are carried out - fluctuations in cortisol are recorded when ACTH or insulin is administered. An insulin test allows one to differentiate tuberculous damage to the adrenal cortex from its destruction by an autoimmune process. Tuberculous damage is accompanied by destruction of the medulla (in which catecholamines are synthesized), while when affected by an autoimmune process, changes occur only in the cortical layer of the adrenal gland. Therefore, by determining the content of adrenaline in the blood serum during the insulin test along with glucocorticoids, it is possible to establish the cause that caused chronic adrenal insufficiency.
To diagnose hypoaldosteronism, the concentration of aldosterone in the blood plasma or its excretion in the urine is determined. Here again, preference should be given to pharmacodynamic tests. Angiotensin is a specific stimulator of aldosterone secretion. If the aldosterone concentration does not increase at the end of the angiotensin infusion, this indicates hypoaldosteronism.
Mode
Addison's syndrome does not allow patients to engage in heavy physical labor. Any stressful condition (infection, physical or mental stress, etc.) requires an increase in glucocorticoid intake. The principle of clinical observation in relation to these patients must be strictly observed. All patients with Addison's syndrome are provided with a special leaflet, which indicates a rational schedule for taking corticosteroids and the optimal single and daily doses of various corticosteroid drugs for a given patient. In case of an urgent situation, glucocorticoids should be ready for parenteral administration. Warning information should also be prepared for doctors in case the patient is unable to independently provide information about his illness. Patients should be aware that they should consult a doctor immediately if they experience weakness, malaise, fever, abdominal pain, diarrhea, or other signs of worsening condition. Drinking alcohol, taking barbiturate sleeping pills, and using alkaline mineral waters to wash down tablets containing corticosteroids are prohibited.
1. Balabolkin M. I. Endocrinology, 1998 2. McDermott M. Secrets of endocrinology, 2001 3. Wolfgang Oelkers M. Adrenal issuficiency. The New England Journal of Medicine, Vol. 335, no. 16, p. 1206-1212 https://www.temple.edu/imreports/Reading/Endo%20%20-Adrenal%20insuff.pdf 4. May M., Vaughn E., Carey R. Adrenocortical insufficiency - clinical aspects. In: Adrenal disorders, 1989, p. 171-189 5. Oelkers W., Diederich S., Bähr V. Recent advances in diagnosis and therapy of Addison's disease. Journal of Endocrinology Vol. 1. 1994, p. 69-80
B12 anemia: causes
The daily requirement of the human body for vitamin B12 is from one to five micrograms. It is satisfied through its consumption with food: after entering the stomach, the vitamin is separated from protein under the influence of enzymes. In order for the body to fully absorb it, a process of connection with glycoprotein and other factors must occur. Absorption of the vitamin into the blood occurs in the lower part of the ileum, from where it passes to the tissues. Factors that can initiate the development of anemia are divided into two groups:
- Nutritional – an unbalanced diet that is unable to ensure the required amount of B12 enters the body. This often happens if the patient practices fasting, vegetarianism, or diets that minimize or eliminate the consumption of animal protein;
- Endogenous – disruptions in the process of vitamin absorption due to a deficiency of protein that binds the vitamin and converts it into an absorbable form. A similar phenomenon can be initiated by: a congenital absence of the internal Castle factor;
- inflammatory processes of the gastric mucosa in a chronic form;
- condition after gastric excision surgery;
- condition after partial removal of the ileum or duodenum;
- inflammation of the small intestine (enteritis), pancreas (pancreatitis);
- gluten enteropathy;
- granulomatous inflammation of the digestive tract (Crohn's disease);
- protrusions of the intestinal wall - (diverticula);
- neoplasms of the jejunum of a malignant nature;
- helminthic infestations caused by different types of helminths.
The reasons may lie in physical and mental dependence on alcohol intake, in the use of Colchicine, Neomycin, as well as a number of oral contraceptives.