A scar on the heart in medical terminology is called cardiosclerosis. The essence of the pathological process is the death of cardiac muscle cells and their replacement with connective tissue, this can happen after a heart attack or as a result of an inflammatory process. An ECG helps identify changes in the heart muscle and specify the extent of damage.
This process is dangerous for the patient’s life, since fibrous tissue is tougher in structure than muscle fibers; it is not able to contract in a rhythm synchronous with all other parts of the heart. For patients experiencing heart scarring, it is important to know the causes of this phenomenon and to prevent further changes in the heart muscle. Without appropriate help, the consequences of fibrosis can be very diverse, from heart failure and aneurysm of the lower wall of the heart to sudden death as a result of a second heart attack.
Development mechanism
At the time of the development of an acute infarction, a sharp disruption of the blood supply to the myocardium occurs for the following reasons:
- Rupture of an atherosclerotic plaque under the influence of a sharp jump in pressure, increased heart rate and acceleration, and accelerated blood flow through the coronary vessels.
- Blockage of blood vessels due to blood thickening (acceleration of platelet aggregation, activation of the coagulation system, decreased rate of blood clot lysis).
- Spasm of the coronary artery (vasoconstriction).
I often observed patients in whom several factors were identified as the cause of the disease with myocardial damage. In young patients, vasospasm is often the basis of pathological disorders, which is not possible to determine after the start of treatment.
Prevention
To prevent cardiosclerosis, the doctor prescribes vitamins, magnesium, potassium, antiarrhythmic drugs that strengthen cardiovascular activity. It is also necessary to undergo regular electrocardiography.
For normal heart activity, it is important to follow a sleep and rest schedule, monitor blood pressure, avoid heavy exercise and walk in the fresh air. You need to eat food in moderation. It is advisable to exclude salty, sweet, fatty, spicy, as well as soda and alcohol from the diet. Food should be rich in vitamins and minerals. The diet should be based on boiled meat, fish, vegetables, fruits and dairy products.
The ABC Medicine clinic offers you to undergo diagnostics and a full course of treatment for cardiosclerosis. Call us by phone + and our clinic consultants will answer all your questions in detail and make an appointment with a specialist.
Expert advice
I strongly recommend starting treatment in a hospital immediately after an acute attack, since only in this case is it possible to limit the further spread of necrosis and minimize irreversible changes in the myocardium.
The study of histological samples confirms the destruction of the cardiac myocyte 20 minutes after the development of ischemia. After 2-3 hours of lack of oxygen, their glycogen reserves are depleted, which marks their irreversible death. Replacement of myocarditis with granulation tissue occurs within 1-2 months.
As my practice and the observations of colleagues show, the scar on the heart is finally consolidated after six months from the moment the first symptoms of acute infarction appear and is a section of coarse collagen fibers.
Classification
Heart scars can be classified according to their location and extent of distribution.
They can be located along the coronary vessels:
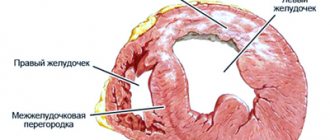
- Impairment of blood flow in the anterior interventricular artery leads to ischemia with the subsequent appearance of a scar in the area of the septum between the ventricles, involving the papillae and lateral wall, as well as on the anterior surface and apex of the left ventricle.
- The infero-posterior and lateral part is affected when the left circumflex coronary artery is blocked.
- Problems with the blood supply to the myocardium in the right artery results in irreversible changes in the right ventricle and can affect the posterior inferior part of the left ventricle and the septum. But such a violation is extremely rare.
According to the type of distribution, scars can be local (focal), which can be compared to a scar on the body, or diffuse (multiple). Experts call the second option dystrophic changes in the myocardium.
How does a scar manifest itself?
The acute period of a heart attack is characterized by a variety of clinical manifestations. The main symptom is pain, which can be relieved exclusively with narcotic analgesics and can be observed from an hour to 2-3 days. Then the pain syndrome disappears and the formation of an area of necrosis begins, which takes another 2-3 days. Then comes a period of replacing the affected area with loose connective tissue fibers.
If the correct treatment tactics are used, the following symptoms are noted:
- development of compensatory hypertrophy;
- rhythm disturbance (which often accompanies the acute period) is eliminated;
- tolerance to stress gradually increases.
If a scar that appears on the heart crosses the conduction paths along which the impulse travels, a conduction disorder is recorded, such as a complete or partial blockade.
In the case of successful recovery after a primary small-focal infarction, I did not notice any significant disturbances associated with the functioning of the heart in my patients.
If patients have formed a large scar or many small ones, the following deviations are observed:
- dyspnea;
- increased heart rate;
- the appearance of edema;
- enlargement of the left chambers of the heart;
- pressure fluctuations.
Symptoms
This disease often develops without any symptoms. This is especially true for moderate degrees of diffuse cardiosclerosis, as well as focal forms. Experts usually associate this diagnosis with a disturbance in the rhythm of the heart muscle or pain syndrome. Sometimes arrhythmias of varying degrees are the first signs of developing sclerosis. In the diffuse form of cardiosclerosis, they may be accompanied by cardiac contraction disturbances or heart failure. The more tissues are affected, the stronger the symptoms of cardiosclerosis will be.
In atherosclerotic and post-infarction forms, the symptoms of cardiac cardiosclerosis are approximately the same:
- the heart rhythm is heard intermittently;
- difficulty breathing (shortness of breath);
- increased heart rate;
- pulmonary edema;
- pain in the heart area;
- enlarged liver, swelling of the extremities, accumulation of fluid in the abdominal and pleural cavities.
Both of these forms of the disease can be accompanied by arterial hypertension.
The identified symptoms of cardiac cardiosclerosis develop progressively, since the disease itself tends to progress as scars form.
How dangerous is this?
The most dangerous is the development of a scar as a result of large-focal or transmural infarctions, as well as several repeated violations in different basins of the coronary vessels with diffuse multiple lesions.
In the case of a large area of damage or widespread cardiosclerosis, the remaining healthy cells cannot fully compensate for the work of damaged cardiomyocytes. The frequency and strength of contractions increases in order to provide organs and tissues with oxygen and necessary substances.
As a result, tachycardia develops; with its appearance, the load on the heart becomes even greater, which leads to dilatation of the left ventricle and atrium. As it progresses, blood stagnation appears in the right side with the development of heart failure.
I also observed another type of complication: a scar on the heart after a heart attack with extensive and deep damage to all layers of the organ caused the formation of an aneurysm due to the thinning of its wall.
The reasons for the appearance of such a defect are:
- transmural lesion;
- increased blood pressure;
- increased blood pressure inside the ventricle;
- excessive physical activity of the patient, refusal to comply with the regimen.
An aneurysm leads to the rapid development of heart failure, the formation of a parietal thrombus, and pronounced stagnation in the systemic circulation. Often complicated by severe rhythm disturbances leading to death (paroxysmal tachycardia and ventricular fibrillation).
Diagnostics
In order to establish a diagnosis, I conduct a survey and study the medical history (mainly, it includes ischemic heart disease with a history of heart attack). External examination usually reveals increased respiratory rate, weakening of heart sounds during auscultation, the presence of edema, and various rhythm disturbances. I will definitely take a blood pressure measurement.
Then I send you to the following research:
- general and biochemical blood test, coagulogram (will help establish concomitant diseases, cholesterol levels and clotting time);
- EchoCG or ultrasound of the heart helps to establish the presence of localized or diffuse areas of connective tissue, allows you to clarify the location and extent of distribution;
- MRI helps to visualize and reliably assess the affected area;
- scintigraphy is required to determine dysfunctional areas of the myocardium.
With the help of an ECG after a transmural and large-focal infarction, it is possible to clarify where the scar is located on the diseased heart.
It is determined by the presence of a Q wave in different leads, as can be seen in the table.
| ECG leads | Localization of post-infarction scar in the left ventricle |
| V1-V3 | Anterior wall with septal involvement |
| V3-V4 | Anterior wall and apex |
| I, aVL, V5-6 | Anterolateral sections |
| I, aVL, V1-6 | Entire front wall |
| II, III, aVF | Posterior wall and diaphragmatic region |
| V7-8 | Posterobasal area |
The increase in the T wave and ST segment, which are characteristic of the acute period, is no longer observed. ST returns to the isoline, T decreases. With a small area and depth of the lesion, no signs of a scar remain; it is leveled, since the function of conductivity and contractility is taken over by neighboring cells. A nonspecific manifestation of dystrophic changes can be a smoothed or moderately negative T wave.
Sources
- Chen W., Bian W., Zhou Y., Zhang J. Cardiac Fibroblasts and Myocardial Regeneration. // Front Bioeng Biotechnol - 2021 - Vol9 - NNULL - p.599928; PMID:33842440
- Deng M., Chen W., Wang H., Wang Y., Zhou W., Yu T. The disappearance of IPO in myocardium of diabetes mellitus rats is associated with the increase of succinate dehydrogenase-flavin protein. // BMC Cardiovasc Disord - 2021 - Vol21 - N1 - p.142; PMID:33731005
- Ikeda G., Santoso MR., Tada Y., Li AM., Vaskova E., Jung JH., O'Brien C., Egan E., Ye J., Yang PC. Mitochondria-Rich Extracellular Vesicles From Autologous Stem Cell-Derived Cardiomyocytes Restore Energetics of Ischemic Myocardium. // J Am Coll Cardiol - 2021 - Vol77 - N8 - p.1073-1088; PMID:33632482
- Villa Del Campo C., Liaw NY., Gunadasa-Rohling M., Matthaei M., Braga L., Kennedy T., Salinas G., Voigt N., Giacca M., Zimmermann WH., Riley PR. Regenerative potential of epicardium-derived extracellular vesicles is mediated by conserved miRNA transfer. // Cardiovasc Res - 2021 - Vol - NNULL - p.; PMID:33599250
- Alagarsamy KN., Mathan S., Yan W., Rafieerad A., Sekaran S., Manego H., Dhingra S. Carbon nanomaterials for cardiovascular theranostics: Promises and challenges. // Bioact Mater - 2021 - Vol6 - N8 - p.2261-2280; PMID:33553814
- Liu X., De la Cruz E., Gu X., Balint L., Oxendine-Burns M., Terrones T., Ma W., Kuo HH., Lantz C., Bansal T., Thorp E., Burridge P ., Jakus Z., Herz J., Cleaver O., Torres M., Oliver G. Lymphoangiocrine signals promote cardiac growth and repair. // Nature - 2021 - Vol588 - N7839 - p.705-711; PMID:33299187
- Stępniewski J., Tomczyk M., Andrysiak K., Kraszewska I., Martyniak A., Langrzyk A., Kulik K., Wiśniewska E., Jeż M., Florczyk-Soluch U., Polak K., Podkalicka P., Kachamakova-Trojanowska N., Józkowicz A., Jaźwa-Kusior A., Dulak J. Human Induced Pluripotent Stem Cell-Derived Cardiomyocytes, in Contrast to Adipose Tissue-Derived Stromal Cells, Efficiently Improve Heart Function in Murine Model of Myocardial Infarction. // Biomedicines - 2021 - Vol8 - N12 - p.; PMID:33297443
- Xu D., McBride E., Kalra K., Wong K., Guyton RA., Sarin EL., Padala M. Undersizing mitral annuloplasty alters left ventricular mechanics in a swine model of ischemic mitral regurgitation. // J Thorac Cardiovasc Surg - 2021 - Vol - NNULL - p.; PMID:33288234
- Regard S., Rosa D., Suppan M., Giangaspero C., Larribau R., Niquille M., Sarasin F., Suppan L. Evolution of Bystander Intention to Perform Resuscitation Since Last Training: Web-Based Survey. // JMIR Form Res - 2021 - Vol4 - N11 - p.e24798; PMID:33252342
- Ruan Y., Zeng J., Jin Q., Chu M., Ji K., Wang Z., Li L. Endoplasmic reticulum stress serves an important role in cardiac ischemia/reperfusion injury (Review). // Exp Ther Med - 2021 - Vol20 - N6 - p.268; PMID:33199993
Treatment
Treatment of dystrophic changes includes the use of medications, diet, and lifestyle changes.
Drug therapy
The choice of medications for the appearance of scars depends on the person’s condition.
Typically, after a heart attack and the formation of scar tissue, the following groups of drugs are used:
- statins to lower cholesterol levels (Atorvostatin, Rosuvastatin);
- Beta blockers and ACE inhibitors (Bisoprolol, Ramipril) help reduce the load on the LV and increase its resistance to ischemia
- diuretics allow you to remove swelling and relieve the systemic circulation (Indapamide, Torasemide).
Surgical intervention
When the scar causes complete blockade of the conduction system, treatment consists of installing a pacemaker (pacemaker). An operation (coronary artery bypass surgery) allows you to restore blood flow, when a section of a damaged coronary artery is replaced by another vessel.
In cases of severe degenerative processes and the development of heart failure incompatible with life, an organ transplant is required.
Traditional methods
It is impossible to treat cardiosclerosis and scar changes in the myocardium using traditional methods. They only slightly alleviate a person’s condition, complementing general therapy. However, neither mumiyo nor celandine, as the “healers” write, are capable of ridding the patient of a scar, much less restoring the functioning of the heart.
Diet
The diet after a heart attack and scar formation depends on the degree of damage to the heart muscle.
General nutritional requirements are:
- maximum salt restriction;
- reducing fluid consumption (up to 1.5 liters);
- eliminating foods high in cholesterol;
- mandatory use of products with potassium;
- if you are overweight, you should reduce the total number of calories;
- Avoid caffeinated drinks completely.
It should be noted that currently there are no effective ways to completely get rid of a heart scar. Repeated attempts to restore tissue using stem cells have so far been unsuccessful.
Consequences of cardiosclerosis
The disease will lead to a deterioration in the functioning of the heart muscle and an increased risk of various complications. Even if the causes are eliminated and the pathological process is stopped, the presence of connective tissue in the myocardium leads to adverse consequences. In the near future, problems can be dealt with surgically or with medication, but the patient will not be able to get rid of them completely.
The most common complications and consequences of cardiosclerosis are:
- arrhythmias;
- CHF;
- thromboembolism;
- cardiac aneurysm;
- CFS;
- acquired heart defects.
Case from practice
A patient came to me for a consultation with complaints of shortness of breath, fatigue, and swelling in the ankles.
History of large-focal myocardial infarction. On examination, the skin is pale and pasty (mild swelling) of the legs. Auscultation - heart sounds are slightly muffled. Blood pressure is within the age norm (130 to 75 mm Hg). The ECG shows signs of dystrophic changes in the posterior wall of the LV, post-infarction scar in the anteroseptal region. After examination, a moderate change in the myocardium and mild hypertrophy of the left ventricle were discovered. A biochemical blood test showed an elevated level of low-density cholesterol.
Diagnosis: IHD. Post-infarction cardiosclerosis, heart failure I. Received treatment with beta blockers, prescribed Aspirin Cardio in a minimal dosage, and a diuretic. She recommended lifelong use of statins (Atorvastatin) under the control of cholesterol levels. She prescribed a diet with a low amount of salt, limiting fluid to 1.5 liters per day, stopping smoking and drinking alcohol. After 2 weeks of treatment, pastiness is not detected, shortness of breath has decreased, and exercise tolerance has increased.
What is a microinfarction?
Don't know. In world medicine such a term does not exist. Sometimes “microinfarction” is understood as unstable angina. This is an intermediate condition between myocardial infarction and an acute attack of angina. With unstable angina, a small zone of thrombosis occurs, but the vessel is not completely blocked, blood flow is maintained, which means the myocardium does not die. However, unstable angina can rightfully be called a “pre-infarction state”, and therefore, the treatment of such patients includes almost the entire complex that we discussed for patients with a heart attack, including mandatory coronary angiography and often the installation of a stent.