Causes of aortic stenosis
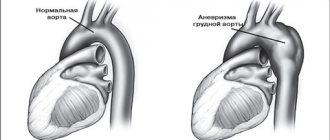
The cause of the development of aortic stenosis may be the following diseases: 1. Rheumatism, 2. Protracted septic endocarditis, 3. Atherosclerosis, 4. Infectious diseases. 5. Congenital pathology In addition to true organic stenosis of the aortic mouth, relative stenosis is distinguished, when the aortic valves are not changed, and the ascending part of the aorta is sharply expanded due to arterial hypertension or as a result of loss of elasticity of the aortic wall (atherosclerosis). Aortic stenosis creates a significant obstacle to the flow of blood from the left ventricle into the systemic circulation only if the area of the aortic opening is reduced by more than 50%. Maintaining even 10-20% of its normal value is compatible with life. The lengthening of the systole (contraction time) of the left ventricle and the increase in pressure in its cavity, as a compensatory reaction to the narrowing of the aortic mouth, causes the development of pronounced hypertrophy (increase in muscle mass) of the left ventricle. With no other defect does such significant hypertrophy of the left ventricular myocardium develop as with stenosis of the aortic mouth. Since the powerful left ventricle takes part in the compensation of aortic stenosis, the defect occurs for a long time without circulatory disorders. A long period of compensation is a feature of this defect.
Publications in the media
Aortic valve insufficiency is a pathological condition characterized by retrograde blood flow from the aorta into the left ventricular cavity through a defective aortic valve.
Frequency. Among those who died from various heart pathologies, aortic valve insufficiency was detected in 14% of cases, of which in 3.7% - in isolated form, and in 10.3% - in combination with other defects. Since 1999, more than 80% of heart valve surgeries have involved aortic valve replacement.
Etiology • Rheumatism, including cases of secondary infective endocarditis (46.5%) • Medionecrosis (18%) • Primary infective endocarditis (12.8%) • Congenital anomalies (flapping cusp syndrome, isolated aortic valve insufficiency, annuloaortic ectasia , abnormalities in the number of aortic valve cusps), including cases of secondary infective endocarditis - 13.5% • Syphilis (2.1%) • Aortitis in Reiter's disease, ankylosing spondylitis, rheumatoid arthritis (2.1%) • Connective tissue diseases, such as syndrome Marfana et al. (1.9%) • Traumatic and spontaneous rupture of aortic valves (1.3%) • Atherosclerosis (0.9%) • Arterial hypertension (0.9%).
Pathophysiology • Hemodynamic disturbances are caused by regurgitation of blood from the aorta into the left ventricle during diastole. The volume of regurgitation depends on the area of the defect, the magnitude of the diastolic pressure gradient between the aorta and the left ventricle, the duration of diastole • An increase in the diastolic volume of the left ventricle leads to its tonogenic dilatation • According to the Frank-Starling law, the left ventricle ejects an increased volume of blood into the aorta, which, together with regurgitation, leads to a decrease in diastolic blood pressure, an increase in systolic and pulse blood pressure • As myogenic dilatation develops, the end-diastolic volume and end-diastolic pressure of the left ventricle increase, which leads to stagnation of blood in the pulmonary circulation • Congestion in the pulmonary circulation increases with the development of relative insufficiency mitral valve due to dilatation of the left ventricle • Compensation mechanisms: decreased peripheral vascular resistance, tachycardia, left ventricular hypertrophy.
Clinical picture and diagnosis • Complaints •• No complaints - 4.5% •• Episodes of angina - 20.1% •• Syncope episodes - 1.0% •• Dyspnea on exertion - 31.4% •• Orthopnea - 2.8 % •• Symptoms of systemic venous hypertension - 25.6% •• Paroxysmal nocturnal dyspnea (cardiac asthma) or pulmonary edema - 32.4% •• Combination of dyspnea with syncope and episodes of angina - 0.8% •• Other symptoms - 1 .3%.
• Peripheral symptoms are caused by low diastolic and high pulse blood pressure. It should be borne in mind that all peripheral symptoms are nonspecific and are possible with neuroses, anemia, thyrotoxicosis, arteriovenous malformations, etc. •• Corrigen's sign (carotid dance) - pronounced pulsation of the carotid arteries •• High and fast pulse •• Musset's sign - shaking of the head with each pulse wave •• Müller's sign - pulsating uvula •• Pulsation of retinal arterioles •• Quincke's sign - pulsating color change lips or nail bed, synchronous with pulse; determined by pressing on them with a glass slide •• Hill's symptom - the difference between blood pressure in the arms and legs is more than 20 mm Hg •• Double Traube tone - listening to loud (similar to a pistol shot) tones on the femoral arteries •• Durosier's symptom - systolic murmur on the femoral artery when it is clamped proximal to the site of auscultation and diastolic murmur when the femoral artery is clamped distal to the site of auscultation •• Listening to heart sounds on the palmar surface of the hand •• Listening to heart sounds on the palmar surface of the hand when raising the hand up •• Listening to the pulse above the superficial palmar arch .
• Valve symptoms •• Soft (flowing) diastolic decreasing murmur, following immediately after the aortic component of the second sound (best heard in the second intercostal space to the right of the sternum during exhalation when the patient’s torso is tilted forward), carried out to Botkin’s point •• Rough musical murmur (murmur “cooing pigeon”) occurs when the valve flaps or perforates the valve •• With decompensation and a pronounced increase in end-diastolic pressure of the left ventricle, the intensity of the murmur of aortic regurgitation weakens •• Austin Flint murmur is a mesodiastolic low-frequency murmur of relative mitral stenosis, arising in connection with the covering of the anterolateral mitral leaflet valve with a stream of regurgitation in severe aortic insufficiency. The degree of attenuation of the first tone reflects the severity of decompensation of the defect for the same reason. •• Systolic murmur over the aorta, caused by an increase in the volume of ejection from the left ventricle, can be heard in the absence of aortic stenosis.
• Left ventricular symptoms are caused by hypertrophy, dilatation and insufficiency of the pumping and contractile functions of the left ventricle •• Diffuse, prolonged apical impulse, shifted to the left and down •• Palpation detectable III tone •• Increase in the area of relative dullness of the heart to the left •• Auscultatory signs of congestion in the lungs - diffuse moist rales of various sizes, best heard in the basal regions.
• Symptoms of an underlying disease , such as Marfan syndrome, aortic aneurysm, syphilis, infective endocarditis.
Special studies • ECG: signs of hypertrophy and overload of the left parts of the heart, primarily the left ventricle. • X-ray examination of the chest organs: bulging of the left ventricular arch and aorta, enrichment of the pulmonary pattern in pulmonary hypertension.
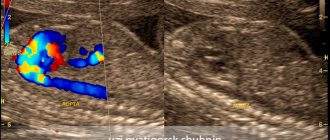
• EchoCG •• Dilation of the cavity and hypertrophy of the left ventricular myocardium •• Violation of local and global systolic, as well as diastolic functions of the left ventricle •• Dilation of the ascending aorta •• Damage to the aortic valve leaflets (defects, vegetations, abnormalities in the number of leaflets, expansion of the fibrous ring, leaflet prolapse) •• In Doppler mode - pathological flow from the aorta to the left ventricle during diastole, the volume of which (recorded in color mapping mode) corresponds to the severity of the defect •• Increased systolic pressure of the right ventricle with stagnation of blood in the pulmonary circulation •• Signs lesions of other heart valves with combined defects •• In order to determine the size of the prosthesis, it is necessary to measure the diameter of the aorta at the level of the fibrous ring, sinuses and ascending limb ••
Transesophageal echocardiography is performed for the purpose of detailed diagnosis of the condition of the thoracic aorta, more accurate identification of vegetations on the valves, thrombosis of the left atrium in the presence of atrial fibrillation, as well as for patients in whom transthoracic visualization turned out to be difficult (due to obesity, emphysema, etc.).
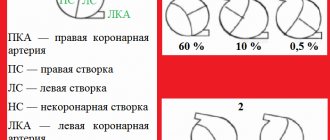
• Catheterization of the left and right ventricles and aorta •• In case of left ventricular failure - increase in end-diastolic pressure of the left ventricle •• In case of congestion in the pulmonary circle - increase in pressure in the right ventricle, pulmonary artery wedge pressure •• Tests are performed to determine the prognosis for pulmonary hypertension with aminophylline and oxygen inhalation •• Depending on the volume of regurgitation as a percentage of the stroke volume of blood, four degrees of aortic valve insufficiency are distinguished ••• I degree - 15% ••• II degree - 15–30% ••• III degree - 30–50%, ••• IV degree - more than 50%.
• Left ventriculography , ascending aortography •• The presence and degree of regurgitation is determined by the number of contractions required to completely expel the contrast agent from the cavity of the left ventricle •• The presence of zones of hypo- and akinesia of the left ventricle indicates myocardial ischemia •• Combined valvular lesions are also diagnosed.
• Coronary angiography •• Performed in the presence of episodes of angina and positive results of stress testing, as well as in all women over 45 years of age, men over 40 years of age and all candidates for aortic valve replacement to exclude concomitant coronary artery disease.
TREATMENT • Drug therapy •• For asymptomatic mild aortic insufficiency, only annual dynamic monitoring (examination, echocardiography, ECG) and limitation of isometric physical activity are indicated (an increase in aortic regurgitation and damage to the aortic root is possible) •• For moderate asymptomatic aortic insufficiency, ACE inhibitors and conduct a clinical examination every 6 months •• In case of severe asymptomatic aortic insufficiency, constant use of peripheral vasodilators and clinical examination every 6 months (or immediately in case of decompensation) are necessary •• Treatment of decompensated aortic insufficiency is carried out according to the general principles of treatment of circulatory failure (vasodilators, cardiac glycosides, diuretics ).
• Surgical treatment •• Indications: aortic regurgitation grade III–IV or grade II in the presence of at least one of the following conditions: heart failure functional class III–IV (according to the New York Heart Association classification), angina pectoris, syncope, acute left ventricular failure (cardiac asthma or pulmonary edema), end-diastolic pressure in the left ventricle above 15 mm Hg •• Contraindications: severe concomitant pathology that threatens the patient’s life; terminal stage of circulatory failure •• Methods of surgical treatment ••• Aortic valve replacement with a mechanical artificial heart valve under artificial circulation ••• Biological prostheses are used in children ••• In the presence of an aneurysm of the ascending aorta - simultaneous replacement of the aortic valve and ascending aorta with a valve-containing conduit according Bentall or Cabrol method.
Specific postoperative complications • Thromboembolism • Secondary infective endocarditis of prostheses • Degenerative changes in biological valves and the need for re-prosthesis • Aneurysms of the ascending aorta when using disc prostheses with a small opening angle.
Prognosis • In the natural course, the 5-year survival rate does not exceed 45%, and the 10-year survival rate does not exceed 38% • After identifying symptoms of the disease, the average life expectancy is 2–5 years • After identifying left ventricular dilatation, the 10-year survival rate does not exceed 56% • With acute development of the defect (usually infective endocarditis), the average life expectancy is 7 months •• With surgical treatment, hospital mortality is 1–3%, 12-year survival exceeds 70% (with initial heart failure of functional class III according to the New York Heart Association classification ). Synonym. Aortic valve insufficiency
ICD-10 • I06.1 Rheumatic aortic valve insufficiency • I06.2 Rheumatic aortic stenosis with insufficiency • I35.1 Aortic (valvular) insufficiency • I35.2 Aortic (valvular) stenosis with insufficiency • Q23.1 Congenital aortic valve insufficiency
Symptoms of aortic stenosis
Aortic stenosis is more common in men, especially older men, as a result, for example, of calcium deposits on the valve leaflets. In young people, the most likely cause is congenital anomalies. Complaints in patients with aortic stenosis are determined by the cause of the defect, the nature and course of the disease that caused the defect, the severity and stage of development of the defect. At the stage of compensation of the defect, patients do not complain. The defect is most often discovered accidentally. In patients with more severe stenosis of the aortic mouth, during physical activity (less often at rest), there may be dizziness, a feeling of lightheadedness, fainting, increased fatigue, and compressive pain in the heart and behind the sternum. The combination of squeezing pain in the heart with dizziness and fainting is especially characteristic. The appearance of attacks of cardiac asthma and shortness of breath at rest indicates a significant decrease in the contractility of the left ventricle. Pallor of the skin is observed. Stagnation occurs in the pulmonary and then systemic circulation, which causes the appearance of acrocyanosis and edema.
Aortic stenosis (narrowing of the aorta)
Aortic stenosis is a narrowing of the opening through which blood flows from the left ventricle of the heart into the aorta.
What is aortic stenosis?
Aortic stenosis can be congenital (due to disruption of the formation of the aortic valve during intrauterine development) and acquired (due to the effects of pathological processes, that is, diseases).
Aortic stenosis can be valvular or subvalvular. Valvular stenosis is the type of aortic stenosis in which the lumen of the aortic valve narrows. Subvalvular stenosis is called a stenosis caused by a narrowing of the outflow tract of the left ventricle under the aortic valve due to thickening of the muscular septum, or the presence of a membrane.
Why does it arise?
Normally, the aortic valve has 3 thin cusps, which, when opening, allow blood from the heart to the internal organs, and when closing, prevent blood from getting back into the heart and overloading it.
Quite often, as a result of a violation of intrauterine development, the aortic valve from birth may have only 2 leaflets, this leads to accelerated “aging” of the valve with the formation of a narrowing of its lumen.
Everyone knows such a disease as atherosclerosis; it affects the vessels of all organs, as well as some structures of the heart. The aortic valve is an intravascular formation as it is located in the lumen of the main artery of the body, the aorta. When atherosclerotic plaques develop on the aortic valve, thickening of the leaflets may occur. Thickened valves lose elasticity and become covered with calcium salts, which narrows the lumen.
Who can get sick
The disease is typical for patients of any age. Children are born with a bicuspid aortic valve, which makes them sick from birth. Subvalvular membrane is also a congenital defect. ( Any age )
Atherosclerosis progresses with age in all people, causing the gradual formation of aortic stenosis in a certain proportion of the population. ( Most typically from 45 to 70 years old )
A special group consists of elderly people in whom the function of the aortic valve arises as a result of its aging along with the entire body. ( Over 60 years old )
Subvalvular aortic stenosis often develops in women with a rare hereditary disease - hypertrophic cardiomyopathy. ( Ages 12 years and older, women are affected )
Anyone who has long-term high blood pressure and does not receive proper treatment can develop thickening of the heart muscle (myocardial hypertrophy), which can cause partial blockage of blood flow from the heart. ( Ages 35 and older )
What are the symptoms of the disease?
Aortic stenosis is an insidious disease. For a long time, no symptoms may appear at all; this is due to the compensatory capabilities of the body.
The following complaints are typical for this disease:
- Shortness of breath with little physical activity (people around you may notice that you get tired faster)
- Heartbeat
- Interruptions in heart function
- Pain in the heart area during exercise and at rest
- Dizziness when changing body position, or physical effort, stress.
- Late stages of the disease are characterized by sudden attacks of loss of consciousness
- Edema of the lower extremities
How is the diagnosis made?
Most often, when undergoing a professional examination, medical examination, or fluorography, doctors may notice significant deviations in the shape of the heart or changes in the electrocardiogram. An experienced cardiologist will always be able to hear a rough heart murmur characteristic of aortic stenosis and will prescribe a number of studies:
- Electrocardiograms
- X-ray of the chest organs
- 24-hour Holter ECG monitoring
- ECHO-cardiography (ultrasound of the heart)
- In difficult cases, multislice computed tomography with the introduction of a contrast agent is required.
This scope of research allows you to confirm or exclude the diagnosis, determine the stage of the disease and prognosis.
In the later stages of the development of the defect, patients are admitted to the cardiology department with symptoms of acute myocardial infarction; an incorrect diagnosis is often made and the effect is treated rather than the cause.
What are the stages of the disease?
Aortic valve stenosis occurs:
- Easy
- Moderate
- Expressed
- Heavy
- Critical
Who is treating?
Mild to moderate aortic stenosis is monitored by a cardiologist with periodic consultations with a cardiac surgeon.
Severe, severe and critical aortic stenosis is treated by a cardiac surgeon. The treatment method is surgical replacement of the aortic valve.
What are the approaches to surgical treatment?
Depending on the stage of the disease, the age of the patient and many other factors, there are open surgical techniques, minimally invasive techniques, and endovascular aortic valve replacement (TAVI).
Each method has its own advantages and disadvantages.
Aortic valve replacement using an open technique under artificial circulation.
During open surgery, a longitudinal incision of the sternum and complete visualization of the heart are performed under artificial circulation. Then a heart-lung machine is connected, the heart stops, the altered heart valve is excised, and a prosthetic heart valve is securely sewn in its place.
Advantages of the method:
- Wide use
- This approach is considered excellent
- It is easy to influence complications that arise during surgery
Disadvantages of the method:
- Significant surgical trauma (scar length 20-25 cm).
- The need to sleep strictly on your back for 3 to 6 months.
Duration of the operation: from 3 to 6 hours.
In the intensive care unit: usually about 36 hours.
Total duration of hospitalization: 12-15 days.
Risk of intervention: about 1.5%
Aortic valve replacement from a mini-access under artificial circulation
This surgical correction option is characterized by a smaller incision, which is less traumatic for the patient. The course of the operation is similar to open surgery.
Advantages of the method:
- Less traumatic method
- Cut about 10 cm long
- Early rehabilitation
- There is no need to sleep on your back for long periods of time
Disadvantages of the method:
- Great technical complexity
- Limited ability to influence complications during surgery, or requires switching to a larger incision
Duration of the operation: from 2 to 8 hours.
In the intensive care unit: usually about 24 hours.
Total duration of hospitalization: 10-15 days.
Risk of intervention: more than 2%
Endovascular aortic valve replacement
Since 2007, intravascular aortic valve replacement has been used worldwide. With this approach, a large artery of the thigh is punctured, a folded prosthetic aortic valve is passed through the vessel into the heart, in the right place it is inflated on a special balloon and, breaking the narrowed aortic valve, it becomes in its place.
Advantages of the method:
- Minimal trauma, incision is 1 cm, often the intervention is performed under local anesthesia
Disadvantages of the method:
- It is extremely difficult to influence the complications that arise.
- High price
- Possibility of implantation of exclusively biological prosthetic heart valve
- There are many restrictions and contraindications for carrying out.
Duration of the operation: from 1 to 6 hours.
In the intensive care unit: usually about 24 hours.
Total duration of hospitalization: 5-10 days.
Risk of intervention: moderate
What's the prognosis?
If you seek medical help in a timely manner, most patients, after successful surgical treatment, fully return to normal life within 3-6 months. People who work physically can return to work after 4-6 months; if the work does not involve physical effort, 6-8 weeks is often enough for rehabilitation. It should be understood that in each specific case the pace of rehabilitation is individual and depends on the patient’s age, the degree of “neglect” of the case, the presence of concomitant diseases, and complications during treatment.
I need to get examined! What are the stages?
1. Consultation with a cardiac surgeon.
After an in-person examination and a standard physical examination, it is possible with a high degree of probability to confirm or refute aortic stenosis.
Research will be conducted:
- Electrocardiography
- ECHO-cardiography (ultrasound of the heart)
If the diagnosis is confirmed, further examination is indicated before hospitalization in a specialized hospital.
- Determination of blood group, Rh factor
- Diagnosis of HIV, hepatitis B, C, syphilis
- General urine analysis
- General blood analysis
- Standard biochemical blood test
- X-ray of the chest organs, or fluorography
- Consultation with a urologist for men, a gynecologist for women
- Fibrogastroscopy
The main purpose of the examination before planned hospitalization is to exclude possible contraindications.
2. Hospitalization to a specialized hospital for further examination
In a hospital setting the following will be performed:
- Coronary angiography (men over 40 years old, women in menopause)
- Control ECHO-cardiography
- Examination with the participation of the head of the department or a professor as part of a council in order to determine the indications for surgical treatment and the choice of treatment tactics.
3. Discharge from the hospital with the exact date of hospitalization for surgical treatment if consent and indications are available.
4. Registration of a quota of high-tech medical care for surgical intervention.
5. Hospitalization for surgical treatment
6. Postoperative observation.
If you find yourself with similar symptoms, or your cardiologist suggests this diagnosis, do not hesitate, seek qualified medical help, we will conduct an examination on an outpatient basis, accompany hospitalization in a specialized hospital for high-tech additional examination and surgical treatment, and ensure proper monitoring after the operation.
Without surgical treatment of severe forms, the long-term prognosis for life is unfavorable. Patients die from acute myocardial infarction, sudden arrhythmic death, rupture of aortic aneurysm, aortic dissection, and progressive congestive heart failure.
Remember: aortic valve stenosis cannot be treated with pills and IVs!!!
Make an appointment now
Treatment of aortic stenosis
— All patients, incl. and with minor aortic stenosis that does not have clinical symptoms are under close medical supervision - Patients with aortic stenosis without severe symptoms are recommended to be examined every 3-6 months - Echocardiography - every 6-12 months - All patients with aortic valve stenosis require prophylaxis endocarditis (antibiotics) before, for example, dental treatment or other invasive procedures (regardless of age, cause or degree of stenosis)
Drug therapy
— There is no specific drug treatment. Drug treatment is aimed at stabilizing hemodynamics - Prevention of infective endocarditis is indicated. Indications for surgery: - pressure gradient between the left ventricle and the aorta is more than 50 mm Hg. Art., or the area of the aortic opening is less than 0.7 cm2 (normally its area in adults is 2.5-3.5 cm2) - angina pectoris, fainting, signs of heart failure. Surgical treatment: — Radical treatment — aortic valve transplantation. — Balloon valvuloplasty of the aortic valve is indicated for elderly, debilitated patients who may not undergo valve replacement surgery
Minimally invasive aortic valve replacement surgery
Return to section:
Cardiology department
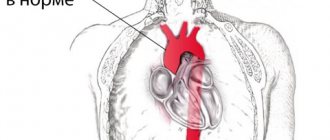
The blood expelled by the heart enters the aorta. The aorta is the largest vessel in the human body, through which blood is directed to organs and tissues. The aorta is connected to the heart by the aortic valve. By opening, this valve facilitates the outflow of blood from the heart; when closing, it prevents blood from penetrating back into the heart chambers.
Surgery to replace (prosthetic) the aortic valve may be required if dysfunction (malfunction) of the valve occurs. This, in turn, may be due to two reasons:
- The aortic valve narrows and does not allow the required amount of blood to pass through, i.e. Blood flow to the body decreases - this is called “aortic stenosis.” Among the main causes are age-related degenerative changes and rheumatism.
- The valve “leaks”, does not hold blood, and blood leaks back into the heart cavity - this is called “aortic regurgitation”. The main causes: congenital genetic defects, age-related enlargement of the aorta and valve ring, aortic diseases and bacterial damage to the valve.
Aortic valve replacement surgery involves removing the failed valve and replacing it with an artificial one. The operation is performed under conditions of artificial circulation, i.e. in a stopped heart, when the function of blood supply to organs and tissues is taken over by a special device. During the operation, the patient is under anesthesia and does not feel pain.
The first operation of aortic valve replacement with an artificial valve was performed in the early 1960s. Traditionally, the operation is performed through a 20 cm long midline incision in the sternum. To reach the heart, it is necessary to cut through the skin, soft tissue, the bone located in the middle of the chest, called the sternum, and the special lining of the heart, the pericardium. The next step is to connect the heart-lung machine by sequentially connecting the aorta and cardiac veins to it, and then temporarily stop the heart. Next, the surgeon dissects the aorta in a transverse direction to see the aortic valve. If the valve is severely damaged, it is removed and a new, artificial heart valve is sewn in its place. Artificial valves are divided into two types:
- Mechanical (metal-carbon): durable, can work effectively for decades, but requires lifelong use of drugs that reduce blood clotting (anticoagulants), which increases the risk of bleeding;
- Biological (created from animal or human tissue): more physiological, but less durable, lasting no more than 20 years, but does not require lifelong use of anticoagulants.
| Modern types of artificial heart valves: on the left – mechanical; on the right is biological. | |
After installing a new valve, the integrity of the aorta, sternum, soft tissue of the chest and skin is restored in turn. The duration of the operation is 2.5 – 3 hours.
| Operational access scheme. Full median sternotomy (left), J-shaped ministernotomy (right). | |
Modern knowledge and experience make it possible to reduce the size of the chest wound to perform aortic valve replacement surgery. Such operations are called minimally invasive, i.e. low-traumatic - through reduced access. The use of small accesses was proposed in the mid-1990s.
The technique of surgical intervention remains the same, but the length of the incision is only 7 centimeters, and you can do without a complete dissection of the sternum (full median sternotomy), which can significantly reduce the trauma of the operation, the severity of pain in the postoperative period, preserve the skeletal function of the chest, and speed up the recovery of the respiratory system. functions and return to normal life while maintaining high effectiveness of treatment.
The undoubted advantage for the patient with this operation is the cosmetic result.
Unlike traditional surgery, minimally invasive surgeries take slightly longer (3 – 3.5 hours).
Rice. 3 . Appearance of the chest wound after traditional (left) and minimally invasive surgery (right).
Over the past decade, a new, unique method of aortic valve replacement has been developed: Transcatheter Aortic Valve Implantation (TAVI).
This procedure is performed in a cath lab with a team consisting of cardiologists, cardiac surgeons, and x-ray surgery specialists. Most importantly, this procedure is performed on a beating heart, thus avoiding the risks associated with cardiopulmonary bypass.
An incision 3 cm long is made on the side of the chest as shown in Figure 4. In this case, the intervention is called transapical catheter valve implantation.
Rice. 4 . Access scheme for transapical catheter implantation of the aortic valve (Cheung, Lichtenstein, Annals of Cardiothoracic Surgery, 2012).
Two special hemostatic sutures are placed in the area near the apex of the heart, through which a high-tech device is passed - a delivery system, the diameter of which is only 8 mm. This system contains a biological valve in a “collapsed” state.
The valve is positioned at the required level under the control of an X-ray machine, which can rotate around the patient on a special arc, making it possible to obtain X-ray images from different angles.
Next, the artificial valve opens, occupying a predetermined position in the aortic root. The valve can be opened either using a balloon inflated with helium (see Fig. 5), or independently - for valves with a frame made of shape memory metal called “Nitinol” (an alloy of nickel and titanium).
| Opening an artificial valve using a balloon | View of the valve installed in the aortic position during transapical catheter implantation |
| (Cheung, Lichtenstein, Annals of Cardiothoracic Surgery, 2012). | |
Rice. 6 . Biological valve for implantation in the aortic position using a transcatheter method.
It should be noted, however, that there are strict indications for such an operation. Transcatheter valve implantation is performed for those patients who are contraindicated for traditional surgical intervention due to high risk (they may not tolerate traditional surgery): these are patients with critical aortic valve stenosis, usually elderly (over 80 years old), patients who have undergone coronary artery bypass surgery, patients with diseases of the aorta, which create technical difficulties when accessing the heart and valve from the classical approach.
The transcatheter implantation operation takes about 40 - 60 minutes, and the recovery period after it is much shorter compared to traditional surgery.
At the Department of Cardiac Surgery of City Hospital No. 40, all considered types of correction of acquired aortic valve defects are used.
← Back