Aortic valve insufficiency
Aortic valve insufficiency - or aortic regurgitation - is a pathological condition in which the heart's aortic valve leaflets do not close tightly. The valve defect allows blood to flow back from the aorta into the left ventricle.
Backflow prevents the heart from effectively pumping blood to the rest of the body. As a result, you feel tired and short of breath. Aortic valve insufficiency can develop suddenly (acutely) or over a long period of time. Aortic insufficiency has many causes, ranging from congenital heart defects to complications of infectious diseases. Over time, aortic valve insufficiency becomes severe and surgery to replace the aortic valve is required.
Symptoms
Most often, aortic valve regurgitation develops gradually and your heart compensates for the problem. You may not have any signs or symptoms for many years, and you may not even know you have the disease.
However, when aortic valve regurgitation gets worse, the following symptoms appear:
- fatigue and weakness, especially when the level of exercise increases;
- shortness of breath on exertion or at rest;
- chest pain (angina), discomfort and tension, often increasing during exercise;
- increased heart rate (arrhythmia);
- heart murmur;
- rapid heartbeat - sensations of rapid, fluttering pulse;
- swelling of the ankles and feet (edema).
Rate of progression of aortic valve damage:
- mild aortic stenosis
(aortic valve opening area -1.2 - 2 cm2) becomes severe, requiring aortic valve replacement, over 10 years - in 10% of patients, over 25 years - in 38%; - with moderate asymptomatic aortic stenosis
(the area of the aortic valve opening is 0.75 - 1.2 cm2), aortic valve replacement is required after 10 years in 25% of cases; - asymptomatic severe aortic stenosis
(aortic valve opening area <0.75 cm2) usually progresses more quickly; 30–40% of patients develop symptoms within 2 years and there is a need for aortic valve replacement.
Atrial fibrillation, aortic regurgitation (spontaneous or caused by infective endocarditis), mitral regurgitation, and acute myocardial infarction accelerate decompensation.
In uncomplicated aortic stenosis, the characteristic auscultatory picture is: systolic murmur at Botkin’s point and at the base of the heart on the right, carried out to the vessels of the neck, weakening of the 2nd sound due to the aortic component. The intensity of the systolic murmur may decrease with the development of left ventricular systolic dysfunction and is not a criterion for the severity of the defect. Often the course of aortic stenosis is complicated by pathology of the mitral valve (“mitralization”).
Causes
Aortic valve regurgitation disrupts the normal flow of blood through your heart and its valves.
Your heart, the center of the cardiovascular system, has four chambers. The two upper chambers, the atria, receive blood. The two lower chambers, the ventricles, pump blood to the lungs and the rest of your body. Blood flows through the chambers of the heart, supported by the four clans of the heart.
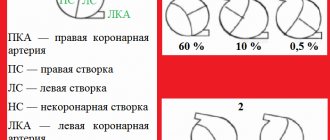
The aortic valve is made up of three tight-fitting, triangular pieces of tissue called cusps. These leaflets are attached to the aorta through the so-called ring.
Heart valves open only in one direction. The aortic valve leaflets can only open into the left ventricle and blood is ejected into the aorta. When the blood has passed through the valve and the left ventricle has relaxed, the valves close so that the blood that just passed into the aorta does not flow back into the left ventricle.
A faulty heart valve may not open or close completely. When the valve does not close tightly, blood can leak back. This backflow of blood through the valve is called regurgitation.
The mechanism of pathology development
Understanding the underlying causes of deviation lies through the assimilation of minimal anatomical and physiological information.
The normal activity of the heart is as follows. Through the chambers of the atria, blood moves into the ventricles, which are responsible for providing the organs with liquid connective tissue.
The left one is the most important: it moves oxygen and nutrients in a large circle. That is, it is through him that all structures are provided.
The aorta emerges into the lumen - the largest artery of the body not only in humans, but also in many mammals in general. Its branches make it possible to adequately supply the body and distant formations through a wide network.
As valve insufficiency develops, the inlet flaps do not close completely at first, and then stop closing altogether.
At the first moment, a partial circulatory disorder occurs, and then a generalized one, depending on the amount of liquid connective tissue disabled.
Correction is carried out by radical (surgical) measures. Even in the early stages, if there are manifestations.
Risk factors
The risk of aortic regurgitation is greater if you are affected by any of the following:
- Damage to the aortic valve.
Inflammation associated with certain conditions, such as endocarditis or rheumatism, can damage your aortic valve. - High blood pressure (hypertension).
High blood pressure makes the heart work harder, increasing stress on the aortic valve, which can make it less elastic and prone to leaking. - Congenital defect of the aortic valve.
If you were born with a unicuspid or bicuspid aortic valve, your chances of aortic regurgitation increase. - Disease.
Certain conditions, including Marfan syndrome, ankylosing spondylitis and syphilis, can cause dilatation of the aortic root (where the aorta attaches to the ventricle), resulting in a leaky aortic valve.
conclusions
Aortic regurgitation is a pathological condition that occurs when the valve leaflets are unable to block the exit from the left ventricle. Stretching
its cavity with an excessive amount of blood leads to a deterioration in contractile activity.
Regurgitation can be detected using Doppler echocardiography and aortography; other methods indicate only its indirect signs.
Even if the study reveals grade 2 aortic valve regurgitation, this does not necessarily indicate the need for surgery. Although the army did not provide a place for people with such pathology.
Complications
Aortic valve insufficiency—or any heart valve problem—puts you at risk for endocarditis. Endocarditis is an infection of the inner lining of the heart, the endocardium. Typically, this infection affects one of the heart valves, especially if it is already damaged. If the aortic valve is incompetent, it is more susceptible to infection than a healthy valve. You may develop endocarditis when bacteria from another part of your body travels through the bloodstream and travels to your heart.
When aortic valve regurgitation is of moderate severity, it may not pose a serious threat to your health. But when it is severe aortic valve regurgitation, it can lead to heart failure. Heart failure is a serious condition in which your heart is unable to pump enough blood to meet your body's needs.
Etiology of mitral regurgitation:
- Congenital pathology: cleft valve, prolapse, etc.
- Ischemic mitral valve dysfunction in ischemic heart disease.
- Degenerative processes: myxomatous degeneration, Marfan and Ehlers-Danlos syndromes, mitral annulus calcification.
- Inflammatory lesions: rheumatism, systemic lupus erythematosus, systemic scleroderma, aortoarteritis.
- Infection: infective endocarditis.
- Injury.
According to the course, mitral regurgitation is divided into chronic and acute and, accordingly, requires a different approach when determining the indications for the urgency of surgical intervention.
Correction of chronic mitral regurgitation must be carried out before left ventricular decompensation develops, taking into account echocardiography criteria for assessing the severity of mitral regurgitation. The development of acute mitral regurgitation, refractory to drug therapy, is an indication for emergency surgery.
The manifestation of clinical symptoms of mitral regurgitation is determined by the severity of mitral valve insufficiency and the functional state of the left ventricle.
Diagnostic tests
Common tests to diagnose aortic valve regurgitation include:
- Echocardiogram.
This test uses sound waves to produce an image of your heart. In echocardiography, sound waves are sent to your heart from a wand-like device (transducer) placed on your chest. Sound waves bounce off your heart and are reflected back through your chest wall and processed electronically to provide video images of your heart. An echocardiogram allows your doctor to take a close look at your aortic valve. A certain type of echocardiography, Doppler echocardiography, may be used. This allows measurements of the volume of blood that flows in the opposite direction through the aortic valve. This volume is expressed in cubic centimeters per beat. - Chest X-ray.
Using a chest X-ray, your doctor can examine the shape and size of your heart to determine whether your left ventricle is enlarged, a possible sign of damage to the aortic valve. - Electrocardiogram (ECG).
In this test, wires (electrodes) are attached to your skin to measure electrical impulses from your heart. The pulses are reflected as waves displayed on a monitor or printed on paper. An ECG can provide information about whether the left ventricle is enlarged, a problem that can occur with aortic valve insufficiency. - Transesophageal echocardiography.
This type of echocardiography allows you to take a closer look at your aortic valve. A “sensor tube” is inserted through your esophagus and goes into your stomach and is closer to your heart. In traditional echocardiography, a device called a transducer moves on your chest to produce the sound waves needed to create a picture of your beating heart. In transesophageal echocardiography, a small probe is attached to the end of a tube and passed through the esophagus. This is done to better visualize the image of your aortic valve and the bleeding through it, since the sensor is closer to the valve itself. - Exercises, tests.
Various types of exercise tests to assess activity tolerance and test your heart's response to exercise (sports). - Cardiac catheterization.
Your doctor may order this procedure if noninvasive tests have not provided enough information to firmly diagnose the type and severity of your heart disease. The doctor threads a thin tube (catheter) through a blood vessel in your arm or groin and into your heart. A contrast agent is injected through a catheter in your heart, making details visible on an X-ray. Cardiac catheterization can show if blood is flowing back from the aorta in the heart into the left ventricle. Some catheters are equipped with special sensors that can measure pressure within the chambers of the heart. Pressure may be increased in the left ventricle with aortic valve insufficiency.
ECG
These tests help doctors diagnose aortic valve regurgitation, determine how severe the problem is, and decide whether your aortic valve needs replacement.
Treatments and drugs
Treatment for aortic valve insufficiency depends on how severe the symptoms of the disease are and how the damaged valve affects the functioning of the heart.
Observation
Individuals with mild aortic valve regurgitation do not require treatment. However, even if you do not have signs and symptoms of aortic valve insufficiency, it is worth seeing your doctor regularly. Regular monitoring by a doctor will help to identify the progression of the disease and recommend the correct treatment.
Medicines
Medicines cannot eliminate aortic valve insufficiency. However, there are a number of drugs that help reduce the symptoms of the disease. Control your blood pressure and your weight.
Surgery
As aortic regurgitation progresses, valve replacement surgery may be required. The heart is usually good at fighting problems caused by a leaky aortic valve, the problem is that if the valve is not fixed or replaced in due time, the strength of your heart can decrease so much that it permanently weakens. You can avoid this by having surgery at the appropriate time.
Overall cardiac function and the amount of regurgitation helps determine when surgery is necessary. Surgical procedures include:
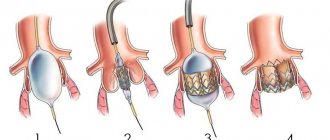
- Aortic valve plastic surgery.
Aortic valve repair is performed to preserve the valve and improve its function. Sometimes surgeons can modify the original valve (valvuloplasty) to eliminate the backflow of blood. You will not need long-term drug therapy to prevent blood clots (anticoagulant therapy) after valvuloplasty. - Valve replacement surgery.
In many cases, the aortic valve must be replaced to correct aortic valve regurgitation. Your surgeon removes your aortic valve and replaces it with a mechanical valve or a biologic valve. Mechanical valves, made of metal, are durable, but they carry the risk of blood clots forming on or near the valve. If you have a mechanical aortic valve, you will need to take anticoagulant medications such as warfarin (Coumadin) for life to prevent blood clots. Biological valves, made from pig, cow or human cadaveric donor tissue, often need to be replaced. Sometimes another type of biological valve can be used, which is your own pulmonary artery valve (autograft).
Aortic valve
Traditionally, aortic valve replacement surgery is performed on an open-heart procedure. A less invasive approach is transcatheter aortic valve implantation—installation of a new valve using a catheter through the femoral artery in your leg (transfemoral) or the left ventricle of your heart (transapical). Currently, this procedure is generally limited to those individuals who have aortic valve stenosis or aortic valve regurgitation, and carries a high risk of surgical complications. In the future, transcatheter aortic valve implantation may be an option for the treatment of aortic regurgitation.
Aortic valve insufficiency can be corrected with surgery and you will usually be back to your normal life within a few months. The prognosis after surgery is good.
How are prolapses treated?
In severe cases, prolapses require surgical treatment (replacement of the valve with an artificial one, or surgical measures to “strengthen” the structures of the living valve).
However, in most cases, prolapses do not require treatment, or treatment is limited to long-term intake of adequate (about 300 mg per day) magnesium preparations, which allows in the long term to normalize collagen metabolism and “strengthen” the structure of the valve. Taking magnesium supplements and mild herbal sedatives can also reduce the subjective unpleasant manifestations of vegetative-vascular dystonia, which often accompany prolapse.
In our clinic you can undergo a full range of examinations and receive advice on assessing the severity and need for treatment of prolapses.
Lifestyle
To improve your quality of life if you have aortic valve regurgitation, your doctor may—in addition to other treatments—may recommend:
- Monitor increases in blood pressure.
Reduces blood pressure, reduces the load on the aortic valve. - Eat less salt.
Reducing your salt intake helps you keep your blood pressure within a normal range, which is very important if you have aortic valve regurgitation. - Visit your dentist regularly.
Follow your care instructions. - Maintain a healthy weight.
Maintain your weight within the range recommended by your doctor. Excess weight puts extra work on your heart. - Exercise.
Perform the exercise as recommended by your doctor. He or she may recommend a program of specific intensity depending on the severity of your aortic valve regurgitation. Exercise alone will not improve your condition, but it can help lower your blood pressure. Exercise also helps maintain overall fitness, which will aid in recovery if you need heart surgery. - Visit your doctor regularly.
Set up a regular schedule for visiting your cardiologist or your primary care physician.
If you are a woman of childbearing age with aortic valve regurgitation, discuss pregnancy and family planning with your doctor because your heart will work harder during pregnancy. How much extra work your heart can do with aortic valve regurgitation depends on the degree of regurgitation and how well your heart contracts. If you become pregnant, you will need care from your cardiologist and obstetrician during pregnancy, labor, and postpartum.
What is the clinical picture of prolapse?
Typically, valve prolapse (mild degrees) is asymptomatic. It is possible to combine valve prolapse with clinical manifestations of vegetative-vascular dystonia (pain in the left half of the cell, mild rhythm disturbances (tachycardia and extrasystole), surges in blood pressure, panic attacks). The causes of vegetative-vascular dystonia (a diagnosis that European and American cardiologists easily dispense with) are very closely related to the cause of prolapse (both collagen synthesis and normal processes in the nervous system are disrupted due to magnesium deficiency in the body).
1 MedicCity cardiologist performs echocardiography with Doppler color mapping
2 A MedicCity cardiologist diagnoses heart valve prolapse using a VIVID i ultrasound scanner
3 MedicCity cardiologist performs echocardiography with Doppler color mapping