Etiology:
- Inflammatory lesions: rheumatism, systemic scleroderma, aortoarteritis.
- Degenerative processes: myxomatous degeneration.
- Atherosclerosis.
- Infectious processes: infective endocarditis.
- Congenital pathology: bicuspid aortic valve.
There is a tendency to increase the frequency of involutional (degenerative-atherosclerotic) causes of aortic stenosis, which has led to an increase in age patients over 60-65 years of age requiring surgical correction of aortic disease.
With congenital or rheumatic valve damage, a long latent period without clinical manifestations is observed. Mortality and the risk of complications increase significantly with the onset of symptoms of the disease. With angina pectoris, fainting and manifestations of heart failure caused by systolic dysfunction of the left ventricle, the average life expectancy is 5, 3 and 2 years, respectively. In asymptomatic patients, the risk of sudden death is low (even with severe aortic stenosis), while in the presence of symptoms, 15–20% of patients die suddenly.
General information
Aortic stenosis occupies a leading position among all heart defects in the adult population (20-25% of all heart defects ).
Males are most often affected. The disease progresses slowly, the symptoms increase gradually, which is due to the well-developed muscular layer of the left ventricle, which is able to compensate for the increased pressure for quite a long time. Aortic stenosis refers to a narrowing of the area of the outflow tract in the left ventricle - the place where the aorta itself exits the heart. Changes can form as a result of calcification of the valve leaflets or be congenital. One way or another, all changes create a barrier when pushing blood out of the heart.
Isolated aortic valve stenosis is extremely rare - no more than 4% of the total. Most often, aortic stenosis is combined with other heart defects. Deformation of the aortic valve occurs as a result of destructive processes in the tissues of the valve itself; extremely rarely, it is a congenital anomaly.
Rate of progression of aortic valve damage:
- mild aortic stenosis
(aortic valve opening area -1.2 - 2 cm2) becomes severe, requiring aortic valve replacement, over 10 years - in 10% of patients, over 25 years - in 38%; - with moderate asymptomatic aortic stenosis
(the area of the aortic valve opening is 0.75 - 1.2 cm2), aortic valve replacement is required after 10 years in 25% of cases; - asymptomatic severe aortic stenosis
(aortic valve opening area <0.75 cm2) usually progresses more quickly; 30–40% of patients develop symptoms within 2 years and there is a need for aortic valve replacement.
Atrial fibrillation, aortic regurgitation (spontaneous or caused by infective endocarditis), mitral regurgitation, and acute myocardial infarction accelerate decompensation.
In uncomplicated aortic stenosis, the characteristic auscultatory picture is: systolic murmur at Botkin’s point and at the base of the heart on the right, carried out to the vessels of the neck, weakening of the 2nd sound due to the aortic component. The intensity of the systolic murmur may decrease with the development of left ventricular systolic dysfunction and is not a criterion for the severity of the defect. Often the course of aortic stenosis is complicated by pathology of the mitral valve (“mitralization”).
Pathogenesis
With stenosis of the left ventricular outflow tract, a barrier to blood flow is created and during systole the left ventricle forms high pressure at the level of the aortic valve. To maintain the required blood volume, the body has to increase the heart rate, shorten diastole (the time of relaxation and recovery of the myocardium) and lengthen the period of blood expulsion from the cavity of the left ventricle. As a result of insufficient emptying of the left ventricle, end-diastolic intraventricular pressure increases. All this leads to the formation of hypertrophied myocardium of the left ventricle of the concentric type (thickening of the muscle layer near the aortic valve).
Thanks to good compensatory capabilities, the heart can maintain adequate hemodynamics for quite a long time. With advanced aortic stenosis, the hypertrophied organ can grow to enormous sizes. Over time, the hypertrophied left ventricle stretches, its dilation forms, and the blood circulation decompensates. Failure of compensatory mechanisms occurs as a result of the development of the inability of blood vessels to provide the heart muscle with the necessary amount of oxygen and nutrients. All this leads to the development of pulmonary hypertension and congestion in the systemic circulation.
Diagnosis of aortic stenosis
- ECG;
- Chest X-ray;
- Coronary angiography - performed when there are indications for surgical treatment or suspected coronary atherosclerosis;
- MSCT of the ascending aorta with contrast – indicated for poststenotic dilatation of the aortic root;
- EchoCG. Echocardiography allows you to determine: the structure of the valve (bicuspid valve, thickening of the leaflets, fibrosis, calcification, vegetation), the nature of its movement (leaf mobility, degree of opening) and the area of the opening; changes in the aortic root (poststenotic dilatation), left ventricular volume, severity of left ventricular hypertrophy, disturbances of local contractility of the left ventricle (indicating coronary artery disease), EF, left atrium volume, condition of other valves. Doppler studies can accurately determine the pressure gradient between the aorta and left ventricle.
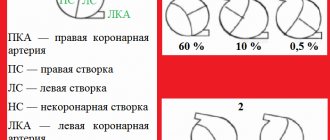
Echocardiographic criteria for the severity of aortic stenosis, taking into account the area of the aortic valve (normal area is 3–4 cm2):
- moderate stenosis 1 – 1.4cm2
- severe stenosis < 1 cm2
- critical stenosis < 0.75 cm2
The average systolic gradient between the aorta and LV at the level of the aortic valve is less than 50 mm Hg. Art. – hemodynamically insignificant aortic stenosis, 50 – 80 mm Hg. – moderate aortic stenosis, more than 80 mm Hg. – severe aortic stenosis.
Indications for surgical treatment (prosthetics) of aortic stenosis
(American Heart Association, American College of Cardiology)
Classification of recommendations and levels of evidence in ACC/AAC format:
- Class I: Conditions for which there is evidence and/or general agreement that a procedure or treatment is beneficial, useful and effective.
- Class II: Conditions for which there is conflicting evidence and/or differences of opinion about the usefulness/efficacy of a procedure or treatment.
- Class IIA: Weight credibility/opinion in favor of usefulness/effectiveness.
- Class IIB: Benefit/effectiveness less well established by evidence/opinion.
- Class III: Conditions for which there is evidence and/or general consensus that the procedure/treatment is not beneficial, not effective, and in some cases may be harmful.
In addition, the levels of evidence to support the recommendations are outlined as follows:
- Level of Evidence A: Data are from multiple randomized clinical trials.
- Level of Evidence B: Data are from single randomized trials or non-randomized trials.
- Level of Evidence C: Expert consensus only, individual case studies and standards of care.
CLASS I
- 1. Aortic valve replacement is indicated in symptomatic patients with severe aortic stenosis (Level of Evidence: B).
- 2. Aortic valve replacement is indicated for patients with severe aortic stenosis during coronary artery bypass grafting (CABG). (Confidence level: C).
- 3. Aortic valve replacement is indicated for patients with severe aortic stenosis, during surgery on the aorta or other heart valves. (Confidence level: C).
- 4. Aortic valve replacement is indicated for patients with severe aortic stenosis and LV systolic dysfunction (EF less than 50%). (Confidence level: C).
CLASS IIA
Aortic valve replacement is indicated for patients with moderate aortic stenosis, undergoing CABG surgery, surgery on the aorta or other heart valves. (Confidence level: B).
CLASS IIB
- 1. Aortic valve replacement is indicated for asymptomatic patients with severe aortic stenosis and an abnormal response to exercise (eg, the development of symptoms of hypotension). (Confidence level: C).
- 2. Aortic valve replacement is indicated for older patients with severe asymptomatic aortic stenosis if there is a high likelihood of rapid progression (age, calcification). (Confidence level: C).
- 3. Aortic valve replacement is indicated for patients with mild aortic stenosis during CABG surgery, when there are signs of moderate to severe valve calcification, which can lead to rapid progression. (Confidence level: C).
- 4. Aortic valve replacement is indicated for asymptomatic patients with extremely severe aortic stenosis (aortic valve area less than 0.6 cm2, mean gradient more than 60 mmHg and flow velocity more than 5.0 m/s), when the expected operative mortality of patients is less than 1.0%. (Confidence level: C).
CLASS III
- 1. Aortic valve replacement is not indicated for the prevention of sudden death in asymptomatic patients with aortic stenosis who do not have any of the indicators from the list of Class IIA/IIB recommendations. (Confidence level: B).
- 2. In older patients with severe, symptomatic, calcific aortic stenosis, aortic valve replacement is the only effective treatment.
- 3. Young patients with congenital or rheumatic aortic stenosis may be candidates for valvotomy. Although there is no consensus regarding the optimal timing of surgery in asymptomatic patients, reasonable recommendations can be made for most patients.
Aortic valve replacement
In recent years, significant progress has been made in the surgical treatment of heart valves. Improvements in technology (including artificial blood circulation machines), the development of uniform standards and protocols for both preoperative examination and the course of the operation have made it possible to reduce the risks of perioperative complications, making the operation on the heart valve apparatus safer than refusing surgery and trying to live with valve dysfunction.
Types of surgical treatment: heart valve replacement surgery
In principle, there are two types of heart valve surgery: prosthetics with an artificial or biological prosthesis and repair of your own valve. It is quite natural that a person’s own valve, after successful reconstruction, functions better than an artificial prosthesis. But if it is impossible to preserve your own valve, the only way out is to replace it with a prosthesis.
Types of valves used in prosthetics
- Biological valves.
They can be made from animal or human tissues (heterografts, homografts, autografts). Biological valves may contain some artificial components to provide valve support and placement. The main advantage of such a valve is the absence of the need for lifelong anticoagulant therapy (constant strict use of drugs that significantly thin the blood and require constant blood tests), and the main disadvantage is its limited service life (15 - 20 years). - Mechanical valves
. They consist entirely of mechanical elements (titanium and pyrolytic carbon) and are designed to replace the patient's own valve functions. The mechanical valve is very reliable and durable, designed for many years of full-fledged operation, which is the main advantage, but requires the patient to constantly take anticoagulants.
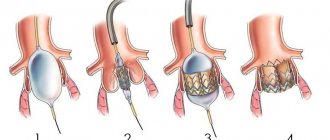
When replacing the aortic valve, access to the valve is achieved by dissecting the aorta in the ascending section (transverse aortotomy). After excision of the aortic valve leaflets and thorough decalcification of the fibrous ring, the latter is sutured with U-shaped sutures. In order to prevent the annulus fibrosus from cutting through, the seams are reinforced with Teflon gaskets. To select the size of the implanted prosthesis, the diameter of the fibrous ring is measured with special calibrators. The selected prosthesis is implanted in the aortic position by stitching its braid. After fixing the prosthesis, the mobility of the locking elements of the mechanical prosthesis or the coaptation of the biological valve leaflets is assessed. If there are no restrictions on their mobility, the dissected aorta is sealed with two rows of sutures.
Risk factors for carotid atherosclerosis
Risk factors for carotid artery disease are similar to those for other types of cardiovascular disease. They include:
- Age
- Smoking
- Hypertension (high blood pressure) is the most important risk factor for stroke
- High cholesterol
- Diabetes
- Obesity
- Sedentary lifestyle
- Family history of atherosclerosis
Men under 75 years of age have a greater risk of developing carotid artery stenosis than women in the same age group. In the group over 75 years of age, women have a greater risk of stroke. In patients suffering from coronary artery disease, narrowing of the carotid artery is often detected.