Aortic valve disease: features of its course and treatment
According to statistics, disorders of the cardiovascular system have become increasingly observed in people over 30 years of age. There are many reasons that provoke pathologies. If some diseases are treatable and, by removing provoking factors, one can achieve normalization of health, then others accompany the patient throughout his life and can significantly shorten his life.
Aortic valve disease is a serious pathology. More often requires surgical intervention. It can be congenital or acquired. Appears as a result of narrowing of the aortic mouth or incomplete closure of its valve.
Causes and symptoms
There are no exact statistics on the prevalence of the disease by age group and gender, but cardiologists note that it is detected several times more often in women than in men. The peak number of patients is observed among people of older retirement age. The main reasons may be:
- leaflet calcification;
- progression of rheumatism;
- idiopathic dilatation of the aorta;
- arterial hypertension and endocarditis;
- aneurysm;
- congenital defect of the aortic valve.
Chest trauma, arthritis, syphilis and some pathologies that develop in a person over a long period of time can also give impetus to the appearance or progression of disruption of the normal functioning of the organ.
8
24/7
Degrees
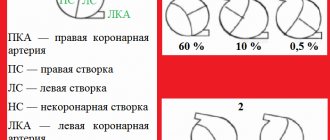
The risk to the patient's health and the need for surgery depends on the degree of aortic regurgitation.
| Stage | Amount of thrown blood, % | Prosthetics |
| First, full compensation | no more than 15 | Not required |
| Second, hidden CH | from 15 to 30 | Required under certain conditions |
| Third, relative coronary insufficiency | up to 50 | |
| Fourth, severe left ventricular failure | more than 50 | |
| The issue is resolved individually | Not required due to its uselessness. |
Depending on the degree, the valves are deformed and the quantitative volume of blood entering the heart through the aorta changes. The initial, first stage of the disease is virtually impossible to determine. The patient’s symptoms are completely absent or feel like side effects of other diseases. This occurs because the heart adjusts to the change in volume and compensates for it.
Symptoms
As the pathology develops, the organ ceases to cope with its functions, and symptoms characteristic of aortic valve disease appear:
- tinnitus and dizziness when moving or changing position;
- increased heartbeat, pronounced pulsation in the blood vessels;
- shortness of breath, fatigue, fainting and pre-fainting states, nausea;
- a pressing feeling of heaviness in the right hypochondrium, as well as swelling of the lower extremities;
- coughing attacks when lying down, standing, feeling of constant weakness.
Due to a lack of oxygen, a person’s complexion becomes pale gray, a bluish tint to the lips is observed, and typical circles appear under the eyes. Also, when examining a patient, the cardiologist examines the presence and severity of symptoms:
- the difference between the upper and lower blood pressure readings;
- pulsation on the carotid arteries, uvula and tonsils;
- reaction of the pupils to heart contractions, heart murmurs;
- changes in the size of the organ, protrusion in the chest area.
Diagnostics
Accurate diagnosis of the disease can only be made on the basis of objective data, a complete cardiac examination, biochemical blood test and a number of other tests.
Based on the presence of clinical symptoms, the severity of the defect, and the severity of aortic insufficiency, a decision about surgery is made. In elderly patients, due to the low contractility of the organ, the functional impairment is almost invisible. The severity of the pathology can be determined after studying the area of the hole in relation to the blood flow. Arterial insufficiency is determined by the indicator of reverse blood flow.
By listening, a cardiologist can determine the onset of development of bicuspid aortic valve disease:
- with stenosis, a systolic murmur is characteristic with a weakening of the 2nd tone in the aorta;
- Insufficiency is indicated by a murmur during diastole.
It is necessary to study the functioning of the heart by:
- ECG;
- X-ray examination;
- MRI to exclude coronary insufficiency and other pathologies.
However, the basis for choosing treatment is echocardiography.
When diagnosing, an accurate description of the patient’s feelings is of great importance, so before the appointment, you can write down all the complaints and let the doctor read them.
8
24/7
Treatment at different stages
Depending on the cause, extent, stage of aortic valve disease and other factors, different treatment methods may be used. The patient must be regularly observed by a specialist and undergo the examinations prescribed by him. In the absence of obvious symptoms:
- mild defect – once every 3 years;
- moderate form – once every 24 months;
- severe degree - annually, sometimes more often.
The following medications are prescribed:
- rheumatic nature of the disease - antibiotics;
- arterial hypertension - to normalize blood pressure.
Surgical intervention is not required, only constant monitoring by the attending physician is required.
If clinical complaints appear, to alleviate the patient’s condition in the preoperative period or if surgery is impossible, the following is prescribed:
- inhibitors, diuretics, nitrates;
- vasodilators and beta blockers;
- drugs that improve blood circulation.
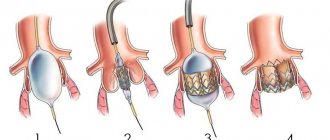
A timely operation can help completely get rid of aortic valve disease. When blood reflux in an amount not exceeding 30% and slight deformation of the valves, intra-aortic balloon counterpulsation is recommended. In case of severe structural changes that allow more than 30% blood flow, implantation is required.
Surgery
In a person with heart disease, the bicuspid aortic valve requires replacement or replacement in several cases.
| Diagnosis | Cause |
| Severe stenosis | Complaints of severe pain and worsening condition. |
| Associated ischemia requiring coronary artery bypass grafting. | |
| Additional pathological changes in the organ requiring surgical intervention. | |
| The ejection fraction with cardiac contractility is below 50%. | |
| Severe valvular insufficiency | Clinical manifestations of the disease. |
| Surgery is required for other diseases of the organ. | |
| A decrease in ejection fraction in the absence of complaints from the patient. | |
| Too much enlargement of the ventricles. |
Surgical intervention is mainly performed after 30-35 years, but with the accelerated development of the disease it can take place at any time. The number of contraindications to prosthetics is minimal. They are:
- decompensated diabetes;
- oncological diseases;
- post-stroke condition;
- exhaustion and anemia.
For each patient, his condition is predicted at the time of the operation and during the rehabilitation period. Depending on this, a conclusion is given about the possibility of returning to normal life.
Forecast
The construction of treatment plans for the disease and the choice of methods occurs after diagnosis and identification of the severity of the aortic valve defect.
Mild hypertrophy with strong obstruction of blood flow leads to a decrease in the number of heart contractions and, accordingly, gradually reduces the therapeutic effect of surgery.
The process of hypertrophy allows, at a certain stage of the disease, to stabilize the functioning of the heart, but at the same time it can cause the development of angina pectoris and increase the likelihood of a heart attack.
If aortic heart valve disease developed asymptomatically, and then its rapid progression began, then the subsequent life expectancy of a person is no more than 3 years.
Risk factors and disease prevention
Aortic valve defects can be divided into 2 groups.
| View | Development time | Cause |
| Congenital | During intrauterine development of the fetus at 2-8 weeks of formation. | Genetic predisposition. Radiation exposure, rubella and other viral infections. Smoking, alcohol and drug addiction of the mother. |
| The defect becomes noticeable as the child grows. | The presence of a muscle cushion above the AC. The valve design is two- or single-leaf rather than three-leaf. Under the valve there is a membrane with a hole. | |
| Acquired | Any age | Infectious diseases that lead to microorganisms entering the organ. The subsequent appearance of a colony of connective tissue at the site of localization leads to deformation of the valves. |
| Autoimmune diseases become an impetus for the fusion of pouches and changes in the aortic mouth. | ||
| Age-related disorders, mainly calcification of the edges of the valves and the growth of fatty plaques, lead to closure of the lumen. |
There are no preventive measures that guarantee complete protection against the disease, but the following help reduce the risk:
- timely treatment of streptococcal infections;
- if you have rheumatism, constant monitoring by a specialist;
- taking certain groups of antibiotics and other drugs prescribed by a cardiologist;
- complete exclusion of alcohol, drugs and smoking;
- engaging in acceptable forms of exercise.
Aortic valve disease needs to be treated using scientific methods of therapy. Traditional methods do not have the desired effect and can lead to missed deadlines when the disease can be cured. Therefore, in case of any deviations, medical attention is needed.
8
24/7
Symptoms
The symptoms of aortic stenosis and aortic valve regurgitation are similar and involve chest pain during exercise that is relieved by rest. There are also several different symptoms.
Aortic stenosis can cause:
- swelling of the ankles;
- fatigue;
- shortness of breath;
- rapid pulse.
Aortic valve insufficiency causes the following symptoms:
- fainting, usually occurring during physical activity;
- cough;
- cardiopalmus.
Both pathologies occur without symptoms for a long time, often the first signs of the disease appear only after several years. If you have these symptoms or at least one of them, you should consult your doctor.
Methods for diagnosing heart defects
In order to establish a diagnosis of heart disease, an anamnesis is collected, the presence of diseases that could lead to deformation of the heart valve is revealed: rheumatic diseases, infectious, inflammatory processes, autoimmune diseases, injuries.
- The patient must be examined to identify the presence of shortness of breath, cyanosis, edema, and pulsation of peripheral veins. Using percussion, the boundaries of the heart are identified and sounds and murmurs in the heart are listened to. The size of the liver and spleen is determined.
- The main method for diagnosing valve pathology is echocardiography
, which allows you to identify the defect, determine the area of the opening between the atrium and the ventricle, the size of the valves, cardiac fraction, pressure in the pulmonary artery.
More accurate information about the condition of the valves can be obtained by performing transesophageal echocardiography. - Electrocardiography is also used in diagnostics, which allows one to assess the presence of atrial and ventricular hypertrophy and identify signs of overload of the heart. Daily Holter ECG monitoring allows you to identify rhythm and conduction disturbances.
- Highly informative methods for diagnosing heart defects are cardiac MRI or cardiac MSCT. Computed tomography scans provide precise and numerous sections, which can be used to accurately diagnose the defect and its type.
- Laboratory tests play an important role in diagnosis, including urine and blood tests, determination of blood sugar, cholesterol levels, and rheumatoid tests. Laboratory tests allow us to identify the cause of the disease, which plays an important role in subsequent treatment and patient behavior.
Reasons for development
As already noted, aortic defects can be congenital or acquired.
As for the first options, it is rarely possible to identify a specific cause for the violation of embryogenesis. However, there are certain risk factors that every pregnant woman should be aware of:
bad habits (smoking, alcoholism);- infectious diseases (including such “harmless” ones as influenza);
- taking medications;
- strong psycho-emotional and physical stress;
- polluted environment;
- X-ray examinations.
The pathogenesis of the disease is as follows:
- one valve may be underdeveloped;
- a hole forms in one of the valves;
- A bicuspid valve is formed instead of a tricuspid valve.
Acquired defects usually develop as a result of previous illnesses.
Infectious diseases (sepsis, tonsillitis, syphilis and other sexually transmitted diseases). In this case, bacteria, entering the endocardium with the bloodstream, damage the structure of the valves
Autoimmune pathologies (rheumatism, systemic lupus erythematosus). The defect is formed due to the fact that immune cells begin to attack their own body, in this case the aortic tissue. As a result, a degenerative process develops and valve damage occurs.
Atherosclerosis. It develops in older people, when calcium salts settle on the valve flaps and plaques form. As a result, their mobility decreases.
Chest injuries. The reason is rare, but still occurs. Valves are deformed due to direct mechanical impact.
It is worth noting that these factors can also cause the development of other defects, such as mitral (bicuspid valve defect) or tricuspid.
conclusions
Aortic valve defects are fairly common diseases that can be either congenital or acquired. Impaired blood flow due to damage to the valves can lead to the development of chronic heart failure.
The symptoms that arise from aortic valve disease are not specific enough, but modern diagnostic methods can easily detect them.
In the absence of significant contraindications, surgical treatment of this disease gives a good result. The prognosis for life and work ability is favorable.
Patient monitoring
Valve defects are a very insidious disease that can hardly manifest itself, and then lead to the development of heart failure. In addition, a blurred clinical picture makes it difficult to make a correct diagnosis.
Auscultation of aortic heart defects is the simplest screening method. If you hear pathological noises, you should immediately send the patient for further examination.
Therefore, if you have been diagnosed with this pathology, you need to take preventive examinations as responsibly as possible. You should undergo echocardiography and other examinations prescribed by your doctor at least once every six months.