VEIN PULSE
The venous pulse, as already mentioned, compared to the arterial pulse is a phenomenon of a completely different order. There are still a number of ambiguities in its interpretation and the reasons for the appearance of individual waves. Many adhere to the point of view of Fredericqs, who believed that the venous pulse is an expression of changes in pressure in the right atrium. However, there is reason to believe that the origin of venous pulse waves depends on other reasons. If the venous pulse is simultaneously recorded on the right and left jugular vein, then the resulting curves in most cases are not quite similar (see Fig. 68), which should not be observed if the cause of origin depended on changes in pressure in the right atrium. In the presence of significant venous stasis, the veins appear strongly swollen, but their pulsation in these cases is rather weakly expressed. If it depended on changes in pressure in the atrium, then when the veins were filled with blood, the transmission of oscillations from the atria to the periphery should have been facilitated.
Rice. 68
A different idea about the causes of venous pulse is much more correct. It must be assumed that the venous pulse is not an expression of changes in pressure in the vein, but depends on fluctuations in the degree of filling of the venous trunk with blood. The arterial pulse expresses changes in pressure and depends on them, the venous pulse expresses changes in volume. For clarification, an analogy can be drawn between the flow of blood in a venous bed and the flow of water in a river. The flow of blood in large venous trunks occurs passively, in a continuous stream, due to the existence of a small difference in pressure in the central and peripheral sections of the system, i.e., in a causal sense, the phenomenon is quite similar to the flow of water in a river bed. If an obstacle to the free flow of water (a dam) arises in the river bed, the water level in the river will begin to rise quickly, and when the obstacles are removed, it will also quickly fall. Level fluctuations will be in the nature of volumetric changes.
Rice. 69
At the moment of atrial systole, an obstacle arises to the free flow of blood from the veins, therefore the degree of filling of the venous trunk increases and its volume quickly increases. In this case, the pressure does not noticeably increase, since, in contrast to the arteries, the vein wall does not present any obstacles, easily stretches and accommodates an excess volume of fluid. Of course, the degree of adaptability of the venous bed has its limits, and when it is overfilled with blood, the pressure in the veins can also increase.
When simultaneously recording the venous pulse and heart sounds, it can be noted that, somewhat preceding the first tone, a wave with a rather steep rise appears on the venous curve. Following the sharp peak there is also a rather steep drop, ending at the time the vibrations of the first tone disappear (see Fig. 69). The common name for this first wave of the venous pulse is the atrial wave, and is usually designated as a (atrium) on the waveforms. It would be more correct to call it a presystolic wave, especially since it is somewhat delayed compared to the moment of increase in pressure in the right atrium. Contraction of the atria stops the smooth flow of blood from the large veins and is therefore only an indirect cause of the appearance of the presystolic wave, but since this wave is closely related to atrial systole, the name “atrial wave” assigned to it is very convenient. If the functioning of the atria is disrupted with an isolated increase or decrease in the number of their contractions compared to the number of ventricular systoles, usually corresponding changes can be observed in the atrial or presystolic wave.
Following the atrial wave, one would theoretically expect a uniform fall in the presystolic rise. However, in most cases, the downward part of the curve is interrupted by a new, sometimes very significant, rise - a tooth. Some believe that the cause of the appearance of the tooth is the push from the closure of the tricuspid valve (Edens, Rihl). The generally accepted interpretation, however, has become widespread since the time of Mekenzie, who considered the cause of the origin of this rise to be the impulse of the arterial wave transmitted to the column of blood filling the large veins. This tooth is called systolic or carotid and is designated on the curves by the letter c (carotis). It exactly coincides with the moment the wave appears in the carotid arteries and is somewhat delayed compared to the moment the tricuspid valve closes. When experimentally closing art. anonyma, at the place of its origin from the aortic arch, the tooth sharply decreases in size, and the time of its appearance is somewhat delayed. The latter must be explained by the fact that normally the transmission of the impulse from the carotid artery to the jugular vein occurs directly, but when the art. anonyma the wave must reach the cervical part of the vein from more distant parts of the venous system, and the speed of its propagation in the veins is much slower than in the arteries.
Directly after the systolic rise is followed by a rapid and deep decline of the curve, the so-called systolic collapse. This negative wave has great diagnostic value. With a normal venous pulse, the deepest part of the systolic delay is located at a distance of 1/50 of a second after the second tone and, therefore, just coincides with the end of systole, since it is necessary to take into account some delay in its appearance on v. jugularis. Following the end of systole of the right ventricle, the tricuspid valve opens, and the crown accumulated during the systolic period from the right atrium immediately passes into the right ventricle. This causes a decrease in resistance to blood flowing from the veins, and some collapse of the venous trunks occurs. In addition, it is also assumed that following ventricular systole, the volume of the organs filling the chest cavity decreases somewhat due to the volume of blood ejected by the heart, which should lead to a slight drop in pressure in the chest cavity and, consequently, to a more vigorous flow of blood from the nearest venous reservoirs. Probably both of these reasons play a role in the origin of systolic collapse.
During the diastolic period, the venous pulse curve slowly rises upward and sometimes gives a slight depression before the onset of the presystolic wave, often turning into wave a with almost no noticeable boundary. The diastolic wave is usually denoted by the letter v or d (venticulus - diastolische Welle); Some authors distinguish in it several individual peaks (3), which, however, have no practical significance and are rarely clearly outlined. The reason for the diastolic rise in the venous curve is most understandable. During the diastolic period, the right half of the heart gradually fills. As its cavities are filled, the resistance to blood movement in the nearest vein trunks increases, and the degree of their filling also gradually increases. This leads to the formation of a sloping rise, called the diastolic wave. The sometimes observed appearance of 3 small waves on the diastolic rise is explained by an uneven and successive separate period in the filling of the right ventricle, right atrium and venous sinus.
These are the main points of a normal venous pulse. In addition to the main passive mechanism of its origin, it is also distinguished from the arterial pulse by the fact that it is affected by the work of not only one ventricle, but also the atrium. Therefore, with arrhythmias, with various kinds of dissociations in the work of the cavities of the heart, these disorders affect the venous curve to a much greater extent than the arterial one. In many cases, the venous pulse curve may be sufficient to resolve the issue of an existing cardiac arrhythmia.
With valvular defects of the left heart, the venous pulse curve does not experience significant deviations from the norm. Valvular defects of the right heart distort it significantly.
With valvular defects of the left heart, changes in the form and time of appearance of systolic retraction are most often observed. This is explained by the phenomena of stasis in the pulmonary circulation and difficulties in emptying the right ventricle. First of all, the magnitude of the systolic retraction decreases, and the maximum retraction appears earlier than usual. Such changes are most often observed with stenosis of the left venous orifice, adhesive pericarditis, arteriosclerosis, nephritis, and emphysema. The presystolic wave, on the contrary, is often larger than normal in size.
With defects of the tricuspid valve, its insufficiency, the venous pulse is distorted to the greatest extent. A so-called positive venous pulse appears. When tricuspid valve insufficiency occurs, blood flows back from the right ventricle into the right atrium. The valves located at the opening of the vena cava in the right atrium are so weak that even with small degrees of insufficiency of the sail valve, they become insufficient, and the blood flow from the right ventricle through the atria easily penetrates into the central veins, creating an active back wave. The normal venous pulse is called atrial or negative due to the passivity of its origin. When the valves of the right venous orifice are insufficient, the pulse becomes active and is therefore called the ventricular or positive venous pulse. This is reflected in the curve by the disappearance of systolic collapse; wave (c) often directly merges with the diastolic wave (v), which shortens and loses its sloping character; the atrial wave is often also more pronounced (see Fig. 70). Wave v, merging with the carotid one and acquiring a sharp apex, seems to move towards the systolic period of the curve. During the diastolic period, the curve does not have a rising, but a falling direction. In cases of a pronounced positive venous pulse, we have only two waves with sharp peaks: wave (a) and wave (c + v). Sometimes you can see the appearance of a small wave between (a) and (c), the so-called tricuspid insufficiency wave (I). A positive venous pulse can often be diagnosed by simply examining the patient and feeling the pulsating vessels of the neck v. jugularis and art. carotis. Venous pulsation is very pronounced and gives the impression of a simultaneous impulse in both the carotid and jugular veins.
Rice. 70
A positive venous pulse is often transmitted very far along the venous trunks, since weak venous valves quickly succumb to strong back-pulses of blood, and the wave can reach the branches of v. porta in the liver, causing pulsation of the organ throughout its entire mass. The so-called hepatic pulse is always the result of a positive venous pulse and a sure sign of tricuspid valve insufficiency. With an enlarged right ventricle, shocks from its contraction can also be transmitted directly to the liver, and they will also be synchronous with the contractions of the ventricle, but when recording the pulse, wave (c) of the hepatic pulse will always be delayed compared to that on v. jugularis. With increased epigastric pulsation, it will correspond in position to wave (c) v. jugularis, since the transmission of the impulse from the right ventricle of the liver occurs directly in the latter case. In addition, since with true pulsation of the liver the organ is greatly enlarged, then, by grasping it with both hands from the front and back surfaces, you can feel how it resounds in its entire mass with each pulse impulse.
When the heart rhythm is disturbed, depending on the nature of the dissociation, in the work of various parts of the heart, either a mutual displacement of individual waves of the venous pulse or an increase in their number is observed. It is more convenient to consider these changes simultaneously with analysis of the electrocardiographic curve, since the latter is the most accurate and subtle method for diagnosing heart rhythm disorders.
24video
Heart sinking
Atherosclerosis
Menopause
38265 20 October
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Fading of the heart: causes of occurrence, what diseases it occurs with, diagnosis and treatment methods.
Description
Fading of the heart is a subjective feeling of the absence or skipping of another heartbeat in a certain period of time, accompanied by unpleasant sensations in the heart area, in some cases, dizziness and darkening of the eyes. Heart stopping is a symptom of a wide range of diseases: from the most harmless ones that do not require treatment to serious pathologies that require medical intervention.
Types of heart palpitations
Normally, the heart contracts rhythmically, at approximately equal intervals. The contraction frequency ranges from 60 to 100 beats per minute.
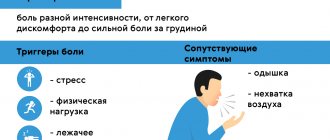
There are several types of heart failure:
- Fading of the heart due to a compensatory pause during extrasystole. There is a sensation of a strong or double heartbeat against the background of a normal rhythm, followed by a short pause felt by the patient.
- Varying intervals between contractions can also cause the heart to feel as if it is stopping (common with atrial fibrillation).
- Pauses of the heart due to blockade of impulses.
- Feeling of freezing with reduced pumping function of the heart (with severe heart failure).
Possible causes of heart failure
First, we list the most common risk factors for cardiac problems:
- Smoking
is one of the main risk factors for cardiovascular disease. This also includes alcohol, caffeine and drugs. - High levels of “bad” cholesterol
- intermediate, low and very low density lipoproteins (IDL, LDL, VLDL). - High blood pressure
.
The feeling of interruptions and pauses in the work of the heart in most cases is caused by extrasystoles, or premature contractions of the heart.
Extrasystoles are often observed in completely healthy people, while there are no signs of myocardial dysfunction, and correction is not required.
However, if attacks of extrasystole exceed the permissible norms per day (diagnosis is carried out using daily ECG monitoring), additional examination and treatment are required.
Less commonly, the cause of heart failure is atrial fibrillation (atrial fibrillation) or blockade of the conduction system of the heart. Atrial fibrillation occurs when the electrical activity of the atria is disrupted with the occurrence of a large number of impulses and chaotic contraction of the atria.
Only a portion of the impulses pass to the ventricles of the heart in an irregular rhythm - hence the fading of the heart, as well as other unpleasant sensations.
Atrial fibrillation can occur in the form of attacks (paroxysms), or it can be permanent. The diagnosis is made based on the results of the ECG.
Blockades of the conduction system of the heart, depending on the severity, manifest themselves in different ways: from asymptomatic to loss of consciousness. Feelings of heart stopping most often occur with 2nd degree atrioventricular block.
There is a gradual depletion of the atrioventricular (AV, AV) node, a decrease in the ability to conduct impulses, and a kind of pause occurs, which the patient clearly feels.
Causes of disturbances in the structure of the conduction system of the heart:
- myocardial infarction with subsequent replacement by connective tissue of destroyed heart structures, including important bundles that conduct electrical impulses from the sinus node;
- coronary heart disease, when due to atherosclerosis of the coronary arteries, adequate blood supply to the myocardial areas in the area of the conduction bundles is disrupted and sclerodegenerative fibrosis (replacement with connective tissue) of the affected tissue areas develops;
- myocarditis (inflammatory damage to the heart muscle);
- dilated and hypertrophic cardiomyopathy;
- congenital anomalies of the structure of the conduction system of the heart.
Sick sinus node syndrome (SSNS) is a rare condition caused by a decrease in the functional ability of the sinus node to act as the main pacemaker and ensure regular conduction of impulses to the atria, which predetermines the appearance of cardiac slowdown and accompanying arrhythmias.
Patients often complain of dizziness, poor exercise tolerance, shortness of breath on exertion, fatigue and episodes of weakness.
Many cardiac problems, which at first glance are not related to rhythm disturbances, can ultimately lead to the appearance of various arrhythmias, accompanied by a feeling of cardiac arrest. For example, with hypertension, the myocardial wall thickens and the nutrition of heart cells is disrupted, which leads to the appearance of ectopic (irregular) impulses. With various defects of the valve apparatus, without treatment, a gradual change in the structure of the heart muscle occurs with the appearance of connective tissue and disruption of the normal conduction pathways of the heart.
Among the non-cardiological reasons for the feeling of heart failure, it is worth noting the menopause, which is accompanied by changes in hormonal levels and various unpleasant sensations and discomfort not associated with disturbances in the functioning of the heart.
Hypothyroidism may cause a slow heartbeat (bradycardia) and a feeling of pauses in the heart. This is due to insufficient levels of thyroid hormones.
During intoxication (during infectious diseases, with severe sweating, vomiting and diarrhea), a loss of electrolytes (potassium, sodium and magnesium ions) occurs, which leads to disruption of the water-salt balance in the body and the occurrence of various rhythm disturbances.
Taking certain medications may be accompanied by a slower heart rate, slower impulse conduction, and a feeling of heart stopping. These drugs include cardiac glycosides, beta-blockers, calcium channel blockers, sympatholytic agents, antidepressants, and narcotic analgesics.
In persons with a labile psyche and frequent emotional experiences, a subjective feeling of discomfort in the chest area and cardiac arrest without visible organic pathology is possible.
Which doctors should I contact?
If various disturbances in the functioning of the heart occur, you should consult a cardiologist. To exclude non-cardiological causes of the feeling of heart failure, the cardiologist can refer you to a general practitioner and endocrinologist.
If the cause of heart rhythm disturbances is the use of medications, you must contact your doctor to adjust the dose or replace the drug.
Diagnosis and examination of cardiac arrest
First of all, to detect cardiac arrhythmias, counting the pulse and heart rate is used. When examining a patient, the doctor uses auscultation to listen to the heart rhythm and detect other accompanying symptoms in order to diagnose the disease that has caused the change in heart rate.
If a pathological change in heart rhythm is detected, a therapist or cardiologist will prescribe an electrocardiographic study (ECG).
Pain in the temple area
Arthritis
9340 28 October
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Pain in the temple area: causes of occurrence, what diseases it occurs with, diagnosis and treatment methods.
Definition _
Pain in the temple area is one of the most common complaints that brings patients to the doctor.
In the bone structures of the skull and brain tissues, pain sensitivity is insignificant, so the main sources of pain are blood vessels, meninges and cranial nerves.
Types of pain in the temple area
According to the International Classification of Headaches 3 (2013), all headaches are divided into:
- for primary pain not associated with diseases of the brain and other structures of the head and neck;
- secondary pain associated with other diseases;
- painful cranial neuropathies, other facial and headaches.
Possible causes of pain in the temple area
Arterial hypertension
is one of the common causes of headaches in the back of the head and temples. When pressure increases, attacks of headaches occur, which may be accompanied by nausea, vomiting, and “spots” before the eyes.
Tension headache
– one of the common reasons for visiting a neurologist and therapist. Patients characterize it as squeezing, pressing.
Tension headaches interfere with quality of life and performance, despite the fact that they are considered benign and do not carry serious consequences.
Migraine
is the most common form of attack-like headache.
Migraine is characterized by localization of pain in the temporo-frontal-orbital region and a paroxysmal nature of the course.
If the pain is not paroxysmal, then it is not a migraine. Seizures can occur on one side of the head or on both sides, and can also change their location (right-left).
A headache attack can occur at any time of the day, more often during a night's sleep in the morning or after waking up. The pain is pulsating, bursting, with a gradual increase in intensity over several hours. Before the onset of an attack, a so-called aura is possible (harbingers of pain, they vary from person to person, but are often described as disturbances in vision, speech, or dizziness). The pain intensifies in bright light, from loud sounds and other irritants, including changes in head position. The attack can last up to several days.
Harris' periodic migraine neuralgia
- characterized by the sudden onset of pain in the eye area on one side and spreading to the temporal, frontal and zygomatic areas, and sometimes even to the neck.
Unlike migraines, there are no warning signs of pain.
The pain is burning, cutting, bursting, accompanied by redness of the eye and lacrimation on the painful side. Some patients experience a sensation of the eye “bulging out of its socket.” All these attacks are characterized by a certain seasonality or periodicity. The duration of the attack ranges from 6–8 weeks to 3 months.
Pain in the temple area may occur immediately after drinking cold water
or ice cream due to arterial spasm. In this case, the pain is aching, squeezing, sometimes throbbing.
Cold pain occurs in individuals with increased sensitivity to cold stimuli and high reactivity of the body.
“Sausage” headache
(in English-speaking authors -
hot dogs headache
) occurs when eating foods containing food additives such as sodium nitrate. During a chemical reaction in the body, nitrate is converted into nitrite, which has a vasomotor effect (controlling the process of contraction and relaxation of the muscular lining of the walls of blood vessels, and, consequently, the lumen of blood vessels), and sensitive people may feel pain in the frontotemporal region.
A similar effect sometimes occurs when eating Chinese dishes (“Chinese restaurant headache”), where monosodium glutamate is often used.
Giant cell arteritis
is the most common systemic vasculitis in the world, affecting large vessels. The favorite localization of this disease is the temporal artery. Most often, the pain is intense, accompanied by limited function of the corresponding temporomandibular joint, blurred vision with its gradual decrease, and a hardened artery in the temple area is detected.
Without treatment, it can lead to permanent blindness of the eye on the affected side.
With inflammatory diseases of the ear,
pain in the temporal and parotid region is possible, which is accompanied by fever, redness, swelling in the ear area, and purulent discharge from the ear.
Meningitis
develops when an infectious agent enters the membranes of the brain, followed by an inflammatory process.
The headache is sudden, sharp, diffuse, predominant in the frontotemporal areas, sometimes accompanied by vomiting.
Neuralgia of the auriculotemporal nerve
often occurs after an inflammatory process or traumatic lesion of the parotid gland. It is characterized by burning, throbbing pain in the area of the external auditory canal, temple, temporomandibular joint, radiating to the lower jaw. The pain is accompanied by increased salivation and redness of the skin over the affected area. Attacks are triggered by eating and smoking.
Neuralgia of the ear ganglion
manifests itself as attacks of burning pain in the temporal region lasting from several minutes to an hour. May be accompanied by ear congestion and increased salivation.
For altitude sickness
There is a change in arterial tone due to reduced oxygen pressure and changes in barometric pressure. Headache is accompanied by shortness of breath, palpitations, and blurred vision.
The severity of symptoms depends on the speed of ascent to altitude.
The pain is relieved by applying cold to the temples and drinking cool water.
Traumatic lesion of the temporal region
may be the cause of pain. This includes a wide group of pathologies: fracture of the temporal bone, dislocation of the temporomandibular joint, soft tissue contusion.
Subarachnoid hemorrhage
occurs for various reasons, for example, as a result of a rupture of a cerebral aneurysm, a person feels like a strong blow to the head, hot liquid pouring into the head, strong contraction, and then bursting. The pain may initially be localized in the corresponding part of the head - in the temporal region when an aneurysm of the internal carotid artery ruptures.
Damage to the temporomandibular joint
(both inflammatory - arthritis, and non-inflammatory - arthrosis, malocclusion) may be accompanied by pain in the parotid and temporal region. When moving the lower jaw, crunching and clicking may occur in the joint; the pain intensifies when chewing and during conversation.
Which doctors should I contact if I have pain in my temples?
If you experience intense and recurring pain in your temples, you should consult a specialist.
If pain persists after taking painkillers or other symptomatic treatment previously prescribed by your doctor (for example, to lower blood pressure), and there are no signs of injury, you should contact or. Depending on the accompanying symptoms, you may need to consult a neurologist, rheumatologist, otolaryngologist, or ophthalmologist. In case of previous injury, it is necessary to contact a traumatologist or to exclude severe injury.
Diagnostics and examinations for pain in the temples
The list of examinations is prescribed by the doctor depending on the indications. An approximate list of studies that may be prescribed:
- computed tomography of the head;
Arrhythmia
Pyelonephritis
Thyrotoxicosis
Rheumatism
9672 09 April
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Arrhythmia: causes of occurrence, in what diseases it occurs, diagnosis and treatment methods.
Definition
The heart is a muscular organ, a pump that maintains a constant flow of blood in the vessels, generating impulses at a certain frequency that lead to excitation and contraction of the myocardium. Normally, the contraction of the heart’s parts occurs sequentially: first, the right and left atria contract, then the right and left ventricles.
The main source of heart rhythm is located in the right atrium - the sinus node, which in a healthy adult sets the correct heart rate rhythm (60-80 beats per minute).
In addition to the sinus node, other parts of the myocardium can generate impulses and set the rhythm, but in a healthy person they do not cause arrhythmias due to the adequate functioning of the sinus node.
The heart has the property of conductivity, i.e. the ability to quickly propagate an impulse throughout the myocardial tissue, which is necessary for the coordinated work of all cardiac muscle cells.
Cardiac arrhythmia is a condition characterized by a disturbance in the rhythm of the heart, the process of impulse formation and its conduction. Some arrhythmias at a certain age are considered normal, but most are still a sign of one or another pathology, and therefore require close monitoring and treatment.
Types of cardiac arrhythmias
Depending on the heart rate (HR), arrhythmias are divided into
tachyarrhythmias
(with an increase in heart rate of more than 80–90 beats per minute) and
bradyarrhythmias
(with a decrease in heart rate of less than 60 beats per minute).
Based on the location of the myocardial area, which is an abnormal source of rhythm, supraventricular (supraventricular) arrhythmias
, when the pacemaker is located in the atria or in the atrioventricular node, and
ventricular arrhythmias
, when the pacemaker is located in the ventricles of the heart.
One of the most important classifications of cardiac arrhythmias is based on the immediate cause of its development.
- Arrhythmias due to impaired impulse formation, which are based on impaired functioning of the sinus node, for example, sinus arrhythmia, sick sinus syndrome, etc. According to statistics, the prevalence of sinus arrhythmia (SA) in the general population is 33.9-34.5%, sinus bradycardia (SB) - 7.1-12.8%, sinus tachycardia (ST) - 4.9-9.8%.
- Arrhythmias due to changes in the automaticity of latent pacemakers, for example, replacement cardiac rhythms.
- Arrhythmias caused by abnormal circulation of the impulse in the myocardial tissue, for example, extrasystole, atrial fibrillation (atrial fibrillation), atrial flutter.
- Disturbances in the conduction of impulses through the myocardium:
- blockades, for example, atrioventricular block, right bundle branch block, etc.;
- premature excitation of the ventricles - the passage of an impulse along additional pathways, for example, Wolff-Parkinson-White syndrome.
Separately, there is a respiratory arrhythmia, which is normally observed in young children and consists of an increase in heart rate during inhalation and a slowdown during exhalation.
Possible causes of arrhythmia
Some of the causes of heart rhythm disturbances lie directly in the structure of the heart, while others are caused by external influences on the heart.
To the reasons of the heart
arrhythmias include congenital and acquired heart defects, consequences of myocardial infarction, inflammatory changes in heart tissue (carditis), heart tumors, cardiomyopathy (changes in normal myocardial tissue), etc. Long-term diseases of the endocrine system, arterial hypertension, alcoholism, etc. can lead to changes in the structure of the myocardium.
To extra-cardiac reasons
conditionally include those conditions that cause rhythm disturbances without leading to structural changes in the heart tissue: changes in the innervation of the heart, changes in the balance of electrolytes (potassium, magnesium, calcium) with damage to the kidneys, adrenal glands, parathyroid glands, with prolonged diarrhea or vomiting, with intoxication, other changes in metabolic processes.
What diseases cause arrhythmias?
- Coronary heart disease (a disease based on insufficient blood supply to the heart muscle, resulting in oxygen starvation of the heart) and the consequences of a myocardial infarction.
- Long-term arterial hypertension.
- Hypertrophic, restrictive, dilated (including alcoholic) cardiomyopathy, arrhythmogenic dysplasia of the right ventricle are pathological conditions based on restructuring of the myocardium with disruption of its basic functions.
- Heart defects, for example, mitral stenosis, aortic insufficiency.
- Congenital heart defects, manifested by numerous symptoms, incl. arrhythmia, already from childhood.
- Congenital anomalies of the cardiac conduction system, for example, an accessory bundle in Wolff–Parkinson–White syndrome.
- Inflammatory damage to the myocardium (carditis, myocarditis).
- Acute and chronic kidney diseases, leading to changes in electrolyte balance, restructuring of myocardial tissue: chronic kidney disease due to glomerulonephritis, pyelonephritis, etc., acute kidney injury.
- Diseases of the endocrine glands: hypothyroidism, hyperthyroidism, adrenal dysfunction, etc.
- Tumors of the heart and other organs.
Which doctors should you contact if you have an arrhythmia?
As a rule, arrhythmias are first diagnosed either during a medical examination or when a patient approaches with specific complaints. Deviations in heart rhythm require consultation to clarify the type of arrhythmia and conduct a comprehensive study of the state of the cardiovascular system.
If the cause of the rhythm change is of extracardiac origin, the patient may be referred to other specialists - a nephrologist. If systemic rheumatic diseases are suspected, observation by a rheumatologist is required.
Diagnostics and examinations for arrhythmia
The doctor may suspect arrhythmias when the patient complains of interruptions in the heart, a feeling of “fading” of the heart, fainting, and shortness of breath. The diagnosis algorithm consists of a thorough history taking, assessing the state of the cardiovascular system (listening to the heart with a stethoscope, feeling the pulse, measuring blood pressure, etc.). According to the clinical examination, the doctor assumes damage to one or another system and prescribes additional laboratory and instrumental examinations:
- electrocardiography (ECG) in 12 leads;