What are heart defects?
There are two types of heart defects:
- Congenital (hereditary chromosomal mutations, bad habits during pregnancy or previous infections);
- Acquired (possible causes: inflammation of the inner lining and valve apparatus of the heart, destruction of the heart valves, atherosclerosis).
Heart defects include:
- Defects of intercardiac septa;
- Defects of the aortic orifice and pulmonary artery;
- Valve defects (stenosis, insufficiency).
Do they take into the army with prolapse?
Prolapse of the 2nd and 3rd degrees can be exempt from the army. Such forms of the disease are often accompanied by disturbances in the functioning of the heart, so patients require lifestyle adjustments. You have to give up overwork, don’t be nervous, and refrain from heavy physical activity. The military lifestyle during these stages can be detrimental to the hearts of sick conscripts.
The conditions for exemption from the army for prolapse are specified in Article 42 of the Schedule of Diseases. The military registration and enlistment office determines the suitability category based on whether the conscript has:
- Severe heart rhythm disturbances;
- Conduction disorders;
- Heart failure.
When assessing heart failure, doctors take into account its functional class (FC).
There are 4 classes:
- FC I – heart disease does not require changes in physical activity. Normal exercise does not cause symptoms of heart failure (shortness of breath, rapid heartbeat, weakness).
- FC II - symptoms appear during normal physical activity, but disappear at rest.
- FC III – shortness of breath, irregular heartbeat rhythms with little physical activity.
- FC IV - symptoms appear even at rest.
According to the Schedule of Diseases, those with mitral valve prolapse are recruited into the army if the disease is accompanied by heart failure FC I. They can also be drafted in cases where the disease is asymptomatic, does not cause discomfort and does not require hospital treatment. In each of these cases, the military registration and enlistment office assigns the conscript a “B-4” fitness category.
The situation is different if the patient has increased mitral regurgitation. Conscription into the army with prolapse in such cases can lead to new complications: mitral regurgitation, arrhythmia or infective endocarditis. Therefore, with increased regurgitation, the conscript also has a chance of being exempt from military service. Exemption from conscription is also granted to young people whose illness is accompanied by disturbances in heart rhythm, conduction, or heart failure FC II.
Stage 3 of the disease is the most pronounced. An increase in the deflection of the valve walls leads to a significant outflow of blood. Against the background of increasing regurgitation, significant disruptions in the functioning of the circulatory system develop. As a result, cerebral circulation and heart rhythm are disrupted, and heart failure appears. If there are serious complications, the army and prolapse are not compatible.
When examining the question of whether people with prolapse are accepted into the army, I relied on legislation. However, as practice shows, draft commissions do not always make a lawful decision and issue the fitness category that must be assigned by law. Therefore, remember: if you do not agree with this decision, you have the right to appeal it to a higher draft commission or court.
Heart disease and the army
What are the general eligibility categories?
- G - fit for service;
- GO - fit for service with minor restrictions;
- VN - temporarily unusable;
- GPS - unfit for service in peacetime;
- NGI - unfit for service with exclusion from military registration;
Congenital heart defects are classified under article 80 of the disease schedule, and acquired defects are classified under article 42.
It follows from it:
- A conscript with a combined (damage to several heart valves at once) or combined (damage to one heart valve: stenosis and insufficiency) acquired heart disease receives the NGI .
- Isolated stenosis of the left atrioventricular orifice in the presence of stage 2 chronic heart failure belongs to the NGI .
- Also, in case of prolapse of the mitral valve or other valves of the 3rd degree (9 mm or more), 2nd degree (from 6 to 8.9 mm) with a violation of intracardiac hemodynamics, the NGI fitness category is assigned.
- Isolated heart defects without chronic heart failure are classified as suitable for CGM.
- Mitral valve prolapse (MVP) or other heart valves of the 1st degree (from 3 to 5.9 mm) with regurgitation of the 2nd degree or more, MVP of the 2nd degree (from 6 to 8.9 mm) without disruption of intracardiac hemodynamics are classified as suitable for CGM.
To determine the exact diagnosis and fitness category, the conscript should consult a specialist, as well as to avoid serious complications.
What is mitral valve prolapse
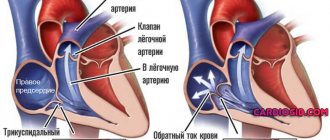
The human heart consists of four chambers: two atria (left and right) and two ventricles (also left and right). The left half of the heart is separated from the right by a muscular septum. And between the chambers in each half there is a valve that connects or separates them. The valve between the left atrium and the ventricle is called the mitral or bicuspid valve.
When it is open, through it, when the left atrium contracts, oxygenated blood from the pulmonary vein enters the left ventricle. After this, the mitral valve closes, preventing blood from flowing back into the atrium, and it is pushed into another exit from the ventricle - the aortic valve, from which it flows into the aorta. The aorta branches into arteries that go to all organs and parts of the body.
Normally, the mitral valve, in the closed position, completely blocks the lumen between the atrium and the ventricle, so that the blood completely flows into the aorta. However, it happens that the doors sag when closed and fall into one of the chambers, not ensuring complete closure of the lumen. Then the blood partially flows not only into the aorta, but also back into the atrium. The extent of this “partially” depends on the degree of sagging of the sashes. Simply put, organs do not receive enough oxygen carried to them by blood.
This pathology is called mitral valve prolapse (MVP), from the Latin prolapsus “prolapse”. And the reverse flow of blood from the ventricle to the atrium is regurgitation, from the Latin gurgitare “to flood,” that is, “reverse flooding.” The sagging itself, the retraction of the valves, is terminologically called prolapse. MVP is the main type of mitral valve insufficiency.
MVP can be congenital or acquired due to calcium deposits on the valve, pathologies of the heart muscle, heart attack, ischemia and other diseases. Symptoms such as stabbing pain in the heart, dizziness, shortness of breath, irregular heart rhythm, and high blood pressure are typical. In serious cases, fainting occurs when the brain lacks oxygen due to regurgitation of blood into the atrium.
Side-by-side comparison. On the left is a healthy mitral valve in a closed state. On the right is a picture of prolapse with regurgitation: obvious non-closure of the valves and reverse flow of arterial blood. At the top left is the aortic valve.
How can we help?
Often conscripts do not know their illnesses, where to go and where to be examined in order to confirm diagnoses and have the right to a deferment or exemption from the army. We employ specialists with extensive positive experience and this is confirmed by reviews from our clients. We guarantee qualified assistance, advice and support from specialists until you receive a military ID or a refund of 50% of the cost of services in the event of a different decision by the draft commission.
You study, work, you have many plans for life. Are you worried about your career or further studies? Are you a law-abiding citizen, but do you think that military service could worsen your health? Contact us and, if you have the right not to serve, we will help you prove it!
Degrees of prolapse severity
The more the valves recess, the greater the regurgitation and the more serious and severe the health consequences. Depending on the amount of sagging, there are three degrees of mitral valve prolapse:
- The first is prolapse from 3 to 6 mm. Usually there are no pronounced consequences in the first degree; with significant loads, short-term mild tingling pain in the heart, rapid heartbeat, and hypertension (a short-term increase in blood pressure without hypertension) are possible. After the end of the load, the condition returns to normal without any intervention. If first-degree MVP does not cause pain or heart rhythm disturbances at all, treatment is not required.
- The second is prolapse from 6 to 9 mm. Here, all the symptoms are much more likely, including shortness of breath, irregular heartbeat, etc. Pain in the heart occurs more often; for this, less stress is sufficient than for first-degree MVP; the pain can be triggered by ordinary household activities that require physical effort. At the same time, the pain lasts longer, is felt more strongly, and medications are often required to get rid of it. Second-degree MVP can form chronic heart failure. It requires conservative treatment.
- Third – prolapse of more than 9 mm. This means full-blown chronic heart failure. Painful sensations occur regularly, after relatively little physical activity, they last longer, are stronger, and are relieved mainly with medication. Therefore, physical activity in third-degree MVP is severely limited and, in some cases, contraindicated. In particularly difficult cases, surgical intervention is possible, including installation of an artificial mitral valve.
Please note: prolapse of less than 3 mm is not even considered a pathology, this is the limit of the norm, such sagging is possible occasionally without diagnosing MVP. In addition, four degrees of regurgitation are separately distinguished according to the length of the reverse blood flow (measured in mm, counting from the base of the mitral valve leaflets; with MVP of the first degree, reverse blood flow may not be observed at all):
- the first is insignificant, with a jet length of up to 3 mm;
- the second is moderate, the jet length is from 3 to 6 mm;
- third – medium with a jet length from 6 to 9 mm;
- the fourth is pronounced if the length of the jet exceeds 9 mm.
In the diagnosis, the cardiologist indicates both components, for example, “1st degree mitral valve prolapse with 1st degree regurgitation.” As a rule, the first degree of MVP is accompanied by regurgitation of the first degree, rarely - the second. The principle is simple: the greater the sagging, the more blood returns to the atrium. Therefore, the third and fourth degrees of regurgitation are characteristic of the second, and more often the third degree of MVP.
Aortic regurgitation on cardiac ultrasound
Discussion - Ultrasound of the heart
Greetings. About 8 years ago, the following diagnosis was discovered: bicuspid aortic valve with 0-1 degree insufficiency, an additional chord in the left ventricle and tricuspid regurgitation of 1-2 degrees. I would like to know more about the complex of these diagnoses, what they are fraught with and what kind of life one should lead: what to avoid and what to strive for. What will happen to me in the future? What are the risks? At the moment there are no special complaints, I have never fainted, rarely, about 1-2 times a month it gets dark in my eyes when I suddenly stand up, but my blood pressure (I measure it at work every day) is always, according to the nurse, rather low (on average 120 /40 sometimes happens at 30). In adolescence, very often, especially in the evening, there was a feeling of incomplete inspiration, i.e. I could not breathe deeply through my mouth, also 5 years ago my lower legs became swollen (the place where the leg articulates with the foot) and the swelling lasted for about 2 weeks (possibly and a lot more time passed, I don’t remember anymore) at the same time it was painful to walk, and after the swelling subsided, its place itched. The same situation repeated itself about 3-4 years ago, after which no swelling occurred. Also, if I lie on my left side before going to bed, I experience discomfort with a slight heaviness and can clearly hear my heartbeat. I also hear the beating of the heart not only before going to bed when lying down (it sounds like it’s beating under the ribs and ends somewhere under the Adam’s apple). And one more question: it so happens that I have to work at work with heavy physical labor. This includes lifting and lowering heavy objects, as well as high physical activity throughout the entire 8-hour working day. At the moment, this does not affect me in any way (except for the fact that my heart beats quickly after lifting, carrying and lowering weights, but the knocking quickly subsides), so, I understand that at this age I will be able to withstand all loads perfectly well, but I’m interested what will happen to me in the future, because such work, as far as I understand, will have a bad effect on my heart in the future in 5-10 years. So, how will it affect and what is the worst that can happen? I have many good friends who play sports and lead a healthy lifestyle, I want to join them, but I’m afraid to start anything without consulting a doctor. This leads to another question: can I work out in the gym? Lifting weights and such? Of course, I don’t mean lifting extreme weights and “punctured” with drugs to increase muscle mass, I’m just talking about healthy eating and working out in the gym 2-3 times a week for 1 hour in order to get an athletic figure. So, what do you think, is it possible for me to do this and how dangerous is it if I can’t do it? By the way, I was not accepted into the army precisely because of the diagnosis I described. Thank you for your time, I look forward to your answers and recommendations.