Anomalies in the location of the heart are one of the most difficult areas in the problem of congenital heart defects. They may be a consequence of abnormal development of the heart itself and the result of the influence of extracardiac causes [1]. The abnormal location of the heart in the chest was first described by the Italian anatomist and surgeon Jerome Fabricius in 1606. Marco Aurelio Severino used the term “dextrocardia” in 1643 when describing the mirror arrangement of internal organs in a patient. Matthew Bailey later described organ transposition as a complete rotation of the thoracic and abdominal organs in a mirror image [2–4].
Patient L
., 61 years old, was admitted to the clinic with a diagnosis of coronary artery disease. Angina pectoris of the 3rd functional class according to NYHA, multivessel disease of the coronary arteries, arterial hypertension grade 3, grade III, risk 4, insulin-dependent diabetes mellitus.
Upon admission, he complained of pressing pain in the chest with little physical activity.
From the anamnesis it is known that about 9 years ago the patient noted the appearance of pressing pain behind the sternum during physical activity. He was treated by a cardiologist at his place of residence. Over the past year - progression of angina pectoris, decreased tolerance to physical activity. In March 2021, coronary angiography (CAG) was performed and multivessel lesions of the coronary arteries were detected. Long-term history of arterial hypertension with maximum blood pressure values up to 180/80 mmHg, regularly takes antihypertensive therapy.
Dextrocardia ( situs inversus
).
Survey data. ECG: sinus rhythm, heart rate 73 per minute, deviation of the electrical axis of the heart to the left. Violation of intraatrial and intraventricular conduction along the right branch of the His bundle.
Echocardiography: ascending aorta 4.3 cm, left atrium (LA) 5.2 cm, right ventricle (RV) 3.4 cm, left ventricular end-diastolic dimension (LVEDD) 5.3 cm, LV end-systolic dimension (ESD) 3.9 cm, stroke volume (SV) 68 ml, LV ejection fraction (EF) 49%, interventricular septal thickness (IVS) 1.2 cm, LV posterior wall thickness (LVPT) 1.2 cm, right atrium (RA) not enlarged. There is no significant regurgitation on the heart valves, systolic pressure in the pulmonary artery is 22 mm Hg.
CAG: stenosis of the trunk of the left coronary artery up to 80%, stenosis of the proximal third of the anterior descending artery (LAD) up to 70%, stenosis of the middle third of the circumflex artery up to 90%, occlusion of the obtuse edge branch (BMA), the right coronary artery (RCA) is not stenotic, stenosis of the middle third of the posterior descending artery (PDA) up to 80%. SYNTAX Score II - 29.6.
On April 23, 2018, mammary coronary bypass grafting (right internal thoracic artery) of the LAD, autovenous coronary artery bypass grafting of the VTK and MLV of the RCA on a beating heart were performed. The operation time was 106 minutes.
Intraoperatively, taking into account the transposition of the heart and the fact that the “gold standard” in coronary artery bypass surgery is the use of the ITA for LAD bypass, the tactics of contralateral positioning of the surgical team and the use of the right ITA (RUHA) for LAD bypass were chosen (Fig. 1).
Rice. 1. Anastomosis of the PVGA with the LAD. The choice of the PIHA in this case is due to the possibility of forming an anastomosis with the LAD without tensioning the graft and crossing the conventional midline, which, in the case of repeated surgery, can more likely ensure the safety of the shunt.
Considering that the patient had insulin-dependent diabetes mellitus, severe obesity (body mass index 31 kg/m2) and a high risk of developing wound and sternal infections, it was decided to abandon the use of the left IMA. When forming autovenous anastomoses, no technical difficulties associated with the unusual location of the heart were noted.
It should also be noted that when forming a proximal anastomosis, its heel should be mirrored in relation to its position during coronary bypass surgery in patients with normal arrangement of internal organs.
When performing intraoperative flowmetry, the following indicators of blood flow through the shunts were determined: PIHA with LAD - volumetric blood flow (Q) 31 ml/min, PI 2.3; autovenous shunt with VTK - Q 43 ml/min, PI 2.4; autovenous shunt with VNA of the RCA - Q 45 ml/min, PI 2.8.
Anesthetic care for operations in patients with dextrocardia includes preoperative examination, contralateral placement of ECG electrodes, placement of a central venous catheter in the left jugular vein due to its direct course to the anatomically left atrium (true right atrium).
The early postoperative period was uneventful. The patient was extubated 3 hours after surgery; there was no need for sympathomimetic support. Transferred to the specialized department 21 hours after the operation. In the postoperative period, paroxysmal atrial fibrillation was noted. Appropriate antiarrhythmic therapy was administered.
Postoperative echocardiography data: LA 4.2 cm, RV 3.0 cm, LV EDV 4.3 cm, LV ESD 3.3 cm, LV end-diastolic volume 81 ml, LV end-systolic volume 45 ml, SV 36 ml, LVEF 45%, IVS thickness 1.3 cm, LVSD thickness 1.1 cm, RA not increased. There is no significant regurgitation on the heart valves, systolic pressure in the pulmonary artery is 22 mm Hg.
The patient was discharged on the 10th day after surgery in satisfactory condition.
Right-formed mid-positioned heart.
Previous | Contents | next Synonyms: mesocardia, mesoversion, incomplete dextroversion. This defect accounts for 9% of all AVRS [Bukharin V. A . and Podzol - kov _ V. P., 1979] and is usually a random find if it is not combined with other congenital disorders (Fig. 89, b).
In contrast to the right-formed, right-positioned heart, rotation to the right under these conditions is not so significant and the longitudinal axis of the heart, together with the interventricular septum, is located along the midsagittal axis of the chest, as a result of which the heart occupies a midline position. The vena cava and the right atrium are located on the right, and the right atrium lies in the same plane as the left atrium or somewhat anteriorly, i.e. e. their relationship is approaching normal. The right and left ventricles lie to the right and left of the midline of the body, so that there is no conventional division into anterior and posterior. The apex of the heart is located in the epigastric region, oriented forward and can be bifurcated. In such a two-apex heart, the right apex is formed by the right ventricle, the left - by the left ventricle. The great vessels arise from the corresponding ventricles, the aortic arch is on the left. The location of the abdominal organs is normal.
Among concomitant congenital heart disease, the most common are tetralogy of Fallot, VSD, patent atrioventricular canal (AVC), corrected by TMS.
A shift of cardiac dullness to the right is usually regarded as an enlargement of the right chambers of the heart, and the apical impulse,
palpated in the epigastric region, can be mistaken for the pulsation of a hypertrophied right ventricle. More often, heart murmurs are heard equally well on the right and left of the sternum, less often - only on the left or right. On percussion, hepatic dullness and gastric tympanitis are detected in the usual places.
The ECG shows a positive P
in leads I and aVP, negative - in lead aVR.
In lead aVL, the P
may have a different direction.
In standard I and in lead aVL, a deep Q
and a negative
T
occur with the same frequency or slightly less frequently than in a right-sided heart.
In the chest leads, right ventricular potentials in the form of rS
and
RS
are recorded to the right of the body midline, and left ventricular potentials in the form of
qR
or
qRS
are recorded to the left.
An X-ray examination in a direct projection reveals the shadow of the heart, occupying a mid-position and having a spherical shape in the form of a raindrop. Rotating the patient to the right anterior oblique view at 15 degrees usually reveals a normal cardiac configuration. In direct projection, the apex of the heart is not identified. The liver shadow is localized under the right dome of the diaphragm, and both the right and left domes of the diaphragm are located at the same level.
Cardiac catheterization and angiocardiographic examination clarify the right-sided location of the vena cava and right atrium. When a contrast agent enters the left atrium and left ventricle, their left-sided position is determined. The shadow of the contrasted left ventricle is located to the left of the midline of the body and partially covers the left atrium. The interventricular septum is located along the midline of the body. In the lateral projection, the shadows of the ventricles overlap each other and, as a result, it is impossible to speak about their anterior or posterior position. The great vessels are contrasted from the corresponding ventricles.
Surgical intervention is determined by the topic of the congenital heart disease, and is usually performed using the same approaches as in the normal position of the heart.
Legally formed
left-sided
heart with inverted
abdominal organs
or abdominal heterotaxyebism.
Synonyms: levocardia, levocardia with transposition of the abdominal organs, isolated inversion of the abdominal organs, levocardia, situs solitus.
Violations of the correspondence between the location of the apex of the heart, on the one hand, and the right atrium and liver, on the other hand, were the basis for classifying a right-shaped, left-oriented heart with a reverse arrangement of abdominal organs or abdominal heterotaxy as anomalies of the location of the heart [Konstantinov B. A., 1967; Podzolkov V. P . et al., 19741.
The location of the heart and the relationship of its chambers and great vessels relative to each other is normal. The presence of anomalies of the inferior vena cava is characteristic: in some cases it is located to the left of the spine, then at the level of the liver it abruptly changes its course and, crossing the midline of the body, is directed obliquely upward to connect with the usually located right atrium; in other cases, there is an absence of the hepatic segment of the inferior vena cava, and the outflow of venous blood from the lower half of the body is carried out through the azygos or semi-gyzygos vein, which flows into the superior vena cava. It is extremely rare that the inferior vena cava is located on the right.
The position of the abdominal organs is characterized by mirror topography, i.e. e. the liver is located on the left, and the ventricle and spleen are on the right. Often one can note signs of abdominal heterotaxy, expressed in an enlargement of the right lobe of the liver, incomplete rotation of the intestine (common mesentery) and polysplenia.
The absence of congenital heart disease is observed in approximately one third of patients. The remaining 2/3 patients usually have severe and multiple defects such as the pentade of Fallot, TMS, a single ventricle of the heart - Data from an objective examination and the results of x-ray examination allow us to establish only a left-oriented heart with a reverse arrangement of abdominal organs or abdominal heterotaxy without specific indications about the nature of its formation . The radiograph reveals a normally located heart, the shadow of the liver is determined under the left dome of the diaphragm, and the gas bubble is under the right, the configuration of the heart is determined by concomitant congenital heart disease. Information about the localization of the right atrium is obtained by analyzing an ECG that registers a positive P wave in the first standard lead, cardiac catheterization, which reveals an anomaly of the systemic veins draining into the right atrium, and using an angiocardiographic study, which establishes the normal anatomical structure and topography of the heart chambers. The diagnosis of concomitant congenital heart disease is made based on generally accepted diagnostic criteria.
Surgical tactics and technique depend on the anatomical - hemodynamic - variant of the concomitant congenital heart disease, and when planning surgical intervention under artificial circulation, anomalies of the inferior vena cava must be taken into account.
Left-formed right-oriented heart. Synonyms: mirror dextrocardia, true dextrocardia. The frequency of the defect is 33 %
from all patients with a right-sided position of the heart (Bukharin V.A., Podzolkov V.P., 1979]. In contrast
from the right-formed right-oriented heart with this anomaly, the left-sided vena cavae connect to the right atrium, which is also located to the left and somewhat anterior to the right-sided left atrium (Fig. 89, c). The right atrium is separated by the tricuspid valve from the right ventricle. Its outflow section is directed to the right, upward, posteriorly, and from it begins the pulmonary trunk, located to the right of the midline of the body. The pulmonary veins connect to the right-sided left atrium, which communicates with the left ventricle through the mitral valve. The latter is located to the right and posterior to the right ventricle and forms the right-sided apex of the heart. The aorta departs from the left ventricle, the ascending section of which lies to the left and posterior to the pulmonary trunk.
Thus, the left-formed right-sided heart is an exact mirror copy of the normal heart. With rare exceptions, a left-formed, right-oriented heart is part of a complete reverse arrangement of internal organs. The left lung consists of 3 lobes, the right - of 2, and the tracheobronchial tree is also characterized by mirror anatomy. The left half contains the liver and gall bladder, and the left lobe of the liver is much larger than the right; the ascending colon, the cecum, and the vermiform appendix also lie here. In the right half of the abdominal cavity, the spleen, stomach and descending colon can be noted. The literature describes isolated cases of anomaly with normal arrangement of abdominal organs.
According to the observations of many authors, triad M occurs in 16.5 - 25% of patients. Kartagener (1933), which includes a complete reverse arrangement of internal organs with a left-formed right-oriented heart, bronchiectasis and paranasal sinusitis.
CHDs with a left-shaped right-positioned heart, compared to other anomalies of the heart's location, are observed much less frequently, but more often than with a normal heart position. Their frequency ranges from 4 to 8% [Konstantinov B. A., Astrakhantseva G. I., 1965; Keith J. et al., 1958]. UPS at 94 %
are multiple in nature and in 70
%
are accompanied by cyanosis; the most common are tetralogy of Fallot, single ventricle of the heart, corrected TMS, open VVC, aortic stenosis, etc.
The condition of patients with this anomaly without concomitant heart defects is usually favorable, there are no complaints, they are physically developed normally and live to a ripe old age. The boundaries of cardiac dullness and the apex of the heart are determined to the right of the sternum, here heart sounds are better heard and, in case of congenital heart disease, cardiac murmurs are heard. Hepatic dullness is determined on the left, gastric tympanitis on the right. The ECG shows a negative wave Pv I, aVL, Vs. e lead, reflecting the location of the sinus node in the left atrium, positive Pn. in. v,, negative complexes QRSuvtt,
an increase in their voltage from Vi to Ven and a decrease from Vi to V 6, negative Ti, and vL.
vM. Conventional ECG recording records waves in standard lead I that have the opposite direction to normal; II standard lead corresponds to normal III and, conversely, III standard lead corresponds to the second, lead aVL reflects lead aVR and, conversely, aVR - aVL, lead V is equivalent to V 2 R, Uz - / zk,
V 4 - Vir, Ve - V 5 R ,
-
VeR . Lead aVF does not change.
If you swap the electrodes of the right and left arms and apply the chest electrodes in such a way that their position is a mirror image of the normal one, then the ECG can be analyzed as if the heart is in a normal position.
During an x-ray examination in the anteroposterior projection, the shadow of the heart and its apex are determined in the right half of the chest (Fig. 90), due to this, the right pulmonary field is narrower than the left, and the right dome of the diaphragm is lower than the left. The heart silhouette is a mirror copy of a normally positioned heart. The shadow of the liver is visible under the left dome of the diaphragm, the gas bubble - under the right.
With the help of cardiac catheterization and angiocardiographic examination, the left-sided position of the vena cava, the topography of the cardiac cavities and great vessels, which are a mirror copy of the normal heart, are clarified, and concomitant heart defects are identified.
Only concomitant heart defects are subject to surgical treatment.
Left-formed left-sided heart. Synonyms: levocardia with transposition of the abdominal organs, isolated levocardia, left version of the heart, sinistroversion of the heart, blue-strocardia, cyanotic levocardia, mixed levocardia with atrial inversion (Fig. 89, d). With this anomaly, the heart is located on the left, where the liver and right atrium are also located. This is one of the rare variants of abnormal position of the heart. According to statistics J. Keith et al. (1958), the anomaly occurs approximately 10 times less frequently than a left-formed right-oriented heart, and amounts to 0.8 - 1.0% among all congenital heart disease and 10% among AVRS.
>
the lateral left atrium, which is slightly anterior to the left-sided right atrium. Through the mitral valve, the left atrium communicates with the left ventricle, which lies in front and to the left in relation to the left atrium, to the right and in front of the right ventricle. The ascending aorta is located to the left and posterior to the pulmonary trunk. The arch and descending aorta are also localized on the right. The apex of the heart is directed to the left, forward and down.
Left-formed left-positioned heart is accompanied by
is due to the reverse arrangement of internal organs, i.e. e. two-lobe - left structure of the right lung and three-lobe of the left, the liver is located under the left dome of the diaphragm, the stomach - under the right, etc. d. However, under these conditions, signs of visceral symmetry are observed more often than with previously described types of heart position.
The literature describes only one autopsy-confirmed case of a left-formed left-sided heart without congenital heart disease. In the vast majority of cases, this anomaly is combined with severe cyanotic congenital heart disease, among which the most common is a single ventricle of the heart with inversion TMS, pulmonary artery stenosis, corrected TMS with an open common VVC and pulmonary artery stenosis, and a two-chamber heart.
An objective examination reveals the left-sided position of the apex beat and cardiac dullness, while hepatic dullness is on the left, and gastric tympanitis is on the right. With concomitant heart defects, the clinical picture is determined by the anatomical and hemodynamic variant of the defect. The severity of concomitant congenital heart disease leads to the fact that 75 %
patients do not survive to 1 year and only 6
%
live after 5 years of age. .
The electrocardiographic sign of the defect is negative P
in leads I and aVL, indicating the left-sided position of the right atrium.
In the chest leads, the voltage of the QRS
from Ve to V, and then decreases to V ^ r.
An x-ray of the chest organs shows the normal position of the heart shadow, the liver shadow is determined under the left dome of the diaphragm, and the gas bubble of the stomach is under the right. The left dome of the diaphragm is lower than the right one. However, it is not possible to determine the type of heart formation using x-ray examination.
During catheterization and angiocardiography, the left-sided position of the vena cava and the right atrium is established. The right atrium is covered over a considerable extent by the shadow of the contrasted venous, anatomically left ventricle, which forms the apex of the heart. When receiving the levogram phase, the left atrium is revealed, forming the right lateral contour of the heart and then the arterial, anatomically right ventricle, located to the right and lower in relation to the venous ventricle. From the arterial ventricle, the ascending aorta is contrasted, occupying a position to the right of the pulmonary artery. An angiocardiographic study, as a rule, reveals pulmonary artery stenosis and other congenital heart defects, often multiple; their identification often requires repeated injections of a contrast agent into various parts of the heart. The frequent existence of severe complex congenital heart disease limits the possibilities of surgical care for such patients.
Uncertain - a formed heart is a complex lesion of the cardiovascular system, in which even a detailed anatomical study of the atrial cavity, the location of the vena cava and pulmonary veins does not allow us to speak about the nature of the formation of the heart; usually there are severe congenital heart diseases.
Synonyms: uncertain cardiac situs, atrial isomerism, visceral heterotaxy syndrome, visceral symmetry syndrome. The incidence of the anomaly is 11% among patients with AVRS.
The anomaly usually occurs in the form of 2 pathological syndromes [Podzolkov V. P . et al., 1974], common to them are a single atrium, defects of the atrioventricular valves (split leaflets, a single ring), anomalies in the formation and location of the vena cava, abnormal drainage of the pulmonary veins. The heart and its apex are often located on the right. The liver can be located in the middle, less often on the right or left. The first of them is characterized by: 1) common atrium; 2) accessory superior vena cava, flowing into the left half of the common atrium; absence of the hepatic segment of the inferior vena cava; 3) partial or complete anomalous drainage of the pulmonary veins, symmetrically flowing into the right and left sides of the common atrium; 4) splitting of the septal leaflets of the atrioventricular valves; 5) often right-oriented heart; 6) often 2 lobes in each lung; 7) abdominal heterotaxy: tendency towards a midline location of the liver, common mesentery; polysplenia.
P . et al., 1974], common to them are a single atrium, defects of the atrioventricular valves (split leaflets, a single ring), anomalies in the formation and location of the vena cava, abnormal drainage of the pulmonary veins. The heart and its apex are often located on the right. The liver can be located in the middle, less often on the right or left. The first of them is characterized by: 1) common atrium; 2) accessory superior vena cava, flowing into the left half of the common atrium; absence of the hepatic segment of the inferior vena cava; 3) partial or complete anomalous drainage of the pulmonary veins, symmetrically flowing into the right and left sides of the common atrium; 4) splitting of the septal leaflets of the atrioventricular valves; 5) often right-oriented heart; 6) often 2 lobes in each lung; 7) abdominal heterotaxy: tendency towards a midline location of the liver, common mesentery; polysplenia.
The second pathological syndrome is characterized by an open common atrioventricular canal or a two-chamber heart with the following structure: I) common atrium; 2) open common atrioventricular canal or common atrioventricular valve; 3) VSD or single ventricle of the heart; 4) accessory superior vena cava, flowing into the left side of the common atrium; two inferior vena cava or absence of the hepatic segment of the inferior vena cava; 5) complete anomalous drainage of the pulmonary veins into the superior vena cava, into the common atrium, or into the portal venous system; 6) often transposition of the great vessels; 7) stenosis or atresia of the pulmonary artery; often right-sided heart; 9) often 3 lobes in each lung; 10) abdominal heterotaxy; median symmetrical liver, common mesentery; 11) asplenia.
2) open common atrioventricular canal or common atrioventricular valve; 3) VSD or single ventricle of the heart; 4) accessory superior vena cava, flowing into the left side of the common atrium; two inferior vena cava or absence of the hepatic segment of the inferior vena cava; 5) complete anomalous drainage of the pulmonary veins into the superior vena cava, into the common atrium, or into the portal venous system; 6) often transposition of the great vessels; 7) stenosis or atresia of the pulmonary artery; often right-sided heart; 9) often 3 lobes in each lung; 10) abdominal heterotaxy; median symmetrical liver, common mesentery; 11) asplenia.
Regardless of the location of the confluence of the systemic pulmonary veins, the flows of venous and arterial blood are directed into the cavity of the common atrium, where they are mixed, therefore, patients from birth experience arterial hypoxemia, which is more pronounced with concomitant pulmonary artery stenosis. The existence of anomalies of the atrioventricular valves is accompanied by severe insufficiency, which significantly worsens hemodynamic conditions and early leads to dilatation of the atria and ventricles.
Both syndromes are characterized by a severe clinical course and early mortality: 85.5 - 95 %
these patients die within the first year of life. The leading cause of death is pneumonia or heart failure.
All patients have severe cyanosis, shortness of breath and other signs of cyanotic heart disease from birth. The apical impulse and cardiac dullness can be detected in the right or left half of the chest. A systolic murmur is usually heard along the left or right sternal border. In patients without interventricular defect (first pathological syndrome), it is quiet and depends on relative, secondary stenosis of the pulmonary artery and insufficiency of the atrioventricular valves. In the presence of pulmonary artery stenosis, observed in the second pathological syndrome, the systolic murmur has a rough timbre and is better heard at the base of the heart.
There is a Pi wave on the ECG. ovl - negative or isoelectric, arrhythmias in the form of left atrial rhythm or coronary sinus rhythm are not uncommon. Deviation of the electrical axis of the heart to the left or its location in the silent sector along with S or */? S type ECG and signs of combined hypertrophy of the atria and ventricles suggest an open common AVK, a two- or three-chambered heart.
An x-ray examination of the abdominal cavity reveals a symmetrical, midline location of the liver shadow, which is a specific x-ray symptom of this anomaly. A contrast study of the gastrointestinal tract confirms the location of the stomach and establishes incomplete rotation of the intestine, including the common mesentery. On the cholecystogram, the gallbladder is displaced to the midline of the body.
On chest x-rays in the anteroposterior projection, the shadow of the heart is moderately enlarged in diameter and is often located in the right half of the chest. With a left-located heart, its left contour is represented by the ventricular surface, and the right – by the atrial surface, and, conversely, with a right-located heart, its right contour is formed by the ventricular surface, the left – by the atrial surface. The pulmonary artery arch is usually not defined (second pathological syndrome).
An important diagnostic feature is represented by superexposed chest radiographs, which show the symmetrical topography of the tracheobronchial tree, indicating with great accuracy an indeterminately formed heart.
Cardiac catheterization and angiocardiographic examination confirm anomalies in the confluence of the vena cava, from which the contrast agent enters the rounded atrial cavity, which occupies the presumed area of both atria, which indicates the presence of a common atrium.
Radical surgical treatment is possible in patients with the first, and less often with the second, pathological syndrome, in whom intervascular anastomoses and, in some cases, hemodynamic correction using the Fontan method can be performed.
Discussion
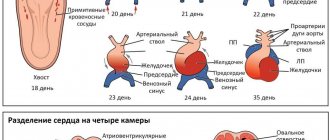
Currently, dextrocardia is understood as a rare congenital anomaly of the development of the cardiovascular system, in which the heart is located in the chest on the right. Accordingly, all incoming and outgoing vessels of the heart are located in a mirror image with respect to their normal position. During embryogenesis with situs inversus
the developing thoracoabdominal organs rotate 270° clockwise, and during the normal formation of internal organs, a rotation occurs 270° counterclockwise [11].
Using genetic studies, it has been established that dextrocardia is associated with a mutation in the HAND
,
ZIC3Shh
,
ACVR2
,
Pitxz
. The autosomal recessive mode of inheritance of this pathology has been proven. The frequency of this anomaly reaches 1.5-5% among all congenital heart defects. Dextrocardia is usually combined with transposition of the great vessels [3-5]. The most common forms of pathology are a right-formed right-sided heart (isolated dextrocardia, 54%) and a left-formed right-sided heart (mirror dextrocardia, 33%). In the first case, the location of other chest organs and the topography of the abdominal organs correspond to the physiological norm, and in the second case, a complete reverse arrangement of the internal organs is noted [6-8].
The first coronary bypass surgery in a patient with dextrocardia was described in 1980 [9].
There are limited reports in the literature [10] on myocardial revascularization in such patients. Most surgeons, when operating on patients with dextrocardia, prefer to stand on the patient's left side due to the position of the heart. However, there are reports [12] in which surgeons successfully performed such operations while working in a normal position.
MARS - syndrome. Diagnosis as the name of a planet.
In Belarus, in recent years there has been an increase in the number of children with MARS. This is primarily due to the widespread introduction of cardiac ultrasound into the practice of pediatric cardiologists.
Many parents begin to worry when they hear that their child has been diagnosed with MARS. In the popular literature there is practically no information about this syndrome in an accessible form. Now let's try to understand this syndrome by answering the most common questions that parents ask their cardiologist at their appointment.
What is MARS?
Minor anomalies of cardiac development (or MARS) are one of the manifestations of not entirely correct development of connective tissue. Connective tissue is found in all organs. It forms the frame of the heart, valves and walls of large vessels. Due to this, the heart tissue is elastic, but quite durable. Minor anomalies in the development of the heart are considered to be the presence of anatomical congenital changes in the heart and its large vessels. In this condition, the connective tissue is either too weak or is formed in excess, not in the places where it should normally be. MARS is mainly detected in children in the first 2–3 years of life and does not tend to progress. Many MARS disappear as the child grows.
Reasons for the development of MARS?
Multiple factors are believed to be involved in the formation of MARS. There are two large groups - external and internal. External factors include the influence of the environment, the diet of the pregnant woman, diseases of the body, taking medications during pregnancy, radiation, smoking, alcohol, and stress. Internal factors include: heredity, genetic and chromosomal abnormalities.
What heart abnormalities occur in children?
The most well-known and common MARS is mitral valve prolapse (MVP). MVP is the sagging of the bicuspid valve at the moment of contraction of the heart into the cavity of the left ventricle, due to which a slight turbulence in the blood flow in the heart occurs. Only the first degree of prolapse is classified as MARS. All other degrees are accompanied by severe circulatory disorders and should be considered heart defects.
A fairly common second MARS is additional chords in the cavity of the left ventricle (LVAD) or otherwise abnormal chords (LV ARCH). This is MARS, which manifests itself in the presence inside the ventricular cavity of additional strands of connective tissue or muscles attached to the walls of the ventricle or the interventricular septum. Normally they are attached to the valve flaps. Most often, false (additional) chords occur in boys. False chords can be single or multiple, occurring both separately and in combination with other anomalies. The location can be along the blood flow, across it or diagonally. The severity of the heart murmur will depend on this. Chords can cause rhythm disturbances, so patients require special supervision by a cardiologist.
The third common MARS is patent foramen ovale (PFO). A variant of the norm is the presence of a minor defect of up to 2 - 3 mm under the age of one year. But when it is present at an older age, in some cases we are talking about a developmental anomaly (when the defect size is up to 5 mm), in others – about heart defects (when the defect is pronounced and there is a circulatory disorder).
How does MARS manifest itself?
In most cases, MARS does not manifest itself in any way, and children are no different from their peers. Very rarely, but there may be complaints of pain in the heart area, a feeling of interruptions in the heart, surges in blood pressure, arrhythmias on the electrocardiogram.
Very often, cardiac anomalies are combined with other connective tissue anomalies: vision, skeleton, skin, gall bladder, kidneys. Therefore, the manifestations will be systemic, that is, at the level of the entire organism. These changes can be either minimal or quite pronounced.
A careful examination of the child can reveal scoliosis (curvature of the spine), various forms of flat feet, hypermobility (excessive mobility of the joints). The most common combinations of MARS are the gastroesophageal reflex (return of stomach contents into the esophagus), inflection of the gallbladder, megaureter (dilation of the ureter). In addition, MARS is often accompanied by neurovegetative disorders - the peripheral and central nervous systems work unbalanced. This can manifest itself as urinary incontinence, speech impediment, vegetative-vascular dystonia, and behavioral disturbances. All these combinations do not lead to severe dysfunction of organs and systems and do not impair the child’s life.
What complications can there be?
Not always, but in some cases, disturbances in heart rhythm and disturbances in the conduction of impulses through the heart may be observed, which are detected on the electrocardiogram and are accompanied by complaints of pain in the heart and palpitations. This requires additional examination by a cardiologist. As a rule, these disorders are characteristic of mitral valve prolapse (MVP) and abnormally located chordae.
What is the treatment for this syndrome?
The basic principles of treating children with MARS are:
- Maintaining a daily routine. Elimination of psycho-emotional stress, sleep no less than the required number of hours according to age.
- A balanced and balanced diet with the obligatory inclusion of foods rich in magnesium and potassium (legumes, fresh herbs and vegetables, various cereals, dried fruits).
- Water treatments, massage, physiotherapy.
- Physical education class.
- Vitamins (group B) and magnesium preparations (magnesium B6, Magnerot, Magvit)
Summary
MARS is a syndrome, it is not a death sentence, it is a special condition of a child that requires observation and minor correction. This is not a reason to limit your child from physical activity. There is no need to treat a child diagnosed with MARS as a patient. Most MARS progress favorably and the child is not affected in any way. All you need to do is change your lifestyle and regularly see a cardiologist. Healthcare Institution "11th City Children's Clinic" Cardiologist, Ph.D. Bandazhevskaya G.S.
Myxoma of the heart - symptoms and treatment
The pathogenesis of cardiac myxoma is not well understood. Presumably, it develops from the embryonic endothelium of the parietal endocardium. The severity and nature of the disorders depend on the size and location of the tumor.
Left atrial myxoma narrows the mitral orifice and causes obstruction of the pulmonary veins, which causes pulmonary venous and arterial hypertension, as well as secondary right ventricular heart failure.
The myxoma can protrude into the left ventricle, then when it contracts (in early systole), the tumor moves from the ventricle to the atrium. As a result, the pressure in the atrium greatly increases.
When the left ventricle relaxes (early diastole), the tumor protrudes into the ventricular cavity, causing the pressure inside the atrium to sharply decrease. If the tumor does not protrude, it obstructs the flow of blood through the atrioventricular opening. Blood movement slows down, which is similar to tricuspid or mitral stenosis.
Right atrial myxoma reduces the right atrioventricular orifice and impedes the outflow of blood from the vena cava, which causes systemic venous hypertension to develop.
Left ventricular myxoma leads to narrowing (stenosis) of the left ventricular outflow tract. The course of the disease resembles obstructive cardiomyopathy: the left ventricle is greatly enlarged and the outflow of blood from it is impaired.
Myxoma of the right ventricle can lead to the development of pulmonary artery stenosis. When the right ventricle contracts, blood flows poorly into the pulmonary artery [9]. Manifested by fainting, angina and shortness of breath.
According to the concept of American researchers, some manifestations of myxoma are not directly related to its action. Scientists included fever, vasculitis, hematological changes and constitutional symptoms to such manifestations. Presumably, they arise due to the production of cytokines by the tumor: interleukins, vascular endothelial growth factors, basic fibroblast growth factor and monocyte chemotactic protein-1. Cytokines are involved in tumor growth, relapse and the appearance of distant metastases.
Traditionally, myxomas are considered benign neoplasms, but in the literature there are references to the fact that they can metastasize. They should be considered a rare complication of myxoma. Distant metastases of cardiac myxoma have been detected in the brain, lungs, bones and soft tissues before diagnosis or several years after removal of the primary tumor [17].