1.What is mitral valve regurgitation?
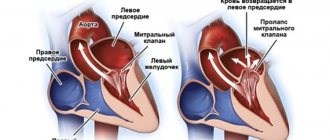
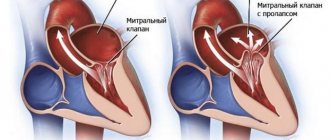
Mitral valve regurgitation
characterized by an unnatural flow of blood from the left ventricle into the left atrium during
systole
- contraction of the heart muscle.
When the heart valve is working properly, blood moves from the atrium to the ventricle. Against the background of rheumatic fever, dilation of the mitral valve ring, ischemic dysfunction of the papillary muscles and other unfavorable factors, the direction of blood flow changes in the opposite direction.
According to statistics, about 70% of the world's population is affected by mitral regurgitation. Minor manifestations of this pathological process can occur even in absolutely healthy people.
A must read! Help with treatment and hospitalization!
Treatment
Treatment of MVP depends on the patient's health status and associated factors. The goal of treatment is to improve heart function, minimize unpleasant symptoms, and avoid future complications.
- Drug treatment.
Of course, pills and injections will not be able to restore a damaged mitral valve. But the right medications will help prevent the formation of blood clots and fluid accumulation.
- Surgery.
Surgery is the optimal treatment method. But this method may be contraindicated during pregnancy.
- Waiting tactics.
Patients diagnosed with primary moderate prolapse do not require surgical treatment. But regular examinations by a cardiologist will be necessary in order to begin the necessary treatment on time.
2.Why does mitral regurgitation occur?
The mitral valve is a kind of valve that separates the left atrium from the ventricle. Due to various factors that impair its functioning, the valve does not fit tightly enough to the walls of the ventricle. As a result, the two connecting plates - components of the valve - cannot effectively block the reverse flow of blood, placing additional stress on the heart to normalize the circulation of blood flow. This phenomenon does not pass without leaving a trace on the human body. The consequences of mitral valve regurgitation can include diseases such as arrhythmia, heart failure and endocarditis.
There are two main forms of mitral regurgitation: chronic and acute. Let us consider in more detail their differences and features of the course.
- Acute mitral regurgitation.
Acute regurgitation of the mitral valve occurs against the background of various cardiac pathologies: dysfunction or rupture of the papillary muscles, acute rheumatic fever, infective endocarditis, rupture of the mitral valve leaflets, dilatation of the left ventricle. Acute regurgitation develops instantly. Due to possible severe bleeding caused by rupture of cardiac tissue, it can be life-threatening. - Chronic mitral regurgitation.
The causes of chronic regurgitation of the mitral valve are also associated with heart diseases - mitral valve prolapse, expansion of its ring. The chronic form of regurgitation is much more common than the acute form. It is characterized by slow and gradual development, so the disease is most often diagnosed in older people.
Visit our Cardiology page
Diagnostics of the process and detailing of complaints
The disease can only be diagnosed after the patient seeks help. Mitral valve regurgitation of the 1st degree (up to 5 ml) is not clinically manifested. Symptoms occur with more significant hemodynamic disturbances.
Long-term concealment of mitral insufficiency is ensured by thickening of the left ventricular myocardium. However, when the reserves of this mechanism are depleted, the patient’s condition sharply worsens.
There are 5 stages of mitral insufficiency.
| Stage | Complaints | Hemodynamic disorders | Treatment |
| Compensation | None | Clinically insignificant regurgitation, up to 1+ (no more than 5 ml) | Not required |
| Subcompensations | Shortness of breath when walking long distances or running | Regurgitation within 2+ (about 10 ml). Left heart: ventricular hypertrophy, atrial dilatation | Surgical treatment is not indicated |
| Right ventricular decompensation | Breathing problems with minor exercise | Significant regurgitation, 3+. Dilatation of the left ventricle, enlargement of the right sections. | Surgical treatments are recommended |
| Dystrophic | Shortness of breath without external causes, cough, swelling, fatigue | Deterioration of the pumping function of the heart, relative insufficiency of the tricuspid valve | Surgical treatment indicated |
| Terminal | The patient's condition is serious. Hemoptysis, cough, swelling, poorly healing ulcers. | Decompensation of the circulatory system | Treatment not indicated |
The army will not accept for military service a person with regurgitation of the second degree or higher!
Typical complaints with mitral insufficiency:
shortness of breath (initially with significant physical activity, in the terminal stages - on an ongoing basis);- palpitations (during physical activity);
- acrocyanosis (blue discoloration of fingertips);
- “mitral butterfly” (blue blush on the cheeks);
- cardialgia (pain in the heart of an aching or pressing, sometimes stabbing nature, not necessarily associated with stress);
- swelling in the legs (appears in the afternoon, in the evening, in the initial stages disappears overnight);
- pain in the right hypochondrium (appears as a result of blood stagnation, with pronounced swelling);
- cough (with stagnation of blood in the pulmonary circulation, often unproductive);
- hemoptysis (with decompensation of the patient’s condition).
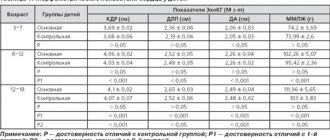
Hemodynamic disorders can be diagnosed using the following instrumental methods:
- electrocardiography (left ventricular hypertrophy, arrhythmias, after the third stage - right ventricular hypertrophy);
- phonocardiography (the first tone is weakened, a systolic murmur is determined at the apex of the heart);
- echocardiography (enlargement of the heart cavities and thickening of the myocardium, changes in the movements of the interventricular septum, calcifications in the mitral valve leaflets);
- Doppler echocardiography (detection of the return of part of the blood to the atrium during ventricular systole).
3. Symptoms of the disease
Chronic mitral regurgitation is characterized by the absence of symptoms for many years. As a rule, patients do not know about heart disease for a long time, the symptoms of which appear gradually. The acute form of regurgitation is much more serious and is accompanied by the same symptoms as cardiogenic shock and acute heart failure.
We list the main symptoms of mitral valve regurgitation:
- constant shortness of breath;
- weakness and increased fatigue;
- dizziness;
- pain in the chest;
- confusion;
- swelling of the lower extremities.
If you notice at least two of the above symptoms, be sure to contact a good cardiologist. You may need immediate treatment.
About our clinic Chistye Prudy metro station Medintercom page!
Causes
Mitral regurgitation of the 1st degree tends to manifest itself in both chronic and acute forms. Among the most significant factors that can provoke the disease are the following:
- infectious endocarditis;
- rheumatism;
- development of physiological pathologies of the mitral valve;
- Congenital heart defect;
- acute form of myocardial infarction;
- chest injury;
- angina pectoris;
- the patient has chronic heart or lung disease.
One or more of the provoking factors listed above sooner or later leads to sagging of the mitral valve walls.
Diagnosis of mitral regurgitation is often accompanied by concomitant ailments:
- disruption of the functioning and anatomy of the papillary muscles;
- the process of damage to the endodermis of the heart by various types of infections;
- increased volume of the left cardiac ventricle;
- cardiac ischemia;
- development of rheumatoid processes.
The possibility of detecting mitral regurgitation in small children or newborns cannot be ruled out.
In this case, the following processes may occur simultaneously:
- myocarditis;
- the formation of a fairly thick layer of protein on the inner wall of the lining of the heart or its valvular region;
- tricuspid congenital heart defects;
- thrombosis;
- atrial fibrillation.
I would like to note that diagnosing grade 1 mitral regurgitation is a rather complex and painstaking process.
With the development of an acute form of the disease, patients can simultaneously detect pulmonary edema, as well as ventricular failure of the heart.
The diagnosis of grade 1 mitral regurgitation is accompanied by a fairly large number of concomitant ailments.
If the diagnosis is not made in a timely manner or if the course of treatment is incorrectly prescribed, these diseases significantly aggravate the patient’s condition.
4. Diagnosis and treatment of mitral valve regurgitation
Diagnosis of mitral valve regurgitation may include:
- medical examination;
- echocardiogram - a procedure based on the use of sound waves to determine the shape, size and structure of heart tissue;
- chest x-ray;
- electrocardiogram of the heart, which allows to detect irregularities in the heart rhythm;
- cardiac catheterization - examination of the cavities of the heart, as well as nearby blood vessels, using a hollow flexible tube.
These tests not only detect mitral regurgitation, but also determine the degree of mitral regurgitation. The information obtained during the study is the basis on which further treatment is based.
The choice of treatment for mitral valve regurgitation depends primarily on the form of the disease, as well as the degree of its progression.
For example, in chronic cases, doctors most often prescribe constant monitoring of the patient’s heart condition and the use of special medications to eliminate the symptoms of the disease. These drugs include:
- vasodilators – a group of vasodilating drugs;
- diuretics and diuretics;
- anticoagulants - drugs that prevent the formation of blood clots.
If necessary, your doctor may recommend surgery to repair or replace the mitral valve. Patients with mitral regurgitation need to radically change their lifestyle in order to reduce the load on the heart. Doctors recommend avoiding intense physical activity and emotional stress, leading a healthy lifestyle and eating right.
Classification
Diagnosed cases of the disease in adolescents and adults are divided into two types:
- MVP with a high risk of developing regurgitation;
- moderate prolapse with a low risk of developing minor regurgitation.
Doctors can also divide the disease into stages:
- moderate prolapse 0-1 degree: also known as primary (even during pregnancy, no negative symptoms are felt; the body independently regulates the additional load on the heart);
- MVP stage 2 (transitional): signs - intracardiac pressure increases, in adolescents and during pregnancy there is constant shortness of breath and fatigue;
- 3rd (decompensated stage): significant damage to the heart muscle can be diagnosed.
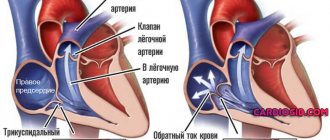
Tricuspid regurgitation
Isolated lesions of the tricuspid valve (TC) are quite rare. As a rule, its insufficiency with regurgitation is a consequence of pronounced changes in the left half of the heart (relative TC insufficiency), when high pressure in the pulmonary circulation prevents adequate cardiac output into the pulmonary artery, which carries blood for oxygenation into the lungs.
Tricuspid regurgitation leads to disruption of complete emptying of the right half of the heart, adequate venous return through the vena cava and, accordingly, congestion appears in the venous part of the systemic circulation.
For tricuspid valve insufficiency with regurgitation, the occurrence of atrial fibrillation, cyanosis of the skin, edematous syndrome, swelling of the neck veins, enlarged liver and other signs of chronic circulatory failure are quite typical.
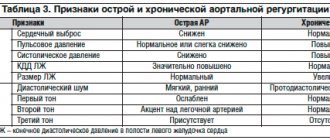
Pathophysiology
The main pathological factor in AR is LV volume overload, which entails a series of compensatory adaptive changes in the myocardium and the entire circulatory system (Table 2).
The main determinants of regurgitant volume are: the area of the regurgitant orifice, the diastolic pressure gradient across the aortic valve and the duration of diastole, which in turn is a derivative of the heart rate. Thus, bradycardia contributes to an increase, and tachycardia - to a decrease in AR volume.
A gradual increase in end-diastolic volume (EDV) leads to an increase in the systolic tension of the LV wall with subsequent hypertrophy, accompanied by simultaneous expansion of the LV cavity (eccentric LVH), which allows the increased pressure in the LV cavity to be evenly distributed to each myocardial motor unit (sarcomere) and thereby helps maintain stroke volume and ejection fraction within normal or suboptimal limits (compensation stage).
An increase in the volume of regurgitation leads to a progressive expansion of the LV cavity, a change in its shape to spherical, an increase in LV diastolic pressure, increased systolic tension of the LV wall (afterload) and a decrease in ejection fraction. A drop in ejection fraction occurs due to decreased contractility and/or increased afterload (decompensation stage). AR is divided into acute and chronic.
Acute aortic regurgitation
The most common causes of acute AR are: infective endocarditis, aortic dissection, or trauma. In acute AR, there is a sudden increase in the diastolic volume of blood entering the unchanged LV. The lack of time for the development of adaptive mechanisms leads to a sharp increase in EDV both in the LV and in the left atrium. For some time, the heart works according to the Frank-Starling law, according to which the degree of contraction of myocardial fibers is a derivative of the length of its fibers. However, the inability of the heart chambers to rapidly compensatory expansion soon leads to a decrease in the volume of ejection into the aorta. The resulting compensatory tachycardia is not enough to maintain sufficient cardiac output, which leads to the development of pulmonary edema and/or cardiogenic shock.
Particularly pronounced hemodynamic disturbances are observed in patients with concentric LV hypertrophy caused by pressure overload and discrepancy between the sizes of the LV cavity and EDV. This situation is observed in the case of aortic dissection due to systemic hypertension, as well as in acute AR after balloon commissurotomy for congenital AS.
Chronic aortic regurgitation
In response to an increase in blood volume during chronic aortic regurgitation, a number of compensatory mechanisms are activated in the LV, facilitating its adaptation to the increased volume without increasing filling pressure.
The gradual increase in diastolic volume allows the ventricle to pump out a larger stroke volume, which determines normal cardiac output. This is ensured by the longitudinal replication of sarcomeres and the development of eccentric hypertrophy of the LV myocardium. Thanks to this, the load on the sarcomere remains normal for a long time, maintaining a preload reserve. Thus, the ejection fraction and fractional shortening of LV fibers remain within normal limits.
A further increase in the size of the cavities of the left chambers of the heart, combined with increased systolic wall tension, leads to the occurrence of concomitant concentric LVH. Thus, AR is a combination of volume and pressure overload (compensation stage).
Subsequently, both the depletion of the preload reserve and the development of LV hypertrophy that is inappropriate for the volume occur with a subsequent decrease in the ejection fraction (decompensation stage) (Table 1).
Pulmonary valve regurgitation
Damage to the pulmonary valve leaflets can be congenital, manifesting itself in childhood, or acquired as a result of atherosclerosis, syphilitic lesions, or changes in the leaflets due to septic endocarditis. Often, damage to the pulmonary valve with insufficiency and regurgitation occurs with existing pulmonary hypertension, lung diseases, and damage to other heart valves (mitral stenosis).
Minimal regurgitation on the pulmonary valve does not lead to significant hemodynamic disorders, while a significant return of blood to the right ventricle, and then to the atrium, causes hypertrophy and subsequent dilatation (expansion) of the cavities of the right half of the heart. Such changes are manifested by severe heart failure in the systemic circle and venous stagnation.
Pulmonary regurgitation is manifested by all kinds of arrhythmias, shortness of breath, cyanosis, severe edema, accumulation of fluid in the abdominal cavity, changes in the liver up to cirrhosis and other signs. With congenital valve pathology, symptoms of circulatory disorders occur already in early childhood and are often irreversible and severe.
Features of regurgitation in children
In childhood, the proper development and functioning of the heart and circulatory system is very important, but disorders, unfortunately, are not uncommon. Most often, valve defects with insufficiency and return of blood in children are caused by congenital developmental anomalies (tetralogy of Fallot, hypoplasia of the pulmonary valve, defects of the septa between the atria and ventricles, etc.).
Severe regurgitation with an abnormal structure of the heart manifests itself almost immediately after the birth of a child with symptoms of respiratory distress, cyanosis, and right ventricular failure. Often, significant violations end fatally, so every expectant mother needs to not only take care of her health before the intended pregnancy, but also promptly visit an ultrasound diagnostic specialist during pregnancy.
Possibilities of modern diagnostics
Medicine does not stand still, and the diagnosis of diseases is becoming more reliable and of high quality. The use of ultrasound has made significant progress in detecting a number of diseases. The addition of ultrasound examination of the heart (EchoCG) with Dopplerography makes it possible to assess the nature of blood flow through the vessels and cavities of the heart, the movement of valve leaflets at the time of myocardial contractions, establish the degree of regurgitation, etc. Perhaps EchoCG is the most reliable and informative method for diagnosing cardiac pathology in the mode real time and at the same time being accessible and inexpensive.
mitral regurgitation on echocardiography
In addition to ultrasound, indirect signs of regurgitation can be detected on an ECG, with careful auscultation of the heart and assessment of symptoms.
It is extremely important to identify disorders of the heart valve apparatus with regurgitation not only in adults, but also during fetal development. The practice of ultrasound examination of pregnant women at different stages makes it possible to detect the presence of defects that are beyond doubt even during the initial examination, as well as to diagnose regurgitation, which is an indirect sign of possible chromosomal abnormalities or developing valve defects. Dynamic observation of women at risk makes it possible to timely establish the presence of serious pathology in the fetus and resolve the issue of the advisability of continuing pregnancy.
Etiology
Aortic regurgitation can be caused either by primary damage to the aortic valve leaflets or by damage to the aortic root, which currently accounts for more than 50% of all cases of isolated AR (Table 1).
Valve damage
- Rheumatic fever is one of the main valvular causes of AR. Wrinkling of the leaflets due to infiltration by connective tissue prevents their closure during diastole, thereby forming a “defect” in the center of the valve, which is a window for regurgitation of blood into the LV cavity. Concomitant fusion of the commissures limits the opening of the aortic valve, which leads to the appearance of concomitant aortic stenosis (AS).
- Infectious endocarditis. AR may be caused by valve destruction, perforation of its leaflets, or the presence of growing vegetations that prevent the leaflets from closing in diastole.
- Calcified AS in elderly people leads to the development of AR in 75% of cases, both due to age-related expansion of the fibrous ring of the aortic valve and as a result of aortic dilatation.
- Other primary valvular causes of AR are:
- trauma leading to rupture of the ascending aorta. In this case, the attachment of the commissures is disrupted, which leads to prolapse of the aortic cusp into the LV cavity;
- congenital bicuspid valve due to incomplete closure or prolapse of its valves;
- large septal defect of the interventricular septum;
- membranous subaortic stenosis;
- complication of radiofrequency catheter ablation;
- myxomatous degeneration of the aortic valve;
- destruction of the biological valve prosthesis.
Aortic root damage
Diseases that can cause aortic root damage include: age-related (degenerative) dilatation of the aorta, cystic necrosis of the aortic media (isolated or as a component of Marfan syndrome), aortic dissection, osteogenesis imperfecta (osteopsatyrosis), syphilitic aortitis, ankylosing spondylitis, Behçet's syndrome, psoriatic arthritis, ulcerative colitis arthritis, relapsing polychondritis, Reiter's syndrome, giant cell arteritis, systemic hypertension, and the use of certain appetite suppressants.
AR in these cases is formed due to pronounced expansion of the aortic valve ring and aortic root with subsequent separation of the leaflets. Subsequent dilatation of the root is inevitably accompanied by excessive tension and bending of the valves, which then thicken, wrinkle and become unable to completely cover the aortic opening. This, in turn, aggravates AR, leads to further expansion of the aorta and closes the vicious circle of pathogenesis (“regurgitation increases regurgitation”).
Regardless of the cause, AR always causes dilatation and hypertrophy of the left ventricle, with subsequent dilation of the mitral annulus and the possible development of left atrium dilatation. Often, “pockets” form on the endocardium at the site of contact between the regurgitant flow and the LV wall.