Tricuspid valve prolapse is a rare heart disease of organic origin. This defect is found in one person out of 10 thousand. Most often, it is diagnosed in males who have a history of coronary heart disease or coronary circulatory pathology.
The tricuspid valve connects the right atrium and the right ventricle. Its function is to ensure the movement of blood towards the aorta and pulmonary artery and limit its flow back into the atrium.
The defect in the functioning of this heart valve is that it does not close completely or sag into the right atrium during diastole, which causes blood to flow in the opposite direction to normal blood flow (this process is called regurgitation). Pathological changes in the functioning of this valve are caused by processes of degeneration and dysplasia of its cells, so it loses its natural elasticity and seems to “fall in.”
Causes
The development of tricuspid valve prolapse is provoked by congenital or acquired factors.
- Disruption of normal intrauterine development, when the fetus can be affected by various toxic substances (with uncontrolled self-medication of the mother with pharmacological drugs, abuse of bad habits).
- Fetal hypoxia, insufficient oxygen supply.
- Toxicoses of a pregnant woman.
- Rhesus conflict between mother and fetus.
- Nutrient deficiency in a woman’s diet, fasting, strict diets.
- Genetic anomalies caused by the inheritance of defective chromosomes (Ehlers-Danlos syndrome, Marfan syndrome, congenital contractural arachnodactyly, elastic pseudoxanthoma).
- Rheumatism or rheumatoid arthritis.
- Cardiomyopathies.
- Pathologies of other heart valves (mitral and aortic).
- Complications after viral or bacterial diseases in early childhood (purulent tonsillitis, glomerulonephritis, pneumonia).
- Tumors in which the body produces a special substance that destroys myocytes (heart cells).
- Infectious heart diseases (myocarditis, pericarditis, endocarditis).
- Hyperthyroidism, thyrotoxicosis.
- Traumatic injuries to the chest (bruises, wounds, hematoma formation).
- Destruction of heart fibers due to the toxic effects of medications, drugs, ethyl alcohol.
- Bronchopulmonary diseases with impaired ventilation of organs.
- Cirrhosis of the liver.
- Autoimmune pathologies.
- Immunodeficiencies.
- Systemic diseases (scleroderma, lupus erythematosus, vasculitis).
- Hormonal or metabolic diseases.
- Arteritis.
- Exposure to ionizing radiation and poor ecology.
Magazine "Child's Health" 2(5) 2007
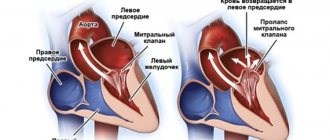
Mitral valve prolapse (MVP), which is based on structural and functional disorders of the mitral valve of the heart, leading to bending of the valve leaflets into the cavity of the left atrium at the time of left ventricular systole, occupies a leading place in the structure of childhood diseases.
In recent years, the incidence of MVP has increased, therefore, despite the fact that the most characteristic auscultatory manifestation of the MVP phenomenon is the presence of systolic clicks (clicks) in combination with systolic murmur, with the widespread introduction of ultrasound research methods into practice, it became clear that even the absence of any - complaints, clinical symptoms and auscultatory changes do not exclude the possibility of its existence [1, 2].
At the present stage, the etiopathogenetic heterogeneity of the MVP phenomenon has been convincingly proven, manifested by clinical polymorphism and represented by such most recognized factors as, firstly, congenital microanomalies of the architecture of the valves, chords and atrioventricular ring, which over time, due to repeated microtraumas against the background of hemodynamic influences, become more pronounced, accompanied by excess production of collagen, predominantly type 3, in the valve stroma, and, secondly, the theory of a primary defect in the development of the connective tissue apparatus of the mitral valve, which is combined with an increase in the number of stigmas of disembryogenesis [2, 7, 14]. The clinical manifestations of MVP are influenced by: the degree of valve prolapse, the background against which MVP is detected, the nature of electrocardiographic abnormalities, and the presence of complications [8–10, 13].
Currently, the attention of clinicians is attracted by anomalies in the development of the choral apparatus of the heart, which occur in children in an average of 38% of cases [1]. The frequency of MVP, which is also a developmental anomaly, in children ranges from 3–5% at the age of up to 1 year, increasing by 14 years to 22–31% and depends on the diagnostic method [7]. Considering the prevalence of MVP among the pediatric population, pediatricians and cardiologists need to lean toward greater clinical vigilance and prevention of possible complications [1].
The purpose of this study was to study the effectiveness of complex therapy for clinical manifestations of MVP based on the results of prospective observation of children in the cardiology department of Children's Clinical Hospital No. 5 in Zaporozhye.
Material and methods
703 children (280 boys and 423 girls) from 3 to 18 years old were under observation. There were 108 (15.36%) children aged 3 to 7 years; from 8 to 12 years - 243 (34.57%); from 13 to 18 years old - 352 (50.1%) children.
All children underwent a comprehensive clinical examination, taking into account complaints, anamnestic data, results of physical examination methods, general clinical laboratory and instrumental (electrocardiography, echocardiography with Doppler ultrasound) research methods using standard methods. To diagnose concomitant somatic pathology, the children were examined by an otolaryngologist, neurologist, ophthalmologist, orthopedic surgeon, endocrinologist, dentist, and the girls were examined by a gynecologist. The nature of cardiac disorders was assessed according to ICD-10 recommendations.
The results obtained were processed using traditional statistical methods using Excel [4, 12].
Depending on the clinical manifestations, all observed children were divided into 3 groups: MVP with rhythm disturbance and electrocardiographic symptoms (short P-Q syndrome, WPW syndrome, long QT syndrome), MVP as a manifestation of connective tissue dysplasia, and MVP with clinical signs of dysfunction of the autonomic nervous system .
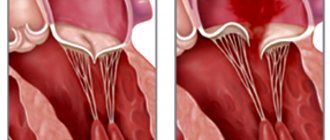
The patients underwent echocardiographic examination in M- and B-modes and Doppler ultrasound in constant wave and pulse modes using an Aloka SSD-630 device. The generally accepted criteria for identifying PMC were used [1, 2, 7]. Also, two-dimensional echocardiography made it possible to detect morphological microanomalies in the structure of the valve apparatus that underlie the occurrence of mitral valve prolapse in the form of ectopic attachments or impaired distribution of tendon filaments, changes in the configuration and position of the papillary muscles, elongation of tendon filaments, and redundancy (enlargement) of the valve leaflets. Transmitral blood flow and mitral valve function were quantitatively assessed using Doppler ultrasound. Mitral valve regurgitation was diagnosed by the presence of turbulent systolic flow under the mitral valve leaflets in the left atrium. The following gradations of regurgitation magnitude were adopted:
— 1st degree (+) — systolic regurgitation in the area under the mitral valve;
— 2nd degree (++) — systolic regurgitation extends to 1/3 of the cavity of the left atrium;
— 3rd degree (+++) — spread of systolic regurgitation to 1/2 of the cavity of the left atrium;
— 4th degree (++++) — spread of regurgitation to more than 1/2 of the cavity of the left atrium [1, 7].
Results and discussion
Over the past five years, according to our observations, the number of children with MVP has increased in dynamics from 18.5% in 2002 to 29% in 2006, which is explained by both the expansion of the capabilities of ultrasound diagnosis of MVP (EchoCG) and the increase in the prevalence of connective dysplasia syndrome tissues with manifestations of dysfunction of the autonomic nervous system in children.
As a result of the study, it was established that in adolescents MVP is diagnosed significantly more often than in other age groups, with a predominance in girls in a ratio of 2: 1. In other groups of children studied, this pathology occurs equally often in both boys and girls.
All children, regardless of the severity of MVP, presented almost the same type of complaints, the variability of which varied depending on the degree of autonomic disorders. There was pain and heaviness in the heart area, a feeling of lack of air, and frequent deep sighs. A number of children experienced paroxysmal conditions, which manifested themselves as an atypical attack of suffocation, mainly after physical exertion and psycho-emotional stress. These conditions in children with severe MVP (as a rule, these are vagotonic children) were regarded as vegetative crises. Often, such children had syncope during follow-up.
Changes in the electrocardiogram (ECG) in the form of extrasystole, long QT syndrome, WPW syndrome were noted in 24% of children with MVP, MVP in combination with other manifestations of connective tissue dysplasia (joint hypermobility, myopia, high “Gothic” palate, low position of the ears, flat feet, asthenic constitution, etc.) were observed in 12% of patients, 64% of children were diagnosed with severe autonomic disorders.
According to the echocardiographic study, depending on the severity of MVP, MVP of the 1st degree was significantly more common and was recorded in 609 children examined (86.6%), MVP of the 2nd degree was detected less often - in 81 children (11.5%), 3rd degree - in 10 people (1.5%), 4th degree - in 3 children (0.4%).
The examined patients had predominantly holosystolic and late systolic variants of prolapse (98%). In 9 patients, Doppler ultrasound examination revealed 1st degree mitral regurgitation, despite the presence of MVP greater than 7 mm.
Morphometric parameters of the heart in the examined children are presented in Table. 1. The echocardiographic examination revealed in children of all age groups, in comparison with controls, only a tendency towards an increase in the size and mass of the left ventricular myocardium. The data obtained do not contradict the literature data [1] that in children with mitral valve prolapse and metabolic disorders of the myocardium, the end-diastolic volume of the left ventricle increases by an average of 20%.
Indicators of pumping and contractile function of the myocardium in the examined children are presented in Table. 2. The analysis showed that in children with MVP in all age groups, the indicators that characterized the pumping ability (EF and %ΔD) and contractility of the left ventricular myocardium (n.Sk.ser. and Sk.ts.) also tended to decrease in comparison with control groups, which is associated with the development of metabolic disorders in the myocardium.
Indicators of the systolic amplitude of movement of the posterior wall of the left ventricle and the interventricular septum, which indirectly characterize the state of the pumping function of the left ventricle, were reduced in children with MVP in all 3 age groups compared to the controls. Changes in the kinetics of the heart muscle, which turned out to be a violation of the movement of the interventricular septum and the posterior wall of the left ventricle, were mainly recorded in the form of hypokinesia of the posterior wall of the left ventricle and the interventricular septum.
Thus, in children with MVP, there are structural prerequisites for the formation of hemodynamic disorders, which are important in the diagnosis and development of diseases of the cardiovascular system in this group of patients and are characterized so far only by a tendency to increase the end-diastolic size and mass of the left ventricle with a decrease in indicators its contractility and contractility.
Taking into account the peculiarities of the clinical manifestations of MVP, we maximally individualized the treatment and management tactics of children, taking into account age, gender, heredity, the presence and nature of dysfunction of the autonomic nervous system, as well as the degree of prolapse of the mitral valve leaflets. Depending on the severity and nature of clinical manifestations, appropriate drug therapy was prescribed. Children with dysfunction of the autonomic nervous system underwent correction of autonomic disorders.
The main aspects of the recommended therapy included the normalization of the daily routine with alternating physical and mental activity. Without exception, everyone was prescribed therapeutic exercises and a visit to the pool. The department widely used physiotherapeutic treatment methods, in particular galvanization using the reflex-segmental technique. In the last 2 years, the department has introduced the administration of drugs immediately before galvanization (thiotriazoline was administered intramuscularly 2 hours before), which ensured a direct effect of the drug on the heart muscle during metabolic changes. In complex therapy, electrophoresis of medicinal substances on the upper cervical spine was widely used: for vagotonic dysfunctions - with calcium, for sympathicotonic dysfunctions - with bromine. The darsonvalization method was used very widely and successfully.
Almost all children were prescribed herbal remedies that have a sedative effect. Children with vagotonic tendencies were prescribed herbal adaptogens: tincture of ginseng, eleutherococcus.
Drugs that improve the metabolism of the central nervous system have proven themselves well. To improve microcirculation, cinnarizine was prescribed for 2–3 weeks. If changes in the rheoencephalogram of children were recorded in the form of difficulty in venous outflow, accompanied by frequent exacerbations of respiratory neurosis, bellataminal was prescribed for 2–3 weeks.
All children were required to be prescribed courses of cardiometabolites for the prevention and treatment of metabolic changes (riboxin, ATP, etc.). Antihomotoxic drugs were also used in the complex treatment of patients with MVP.
When MVP was combined with sinus tachycardia, extrasystole, long QT syndrome, and syncope, beta-blockers were prescribed: atenolol, metoprolol or propranolol in an individually selected dose (1–2 mg/kg) for 2–4 months, followed by gradual withdrawal. Beta-blockers were also recommended for children with severe mitral regurgitation and prolapse of the mitral valve leaflets of the 3rd degree. Children with persistent rhythm disturbances without prolongation of the QT interval on the ECG were prescribed antiarrhythmic drugs (cordarone). Also, in children with MVP, brain metabolites (piracetam), vascular drugs (cinnarizine), membrane stabilizers (Aevit), and antisclerotic agents (lidase) were used for heart rhythm disturbances.
Since many clinical manifestations of MVP can progress, all of our patients with this pathology were hospitalized in the cardiology department two to three times a year. A control echocardiographic study with Doppler ultrasound 6 months after complex treatment revealed clear positive dynamics in the course of the disease in 594 (84.5%) children. Among them, in 48 (8.1%) children, MVP was no longer registered, in 71 (11.9%) children, the degree of prolapse decreased, in 59 (9.9%) patients, cardiac arrhythmias disappeared and electrocardiographic study indicators normalized, in 6 (1%) patients no longer had mitral regurgitation.
Considering the existing possibility of complications from the cardiovascular system in the form of the formation of mitral valve insufficiency, secondary bacterial endocarditis, all patients with mitral valve prolapse were subsequently under medical supervision of a local pediatrician and cardio-rheumatologist, and children with an auscultatory form of MVP accompanied by regurgitation were required to undergo Antibacterial prophylaxis was carried out during dental procedures and surgical interventions.
The results of a comprehensive examination of children with MVP showed that in the occurrence of leaflet prolapse in these children, several factors were simultaneously important, the main ones being: inferiority of the connective tissue structures of the valve, minor anomalies of the valve apparatus, dysfunction of the autonomic nervous system, contributing to hemodynamic dysregulation. Timely diagnosis of MVP and a high probability of developing possible complications make it possible to recommend effective therapy, clinical observation and adequate physical activity for this group of children.
conclusions
1. Recently, there has been an increase in the number of children with MVP, especially teenage girls.
2. In the structure of all identified MVP in children, MVP of the 1st degree was significantly more common (86.6%), and less often - of the 2nd degree (11.5%), 3rd degree (1.5%), 4 th degree (0.4%).
3. Cardiac connective tissue dysplasia syndrome, represented by mitral valve prolapse, determines the presence of structural prerequisites for the formation of hemodynamic disorders in children.
4. As a result of the complex treatment, positive dynamics were observed in 84.5% of children with MVP, among whom MVP was no longer registered in 8.1%, the degree of leaflet prolapse decreased in 11.9% of those examined, heart rhythm disturbances completely disappeared in 9, 9%, and mitral regurgitation in 1% of children.
5. The prevalence of mitral valve prolapse among children dictates the need for effective therapeutic measures and clinical observation of this group of patients in order to prevent the progression of MVP and the occurrence of complications.
Degrees of tricuspid valve prolapse
- The first is the appearance of moderate regurgitation at the level of the leaflets, which can be detected by ultrasound. Patients have no health complaints and maintain an active lifestyle.
- The second is that the reverse flow of blood increases and reaches the middle of the right atrium. Patients begin to feel interruptions in the work of the heart, their health worsens.
- Third, regurgitation reaches large volumes and is observed throughout the atrium; patients present characteristic complaints of disturbances in the functioning of the heart (rhythm changes, increased pressure, dizziness, chest pain, shortness of breath on exertion or at rest).
- Fourth, up to 40% of the blood enters the right atrium in diastole. The condition of the patients is extremely serious, signs of heart failure are clearly expressed.
In medicine, primary prolapse of the TC (tricuspid valve) and secondary are also distinguished. The first option is easier and is most often caused by pathologies in the functioning of the heart and its vessels. The second is a consequence of pulmonary hypertension, which occurs due to serious pathologies of the lungs or pulmonary artery.
Diagnosis of PMC.
Mitral valve prolapse in the vast majority of cases is detected using non-invasive examinations, the final diagnosis is made using echocardiography, and a number of other studies are also used:
- Interviewing the patient for complaints, collecting anamnesis.
- General blood analysis.
- Blood chemistry.
- Auscultatory examination. The doctor listens to the heart with a stethoscope and can detect a specific click and/or systolic murmur at the apex of the heart that is characteristic of the disease - these sounds decrease with the patient standing, sitting or lying down.
- Electrocardiography (ECG). On it, the doctor can see nonspecific changes in the ST segment and T wave in leads III and aVF, as well as “short PQ syndrome”) and supraventricular tachycardia.
- Echocardiography (ultrasound of the heart). Here the doctor can detect such signs of disease as sagging of the mitral valve leaflets (posterior or both at once) into the cavity of the left atrium in mid-systole, in late systole or throughout systole. Echocardiography is one of the most important examinations in diagnosing MVP in a patient.
- Chest X-ray. It may show signs of smoothed lordosis (but it may also be normal).
- MRI (chest).
After all the studies, the cardiologist prescribes the necessary treatment.
Clinic
Symptoms of the disease increase in direct proportion to the increase in regurgitation.
At the initial stages, the defect can manifest itself by indirect signs:
- rapid fatigue when performing household or professional chores;
- migraine-like headaches;
- nausea combined with slight dizziness;
- sleep disturbances, excessive anxiety.
The following symptoms are characteristic of the height of the disease:
- severe fatigue, weakness even with little physical activity;
- excessive sweating, trembling in the limbs;
- severe swelling in the legs and abdomen;
- palpable and visible pulsation of the veins in the neck;
- decrease in the volume of urine excreted;
- heart rhythm disturbances (tachycardia, arrhythmia, extrasystoles);
- heart pain;
- severe shortness of breath;
- hemoptysis (sometimes);
- pain and discomfort in the right hypochondrium, significant enlargement of the liver;
- rises in blood pressure;
- dyspeptic symptoms: nausea, vomiting (not always);
- dizziness, fainting.
Objective diagnostic signs of the disease (detected by listening, beating the heart, on ultrasound images, x-rays).
- Enlargement of the cardiac borders on the right.
- Myocardial hypertrophy.
- Heart murmurs, especially when inhaling.
- Recording the degree of regurgitation and flexion of valve leaflets during ultrasound examination.
How to recognize atresia?
The manifestations and severity of the clinic depend on the size of the communication between the atria and the blood pressure in the pulmonary artery. With tricuspid valve atresia, newborns have a bluish skin color, which intensifies when crying or breastfeeding.
Children lag behind in physical development, fingers are formed like “drumsticks” and nails like “watch glasses”, edema occurs, congestive liver is observed, sharp attacks of deterioration in health are characteristic - the child becomes restless, choking, sharply turns blue, shortness of breath, palpitations, possible loss of consciousness.
In such a serious condition of the child, surgery is indicated. Without surgical treatment, such children in the first year of life have an extremely unfavorable prognosis.
Treatment
Treatment of tricuspid valve prolapse is based on conservative or surgical measures. The choice of treatment method depends on the degree of damage and the course of the disease.
At the initial stages of the disease, doctors prescribe diuretics, ACE inhibitors, potassium supplements, vitamins, cardiac glycosides, and anticoagulants. The goal of therapy for stage 1 PTC is to stop the weakening of valve contractility and restore normal functioning of the heart muscle.
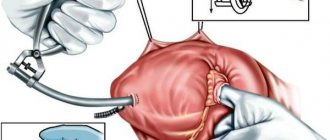
In the later stages of the disease, drug treatment is considered ineffective and patients are offered surgical intervention. It consists of reconstruction of the fibrinous ring of the affected valve or its prosthetics (complete replacement with an implant).
Anomaly or heart defect?
What is the danger?
In order not to drown in the flow of medical terminology, it is necessary to clearly understand the degree of difference between a defect and an anomaly of the development of the heart. Let's look at this difference using the tricuspid valve as an example.
A minor anomaly of cardiac development is an anatomical change in the structure of the heart, which usually does not lead to serious disturbances in the activity of the heart. An example is congenital prolapse of the tricuspid valve.
Heart disease is a gross deviation of the anatomical structure of the heart, which in most cases leads to significant impairment of its function. Example: tricuspid atresia.
Let's talk more about prolapse and atresia.
Prevention and prognosis
- Normalization of the daily routine, rational distribution of loads, adequate sleep.
- Timely treatment of infectious and degenerative diseases of the body.
- Proper nutrition.
- Rejection of bad habits.
- Active lifestyle.
- Pregnant women need to treat gestosis, as well as eliminate harmful effects on the fetus.
Is tricuspid valve prolapse dangerous? Minor TC prolapse has a favorable prognosis. Such patients are monitored by cardiologists and are prescribed diagnostic examinations once a year. Women with this defect can become pregnant and give birth to a healthy child. Of course, subject to constant monitoring at the cardiology center.
If the disease progresses, it is important to promptly perform surgical intervention and restore the functions of the tricuspid valve.
Romanovskaya Tatyana Vladimirovna
Why does atresia occur?
Causes of atresia in a child
The formation of the embryo's heart occurs from 3 to 8 weeks. More often, during this most important period of time for the unborn child, women sometimes do not always know about their pregnancy and lead their usual lifestyle, which, unfortunately, is not always healthy. If the expectant mother drank alcohol, smoked, had a viral infection, or took medications prohibited during pregnancy, there is a possibility that the child will develop tricuspid valve atresia.
Also at risk are women over 35 years of age who have an unfavorable obstetric history (pregnancy termination, stillbirth), suffering from diseases of the endocrine system, or having relatives with heart defects.
Classification
In modern cardiological practice, it is customary to distinguish four degrees of tricuspid valve prolapse:
I degree – characterized by the appearance of minor regurgitation, which does not disturb the general condition of the sick person’s body; II degree - the reverse flow of blood into the ventricle increases, and the force of the jet reaches 2 cm; III degree – severe regurgitation with disturbances in the functioning of the heart muscle (we wrote more about what regurgitation is here); IV degree - severe regurgitation, when about 40% of the total amount of blood enters the ventricle.
It is customary to distinguish primary and secondary forms of PTC. The primary variant of the disease occurs without manifestations of pulmonary artery hypertension, when the pathological process is formed against the background of primary deviations in the normal functioning of the cardiac organ. Secondary TB prolapse is a disease that occurs as a result of pulmonary hypertension and an increase in the size of the right chambers of the heart.
Symptoms
These include the so-called stigmas - signs of imperfection of the connective tissue framework: joint hypermobility, winged shoulder blades, myopia, Gothic (high) palate, malocclusion, flat feet, tall stature and asthenic physique, scoliosis, hernias, varicose veins. There is also a violation of the architectonics of the atrioventricular ring with displacement of the valves and additional chords in the valve apparatus.
Later, by the age of 7, additional symptoms appear: short-term stabbing pains in the heart area of a psycho-emotional nature, and not due to damage to the heart muscle, attacks of rapid heartbeat, interruptions.
Symptoms of vascular dystonia include dizziness, cephalgia in the morning, worsening after overwork, decreased performance and increased fatigue. Children are tearful, often have fears, depression, irritability, and poor sleep. In fact, this is a mass of microanomalies combined with vegetative-vascular instability.
A pediatrician or cardiologist listens to the murmur over the heart area and determines its nature - late systolic or in the form of a systolic click.
Unique operations performed by famous cardiac surgeons - only in Top Ikhilov
Among the main pathologies of the tricuspid valve are a narrowing of its diameter, or stenosis, insufficiency (the valves do not close tightly) and congenital defects (atresia - the ventricles are developed unequally, Ebstein's anomaly - displacement of the valves).
Treatment of tricuspid heart valve disease in Israel involves the use of medications and surgical intervention.
- Drug therapy . The Top Ichilov Medical Center uses modern drugs that are effective against pathology and safe for the body. In the treatment of tricuspid valve defects, angiotensin-converting enzyme (ACE) inhibitors, beta blockers, calcium channel blockers, glycosides, etc. are prescribed. The purpose of using medications is to lower blood pressure, improve blood circulation, reduce the frequency and strength of heart contractions, spasm of the coronary arteries and etc. Individual selection of drugs allows you to achieve maximum effect and reduce the development of side effects.
- Surgical intervention . Cardiac surgeons at Top Ikhilov in most cases prefer low-traumatic operations performed on the beating heart. Annuloplasty is an operation to strengthen the base of the valve and fix the valve flaps in the desired position by applying a ring or sutures. Thanks to annuloplasty, complete closure of the valves and normalization of blood circulation are achieved. When correcting the leaflets, the cardiac surgeon separates the fused leaflets, restores their shape, and stitches the tears. That is, defects in their structure are corrected. Valve replacement with an artificial prosthesis is performed using a transcatheter approach. Biological or mechanical implants (made of composite materials) are used, which are safe, hypoallergenic, and take root well. Percutaneous balloon valvuloplasty is used to increase the lumen of stenosis using a balloon, which is brought to the site of stenosis and inflated primarily with fluid to avoid embolism, thereby increasing the lumen of the valve. After achieving normal values, the liquid from the balloon is released and the balloon is removed along with the catheter.