Causes of plaques in the carotid arteries
The formation of cholesterol plaques in the carotid arteries is one of the forms of systemic atherosclerosis, rarely occurring in isolation.
As a rule, atherosclerosis of the brachiocephalic arteries (brachio - shoulder, cephalis - head (Greek)), which includes the carotid arteries, is combined with atherosclerosis of the aorta, coronary arteries, and arteries of the lower extremities. Atherosclerosis
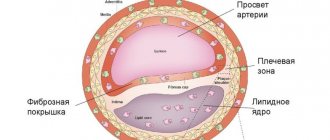
- a chronic disease of arteries of the elastic and muscular-elastic type, arising as a result of lipid metabolism disorders and accompanied by the deposition of cholesterol and some fractions of lipoproteins in the intima of blood vessels. Deposits form in the form of atheromatous plaques. The subsequent proliferation of connective tissue in them (sclerosis), and calcification of the vessel wall lead to deformation and narrowing of the lumen up to obliteration (blockage). It is impossible to name one single reason leading to atherosclerotic restructuring of the artery wall and the formation of atherosclerotic plaques.
Most researchers agree with the fact that atherosclerosis is based on a violation of fat metabolism (more precisely, cholesterol esters) at the level of genetic predisposition. Familial hypercholesterolemia (FH) is a known disease. This is a disease caused by a decrease in the rate of removal of low-density lipoprotein (LDL) from the bloodstream due to mutations in the specific LDL receptor gene. Familial hypercholesterolemia is the most common genetic disease due to a single gene mutation (monogenic disease). The modern medical scientific community, based on numerous studies, considers risk factors to be the main triggers for the progression of atherosclerosis (an increase in the size and number of plaques).
After operation
In the postoperative period, the patient is prescribed antiplatelet therapy - drugs that “thin” the blood. These drugs should be taken only as prescribed by a doctor with strict adherence to the dosage and regimen. Self-cancellation or replacement with other drugs without a doctor’s prescription is unacceptable.
Otherwise, the postoperative period after surgery on the carotid arteries does not differ significantly from any other operations: limiting physical activity, wound care.
In the vast majority of cases, the operation is quite comfortable and well tolerated by patients.
A timely operation saved the lives of many thousands of patients. Remember, there is nothing more expensive than your life and health.
Risk factors
- smoking (the most dangerous factor);
- hyperlipoproteinemia (total cholesterol > 5 mmol/l, LDL > 3 mmol/l, Lp(a) > 50 mg/dl);
- arterial hypertension (high blood pressure) (systolic blood pressure > 140 mm Hg; diastolic blood pressure > 90 mm Hg);
- diabetes;
- obesity;
- physical inactivity (sedentary lifestyle).
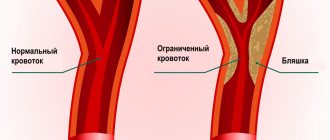
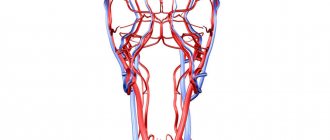
Without correction of risk factors, in the presence of a predisposition to atherosclerosis, cholesterol deposits gradually increase in the walls of the arteries. For clinical manifestations of atherosclerosis, a narrowing of any large artery by more than 50% is necessary. It is at this stage that patients most often seek medical help. Plaques in the carotid arteries are most often located in the cervical segment of the artery, over a short distance. The key point in determining the severity of damage to the internal carotid artery is the percentage of narrowing (stenosis) of its lumen, in relation to the normal lumen located behind the plaque. Numerous studies have proven that stenosis of the internal carotid artery by more than 70% increases the risk of ischemic stroke by 5 times, compared with a lesser degree of stenosis. The brain receives its main blood supply from two internal carotid and two vertebral arteries. Stenosis of the artery by more than 70% leads to a change in the local parameters of the blood flow - they can be compared with the flow of river water in places where the channel narrows - seething, turbulence, chaotic impacts of blood into the vessel wall lead to microthrombosis, trauma to the vessel wall, destruction of unstable plaques and its detachment particles. Particles of plaques and blood clots freely located in the bloodstream are called emboli. Following the bloodstream, the embolus gets stuck in smaller branches located in the brain, causing ischemia of areas of the brain and leading to its death.
Symptoms of atherosclerotic plaques in the carotid artery
The presence of atherosclerotic plaques in the vessels supplying the brain is often difficult to suspect, because complaints are varied and inconsistent. In addition, for clear symptoms to appear, there must be pronounced narrowing of the arteries. It is necessary to suspect the presence of atherosclerosis of the carotid arteries in the presence of risk factors, as well as diseases of the heart and blood vessels of the lower extremities. Currently, the main symptoms are considered to be the presence of small and large ischemic strokes, as well as general cerebral symptoms.
- Transient ischemic attacks (TIA)
occur when small fragments of an atherosclerotic plaque break off and enter small vessels of the brain, causing brain death in a small area. In this case, transient paralysis of the arms and/or legs (from several minutes to several hours), speech impairment, transient or sudden blindness in one eye, memory loss, dizziness, and fainting are possible. The presence of a TIA is a serious sign of a high risk of developing a severe stroke in the near future and requires immediate medical attention.
- Acute ischemic cerebrovascular accident (ACVA)
– a consequence of acute blockage of a large branch of the internal carotid artery, which led to the death of neurons and loss of some functions in the brain. In a third of all cases, a stroke leads to death. In most all cases, severe disability after a stroke forever changes the life of a person and his relatives.
- Chronic cerebrovascular insufficiency
– a decrease in blood flow to the brain due to narrowing of the arteries, forcing brain cells to be in constant tension of all intracellular systems and intercellular connections. Symptoms are non-specific, they can be noise in the head, dizziness, flashing “spots” before the eyes, unsteadiness when walking, etc.
Surgery to remove plaque from the internal carotid artery (eversion carotid endarterectomy)
Unfortunately, there are no drugs yet that can “dissolve” or eliminate plaques in blood vessels. Modern drugs can only stop the growth of atherosclerotic plaques and reduce the likelihood of blood clots. The main and only effective treatment for narrowing of the arteries is surgery. Numerous studies involving many countries have indisputably proven the effectiveness of preventive surgical methods in preventing stroke. It is important to understand that surgical intervention is performed if there are strict indications for surgery, and does not replace the treatment of systemic atherosclerosis.
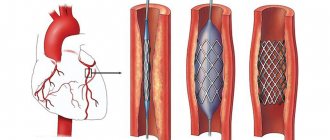
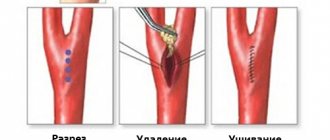
One of the ways to eliminate stenosis of the internal carotid artery is the operation of eversion carotid endarterectomy.
- Under the safest anesthesia (usually a local anesthetic), a small incision (4-6 cm) is made in the neck in the area of the carotid artery.
- Under threefold magnification, with the help of special instruments, the arteries are separated from the surrounding structures (nerves, veins).
- The resistance of the brain to temporary compression of the carotid artery is checked using several techniques. If there is the slightest suspicion that the brain will not be able to withstand clamping of the carotid artery, a special temporary shunt is installed to ensure blood supply to the area of the operated artery. The arteries are pinched.
- The internal carotid artery is dissected transversely and the outer layer of the artery is everted from the plaque like removing a stocking from a leg, after which the atherosclerotic plaque is removed from the vessel along with the inner layer.
- All plaque remnants freely lying in the lumen of the vessel are carefully removed and the outer layer of the artery is returned to its previous position.
- The integrity of the vessel is restored with a continuous suture. The threads used for sutures are thinner than 1/10 mm and are non-absorbable.
- Once the suture is completed, air is released from the artery and blood flow is restored. After checking the sutures for tightness and the absence of sources of bleeding, the wound is sutured layer-by-layer with a cosmetic suture.
Throughout the operation, the patient remains conscious, and verbal and eye contact is always maintained. The duration of the entire operation is 1-2 hours; in the postoperative period, long-term observation and treatment in the intensive care unit is not required. The perioperative protocol at our institution allows patients to be discharged the next day after surgery, which has a beneficial effect on early rehabilitation and prevents the occurrence of infectious complications.
Preparing for a non-surgical procedure
Before elective stenting, your endovascular surgeon will review your medical history and perform a physical examination. Can be assigned:
- Ultrasound . To obtain images using sound waves of the narrowed artery and the speed of blood flow to the brain.
- Contrast-enhanced computed tomography (MSCT) or Magnetic resonance angiography (MRA) . This diagnostic produces highly detailed images of blood vessels using radiofrequency waves in a magnetic field or X-rays injected with a radiopaque contrast agent.
Food and medicine
You will receive instructions about what you can eat or drink before your angioplasty and ICA stenting. Preparation may be different if you are already in the hospital before the intervention.
The night before your endovascular surgery:
- Follow your doctor's instructions about adjustments to your current medications. Your doctor may tell you to stop taking certain medications before having angioplasty, especially if you take certain diabetes medications or blood thinners.
- Arrange transportation home in advance. Angioplasty usually requires a hospital stay, and you may not be able to go home the next day due to the lingering effects of the sedation.
How to get an eversion carotid endarterectomy service (removal of carotid artery plaques)
Indications for surgical treatment of atherosclerosis of the internal carotid arteries are determined by a cardiovascular surgeon; however, to successfully perform the operation and minimize the risk of complications, coordinated interaction between a neurologist, cardiologist, and anesthesiologist is necessary. Our institution employs just such a team of professionals who are ready to help every patient in the fight against cardiovascular diseases. By making an appointment with a cardiovascular surgeon at the clinic, you will receive comprehensive information about the methods of modern diagnosis and treatment of diseases of the carotid arteries, determine the need and timing of surgical intervention. The modern technologies used and the experience of our specialists will help in getting rid of narrowing of the carotid arteries, preventing strokes and maintaining an active and fulfilling life.
Examinations before surgery
To select the surgical method (open or endovascular), the patient undergoes examination of the vessels of the head and neck - ultrasound.
In some cases, additional CT, MRI or angiography is required. In addition to examining the blood vessels before surgery, it is necessary to assess the state of health in general; for this, a number of standard examinations are prescribed, as for any other operation: clinical and biochemical blood tests, urine tests, tests for hepatitis, HIV, syphilis, etc., fluorography, ECHO CG (ultrasound of the heart), consultation with a therapist and/or cardiologist. The doctor must have a complete understanding of the patient’s health status, so additional examinations are prescribed if necessary.
One of the features of the examination before vascular surgery is the mandatory EGDS (examination of the stomach). The fact is that during and after the operation the patient is prescribed antithrombotic drugs that “thin” the blood; therefore, if the patient has a stomach ulcer, bleeding from the ulcer can occur. To diagnose an ulcer, an endoscopy is performed.
After a complete examination, the surgical method is selected depending on the characteristics of vascular damage, concomitant diseases and other factors.
Complications of carotid stenting
The most serious complication of carotid stenting is embolism (blockage) of blood vessels in the brain, which leads to stroke. Another complication that causes blockage of blood vessels is the formation of a blood clot along the stent. In addition, there is a complication such as restenosis - repeated blockage of the vessel. Another type of complication is associated with the toxic effect of the contrast agent on the kidneys, which is especially pronounced in patients with renal diseases. Less common is a hematoma or false aneurysm in the area where the catheter is inserted.
Tips for everyday life
During recovery, you may find it more difficult to do everyday activities. The tips below should help you.
- Maintain good posture: shoulders back and relaxed, head slightly tilted back. This will help relax your pectoral muscles and take pressure off your neck and shoulder muscles.
- If you feel weak on the side you had surgery on, rest your arm on a table or armrest while you sit. When you stand, rest the hand on your operated side on your hip or keep it in your pocket to relieve pressure from that hand on your shoulder. This will take the stress off the muscles and other parts of your neck and shoulder.
- When sleeping, lie on your back as much as possible. If you need to lie on your non-surgical side, you can place the arm on your surgical side on a pillow in front of you to avoid accidentally pulling your shoulder. Do not lie on your surgical side until your doctor or nurse tells you to do so.
- Do not lift or carry anything heavier than 3 pounds (1.4 kg) on your operated side until you no longer experience any pain. For comparison, an iron weighs approximately 3 pounds (1.4 kg), and a 1/2 gallon bottle of milk (approximately 2 liters) weighs 4 pounds (1.8 kg). Check with your doctor or nurse before lifting or carrying anything weighing more than 3 pounds (1.4 kg).
- Refrain from carrying a heavy briefcase on a belt or a bag on the side undergoing surgery. Check with your doctor or nurse before wearing a backpack or backpack.
to come back to the beginning
The cause of age-related changes in the vessels of the neck
Throughout life, the human body is affected by many negative factors. The environment, lifestyle, and foods consumed play an important role. With excessive consumption of foods high in cholesterol, atherosclerotic plaques form. As you age, they grow, causing partial blockage of the arteries, a condition called stenosis.
Another reason for age-related changes in the vessels of the neck is a decrease in the synthesis of collagen and elastin by the body. Vascular tissues become less elastic and more susceptible to negative influences.