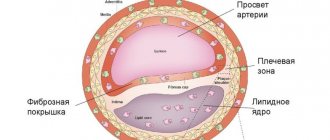
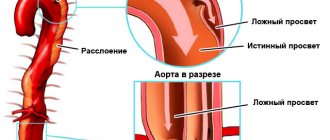
Carotid artery aneurysm is an extremely life-threatening condition for the patient. This is an expansion of a section of a blood vessel, accompanied by thinning and protrusion of its walls, which creates a risk of rupture of the formation. The presence of an aneurysm is a direct prerequisite for the occurrence of ischemic and hemorrhagic stroke.
Education can be:
- saccular - the wall of the vessel protrudes only on one side;
- fusiform - the wall of the vessel protrudes in both directions.
Reasons for appearance
The main reasons for the development of pathology are:
- congenital defects in the structure of the vascular wall;
- connective tissue weakness;
- traumatic injury (during surgery, road accident, fall from height, strong impact);
- chronically high blood pressure;
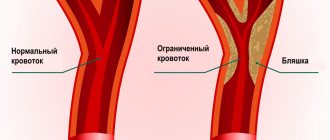
- atherosclerotic deposits on the walls of blood vessels;
- complications after removal of atherosclerotic plaques;
- infectious diseases.
There are also risk factors that significantly increase the likelihood of an aneurysm - smoking, alcohol abuse, obesity, and a sedentary lifestyle.
Types of SPA
The division is based on the causes that provoked the occurrence of vertebral artery syndrome. There are 4 main forms of spa:
- compression – is a consequence of mechanical compression of the arterial walls by surrounding structures;
- irritative - occurs due to spasm of the walls of blood vessels, which is a consequence of vertebral irritation of the nerve endings;
- angiospastic – also accompanied by vascular spasms, but due to stimulation of receptors located at the level of the affected segment of the cervical spine;
- mixed – characterized by the effect on the vertebral arteries of a combination of different factors.
But pathology rarely follows strictly one type. Mixed disorders are usually observed. Most often, compression-irritative and reflex-angiospastic forms are diagnosed.
In the first case, the disruption of blood flow is caused by mechanical compression of the artery itself and the nerve plexuses. In the second, the blood vessel spasms reflexively after irritation of the spinal nerves by intervertebral discs or due to other pathological processes in the spine.
Symptoms
The most common symptoms of a carotid aneurysm are neurological problems. All of them are caused by compression of the formations of various nerves. The main complaint of the vast majority of patients with carotid aneurysm is headache of varying intensity and localization. The following symptoms may also be present:
- double image in the horizontal plane, accompanied by a violation of the abduction of the eyeball outward;
- nystagmus;
- oculomotor disorders accompanied by a decrease in the pupil's reaction to light;
- loss of visual fields;
- paralysis of the facial nerve, accompanied by drooping of the lower eyelid, severe facial asymmetry;
- trigeminal neuralgia, characterized by periodic unilateral acute facial pain;
- bulbar syndrome;
- speech disorders;
- emotional lability, sudden mental deviations, clouding of consciousness.
Often the pathology is accompanied exclusively by a headache, as a result of which the patient postpones a visit to the doctor until the last minute. An aneurysm is often discovered completely by accident, during an examination for the presence of another disease.
The disease poses a direct threat to the patient's life. An aneurysm can rupture at any time, which leads to a coma - blood from the damaged vessel enters the subarachnoid space, mixing with the cerebrospinal fluid. 76% of such cases are fatal.
This is why it is so important not to delay treatment of an aneurysm. A timely operation reduces the patient's risk of death by up to 15%.
Category “Conversation with a specialist” Vertebral artery syndrome
This article was jointly prepared by neurologists of the Academy of Health LLC, Tatyana Valerievna Solovyova and Alexandra Vladimirovna Ananina.
Vertebral artery syndrome (VAS) is a complex of symptoms resulting from disruption of blood flow in the vertebral (or vertebral) arteries. In recent decades, this pathology has become quite widespread, which is probably due to the increase in the number of office workers and people leading a sedentary lifestyle who spend a lot of time at the computer. If previously the diagnosis of SPA was made mainly to elderly people, today the disease is diagnosed even in twenty-year-old patients. Since any disease is easier to prevent than to treat, it is important for everyone to know for what reasons vertebral artery syndrome occurs, what symptoms are manifested and how this pathology is diagnosed. We will talk about this, as well as the principles of SPA treatment, in our article.
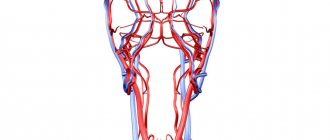
Basic anatomy and physiology Blood enters the brain through four large arteries: the left and right common carotid and the left and right vertebral. It is worth noting that 70-85% of the blood passes through the carotid arteries, so disruption of blood flow in them often leads to acute cerebrovascular accidents, that is, ischemic strokes.
The vertebral arteries supply the brain with only 15-30% of blood. Violation of blood flow in them, as a rule, does not cause acute, life-threatening problems - chronic disorders occur, which, however, significantly reduce the patient’s quality of life and even lead to disability.
The vertebral artery is a paired formation originating from the subclavian artery, which in turn arises on the left - from the aorta, and on the right - from the brachiocephalic trunk. The vertebral artery goes upward and slightly backward, passing behind the common carotid artery, enters the opening of the transverse process of the sixth cervical vertebra, rises vertically through similar openings of all overlying vertebrae, through the foramen magnum enters the cranial cavity and follows to the brain, supplying blood to the posterior parts of the brain : cerebellum, hypothalamus, corpus callosum, midbrain, partially temporal, parietal, occipital lobes, as well as the dura mater of the posterior cranial fossa. Before entering the cranial cavity, branches depart from the vertebral artery, carrying blood to the spinal cord and its membranes. Consequently, when blood flow in the vertebral artery is disrupted, symptoms arise that indicate hypoxia (oxygen starvation) of the areas of the brain that it supplies.
Causes and mechanisms of development of vertebral artery syndrome Along its length, the vertebral artery comes into contact with both the hard structures of the spinal column and the soft tissues surrounding it. Pathological changes that occur in these tissues are the prerequisites for the development of SPA. In addition, the cause may be congenital characteristics and acquired diseases of the arteries themselves.
So, there are 3 groups of causative factors of vertebral artery syndrome:
Congenital structural features of the artery: pathological tortuosity, course anomalies, kinks. Diseases that result in a decrease in the lumen of the artery: atherosclerosis, all kinds of arteritis (inflammation of the artery walls), thrombosis and embolism. Compression of the artery from the outside: osteochondrosis of the cervical spine, abnormalities of bone structure, trauma, scoliosis (these are vertebrogenic, that is, associated with the spine, causes), as well as tumors of the neck tissue, their scar changes, spasm of the neck muscles (these are non-vertebrogenic causes). Often, SPA occurs under the influence of several causative factors.
It is worth noting that RAS develops more often on the left, which is explained by the anatomical features of the left vertebral artery: it arises from the aortic arch, which often has atherosclerotic changes. The second leading cause, along with atherosclerosis, is degenerative diseases, that is, osteochondrosis. The bone canal in which the artery passes is quite narrow, and at the same time mobile. If there are osteophytes in the area of the transverse vertebrae, they compress the vessel, disrupting blood flow to the brain.
In the presence of one or more of the above reasons, factors predisposing to the deterioration of the patient’s well-being and the appearance of complaints are sudden turns or tilts of the head.
Symptoms of vertebral artery syndrome The pathological process in SPA goes through 2 stages: functional disorders, or dystonic, and organic (ischemic).
Stage of functional disorders (dystonic) The main symptom at this stage is headache: constant, intensifying during head movements or with prolonged forced positioning, burning, aching or pulsating in nature, covering the back of the head, temples and moving forward to the forehead.
Also at the dystonic stage, patients complain of dizziness of varying intensity: from a feeling of slight instability to a feeling of rapid rotation, tilting, and falling of one’s own body. In addition to dizziness, patients are often bothered by tinnitus and hearing impairment.
Various visual disturbances may also occur: sand, sparks, flashes, darkening of the eyes, and when examining the fundus, a decrease in the tone of its blood vessels.
If at the dystonic stage the causative factor is not eliminated for a long time, the disease progresses and the next, ischemic stage occurs.
Ischemic, or organic, stage At this stage, the patient is diagnosed with transient disorders of cerebral circulation: transient ischemic attacks. They are sudden attacks of severe dizziness, impaired coordination of movements, nausea and vomiting, and speech disorders. As mentioned above, these symptoms are often provoked by a sharp turn or tilt of the head. If, with such symptoms, the patient takes a horizontal position, there is a high probability of their regression (disappearance). After an attack, the patient feels tired, weak, tinnitus, sparks or flashes before the eyes, and headache.
Clinical variants of vertebral artery syndrome These are:
drop attacks (the patient suddenly falls, his head is thrown back, he cannot move or stand up during the attack; consciousness is not impaired; within a few minutes, motor function is restored; this condition occurs due to insufficient blood supply to the cerebellum and caudal parts of the brain stem); syncopal vertebral syndrome, or Unterharnsteidt syndrome (with a sharp turn or tilt of the head, as well as in the case of a prolonged stay in a forced position, the patient loses consciousness for a short time; the cause of this condition is ischemia of the region of the reticular formation of the brain); posterior cervical sympathetic syndrome, or Bare-Lieu syndrome (its main symptom is constant intense headaches of the “removing the helmet” type - localized in the occipital region and spreading to the front of the head; pain intensifies after sleeping on an uncomfortable pillow, when turning or tilting head; the nature of the pain is pulsating or shooting; may be accompanied by other symptoms characteristic of SPA); vestibulo-atactic syndrome (the main symptoms in this case are dizziness, a feeling of instability, imbalance, darkening of the eyes, nausea, vomiting, as well as disorders of the cardiovascular system (shortness of breath, pain in the heart, etc.); basilar migraine ( the attack is preceded by visual disturbances in both eyes, dizziness, unsteadiness of gait, tinnitus and blurred speech, after which intense headache occurs in the back of the head, vomiting, and then the patient loses consciousness); ophthalmic syndrome (complaints from the organ of vision come to the fore : pain, feeling of sand in the eyes, lacrimation, redness of the conjunctiva; the patient sees flashes and sparks before the eyes; visual acuity decreases, which is especially noticeable with eye strain; visual fields partially or completely disappear); cochleo-vestibular syndrome (the patient complains of decreased hearing acuity (perception of whispered speech is especially difficult), tinnitus, feeling of swaying, body instability or rotation of objects around the patient; the nature of the complaints changes - they directly depend on the position of the patient’s body); syndrome of autonomic disorders (the patient is concerned about the following symptoms: chills or a feeling of heat, sweating, constantly wet cold palms and feet, stabbing pain in the heart, headaches, and so on; often this syndrome does not occur on its own, but is combined with one or more others ); transient ischemic attacks, or TIA (the patient notes periodically occurring transient sensory or motor disturbances, disturbances in the organ of vision and/or speech, unsteadiness and dizziness, nausea, vomiting, double vision, difficulty swallowing). Diagnosis of vertebral artery syndrome Based on the patient’s complaints, the doctor will determine the presence of one or more of the above syndromes and, depending on this, will prescribe additional research methods:
X-ray of the cervical spine; magnetic resonance or computed tomography of the cervical spine; duplex scanning of the vertebral arteries; vertebral Dopplerography with functional loads (flexion/extension/rotation of the head). If the diagnosis of SPA is confirmed during further examination, the specialist will prescribe appropriate treatment.
Treatment of vertebral artery syndrome The effectiveness of treatment for this condition directly depends on the timeliness of its diagnosis: the earlier the diagnosis is made, the less thorny the path to recovery will be. Complex spa treatment should be carried out simultaneously in three directions:
therapy for pathology of the cervical spine; restoration of the lumen of the vertebral artery; additional treatment methods. First of all, the patient will be prescribed anti-inflammatory and decongestant drugs, namely non-steroidal anti-inflammatory drugs (meloxicam, nimesulide, celecoxib), angioprotectors (diosmin) and venotonics (troxerutin).
In order to improve blood flow through the vertebral artery, agapurine, vinpocetine, cinnarizine, nicergoline, instenon and other similar drugs are used.
To improve the metabolism (metabolism) of neurons, use citicoline, gliatilin, cerebrolysin, actovegin, mexidol and piracetam.
To improve metabolism not only in nerves, but also in other organs and tissues (vessels, muscles), the patient takes mildronate, trimetazidine or thiotriazoline.
In order to relax the spasmodic striated muscles, mydocalm or toldel will be used, vascular smooth muscles - drotaverine, better known to patients as No-shpa.
For migraine attacks, antimigraine drugs, such as sumatriptan, are used.
To improve the nutrition of nerve cells - B vitamins (Milgamma, Neurobion, Neurovitan and others).
To eliminate mechanical factors compressing the vertebral artery, the patient may be prescribed physical treatment (manual therapy, post-isometric muscle relaxation) or surgical intervention.
During the recovery period, neck massage, physical therapy, acupuncture, and sanatorium-resort treatment are widely used.
Prevention of vertebral artery syndrome The main preventive measures in this case are an active lifestyle and healthy sleep on comfortable bedding (it is highly desirable that they be classified as orthopedic). If your work involves keeping your head and neck in one position for a long time (for example, working at a computer or activities associated with continuous writing), it is strongly recommended to take breaks from it, during which you perform gymnastics for the cervical spine. If the complaints mentioned above appear, you should not wait for their progression: the right decision would be to consult a doctor as soon as possible.
You can make an appointment with a neurologist by calling: 8(3435)230-500
We care about you!
Always yours, Medical
Stages of the disease
The stage of development of an aneurysm is characterized by its size. Today in medicine the following classification of formations is used:
- milliary – with a diameter of up to 3 mm;
- regular size – diameter from 4 to 15 mm;
- large – with a diameter from 16 to 25 mm;
- gigantic - more than 25mm.
An aneurysm can also be single-chamber or multi-chamber.
SPA treatment at SL Clinic
At SL Clinic you will receive qualified advice. In the shortest possible time, we will be able to understand the reasons for the disturbance of your condition and the occurrence of painful migraines, determine the form of the spa, select the optimal treatment regimen and, if necessary, carry out the best surgical intervention.
If you contact us in the early stages of the disease, it is possible to transfer it to a state of stable remission. During it, you will no longer be bothered by the painful manifestations of SPA, and you will be able to lead an absolutely normal lifestyle.
But even in severe cases, doctors at SL Clinic will not leave you alone with the disease. We will do everything possible to achieve a significant improvement in your condition and overall quality of life. All operations with this diagnosis are performed in neurosurgical departments.
The cost of treatment of vertebral artery syndrome without surgery starts from 120,000 rubles and depends on: - procedures that will be included in the treatment; — Clinic and ward class (where the operation will be performed). The price includes: - Stay at the clinic; - Medications. — Blockades; — Traction treatment; — Physiotherapy. All clinic services and costs are listed in the price list.
SL Clinic specializes in performing various types of neurosurgical interventions and is ready to offer you European-level medicine in Moscow. We have the best modern equipment, and our neurosurgeons have extensive experience and master advanced techniques for treating spinal diseases. Therefore, our success rates for operations are consistently at extremely high positions.
Don’t hesitate, don’t wait until the SPA completely poisons your life and leads to the development of irreversible consequences, contact SL Clinic now. We will help you achieve the longest possible remission and get rid of the obsessive fear of the sudden onset of a new attack.
How is carotid aneurysm treated?
If the size of the aneurysm is not critical, the patient may be indicated for dynamic observation with examination every six months and taking antihypertensive medications. However, in practice this happens extremely rarely. When we are talking about a vital artery, and the aneurysm is localized in close proximity to the brain, it is better to be safe and prevent the problem than to deal with irreversible changes in the event of a sudden rupture of the formation.
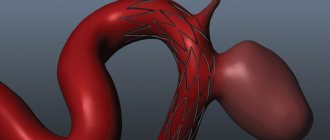
The main task of the doctor when treating an aneurysm is to exclude the damaged section of the artery from the blood circulation, maintaining normal blood flow. The most commonly used endovascular treatment method.
Cerebral aneurysm photo
I present to your attention a photo of 2 aneurysms - the main artery and the bifurcation of the middle cerebral artery, which we encountered in our clinic over the past 2 weeks.
Saccular aneurysm of the bifurcation of the basilar artery
Saccular aneurysm of the bifurcation of the left middle cerebral artery. The aneurysm and branches of M2 are outlined with a ballpoint pen.
The aneurysm of the bifurcation of the basilar artery had to be transferred to another health facility for endovascular exclusion (filling with coils), and the MCA aneurysm was operated on in our clinic.
Minimally invasive method
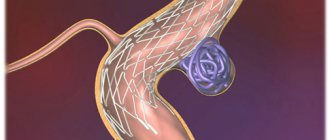
In the case of a saccular aneurysm and a small lumen of the anastomosis, embolization of the aneurysm is performed. The operation goes like this:
- a catheter is inserted through the inguinal vascular access under radiological control, which is passed to the aneurysm;
- upon reaching the goal, a microspiral is released from the tip of the catheter, which is transformed into a coil of randomly shaped wire and fills the aneurysm cavity;
- if one microspiral is not enough, several skeins may be needed;
- in the case of a wide lumen of the anastomosis, stenting of the vessel is performed in parallel with embolization of the aneurysm;
- the catheter is carefully removed, the patient is under the supervision of doctors in the hospital for 24 hours.
An aneurysm filled with a wire coil is switched off from the bloodstream, gradually overgrown with connective tissue. This eliminates the possibility of it breaking. However, this operation is not relevant in cases where the bulging walls of the vessels compress nearby nerves. Then the only treatment option is to remove the damaged section of the artery.
Diagnostics
Today, vertebral artery syndrome is diagnosed more often than it actually occurs. This is due to insufficient understanding of doctors about the specifics of its course. Therefore, the inflammatory process in the inner ear can be mistaken for SPA.
For the purpose of correct diagnosis, doctors at SL Clinic prescribe a set of tests to patients and at the same time carry out long-term monitoring of the peculiarities of the course of SPA. The nature of the existing complaints, a thorough survey and examination of the patient allow our specialists to clearly identify the set of signs and determine how much they correspond to the above 9 clinical forms of SPA.
During the examination, the doctor will definitely find out the degree of pain in the scalp, since often the slightest touch to it provokes a pronounced increase in pain. Muscle tension and the presence or absence of discomfort when pressing on certain points on the back of the neck are also determined.
To detect vascular diseases, spinal pathologies and other disorders, the following must be carried out:
- radiography of the spine;
- MRI of the cervical spine;
- Ultrasound scanning of neck vessels;
- stabilometry;
- otoneurological examination;
- UAC;
- blood chemistry.
During dynamic observation, new data are discovered that help adjust the initially prescribed treatment and increase its effectiveness. This approach to spa therapy ensures its maximum effectiveness, reducing the risk of complications and reducing the frequency of attacks.
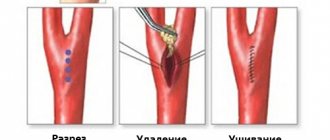
Surgery
In cases of an aneurysm that threatens the patient's life, open intervention is performed - microsurgical clipping. The operation is carried out as follows:
- a hole is cut in the patient's skull;
- a special metal clip is inserted through it, pinching the wall of the damaged vessel.
This technique cannot be called perfect. It is prescribed only in extreme cases when other methods of treating an aneurysm are impossible. Life after clipping has a lot of restrictions; the patient is assigned a disability group. The operation does not guarantee that the aneurysm will not form again
All possible risks and outcomes of the disease must be discussed with the patient. The intervention is carried out by consent. In the event of a rupture of an aneurysm, the patient will undergo emergency surgery with the consent of the next of kin.
Another treatment option is surgical removal of the bulging portion of the vessel wall and its replacement with a polyester or nylon prosthesis. During the operation, the patient is connected to a heart-lung machine. The aneurysmal sac is opened, the thrombus and part of the expanded wall are removed, and a prosthesis is installed in their place. The remaining part of the vessel wall is sewn to the prosthesis.
This technique has a number of contraindications. It is not performed on elderly patients and patients with serious concomitant diseases.
Treatment methods for cerebral aneurysm
Surgical
Aneurysm can only be treated surgically - by direct intervention, disconnection by clipping, wrapping with various materials (rarely) or by the endovascular method. Only milliary aneurysms can be observed in patients without risk factors for rupture. Aneurysms without previous hemorrhages are also subject to surgical treatment. It is easier to prevent a rupture than to treat its fatal consequences - vasospasm and clipping the aneurysm in the acute period.
Intraoperative photo of a clipped left middle cerebral artery aneurysm.
CT angiography the next day after surgery. Aneurysm is turned off. The M2 segments of the left MCA are contrasted.
The red circle marks the intervention area where 2 clips are installed. There are signs of vasospasm.
In the area of surgery on a native CT scan of the brain along the Sylvian fissure there is a small amount of blood - impregnated surgicell.
On a CT scan in bone mode, the clip is clearly visible.
Prevention
The operation does not eliminate the need to regularly visit a specialist. It is necessary to dynamically monitor the condition of the vessels, because expansion of the prosthesis, displacement or weakening of the stent may occur. There are also situations when a stented aneurysm begins to increase in size and bleed. Therefore, patients undergoing surgery for this pathology must visit a doctor every six months and undergo a comprehensive examination. This is the main recommendation that will help to significantly prolong life and improve its quality.
There are no specific measures to prevent carotid aneurysm. However, doctors give general recommendations:
- complete cessation of bad habits - smoking, drinking alcohol, drugs;
- control of blood pressure, cholesterol and blood sugar;
- minimizing the impact of stress factors;
- avoiding physical stress;
- moderate activity - regular walking, swimming, exercise therapy;
- regular comprehensive neurological examinations for patients whose close relatives suffer from carotid aneurysm.
If you suspect you have an aneurysm, contact an experienced professional immediately. Do not self-medicate, and certainly do not be afraid of intervention. Modern medicine has sufficient capabilities to save the lives of patients even in difficult situations.
Still have questions about carotid aneurysm?
Free consultation with AngioClinic specialists
Author
Salmina Daria Vladimirovna
Geneticist. Graduated from the Chelyabinsk State Medical Academy. She completed an internship at the Northwestern State Medical University named after I.I. Mechnikov.
A comment
The article presents a case of successful two-stage surgical treatment of a giant partially thrombosed vertebral artery aneurysm with the staged use of endovascular and microsurgical methods. Surgical treatment of patients with giant partially thrombosed aneurysms is still a difficult problem in modern vascular neurosurgery. This article is important and relevant for vascular neurosurgeons, since it presents the features of the clinical picture and neuroimaging picture, and treatment tactics using a clinical example. Literature data concerning the problems of genesis and surgical treatment of giant partially thrombosed cerebral aneurysms are also widely presented. The work is a striking example of the high effectiveness of the combination of two main neurosurgical methods for the treatment of intracranial aneurysms; it attracts by the logic of the chosen tactics, good illustrations and completeness of discussion of the problem with analysis of literature data. The issues of the mechanism of aneurysm growth are raised with a discussion of the importance of the hemodynamic factor and the role of vasa vasorum
in the blood supply to nearby brain structures.
In our opinion, clipping the stump of the vertebral artery before intersection is less dangerous than coagulating its trunk over a long distance. As for the timing of the second stage of surgical treatment, if at least a slight blood flow in the cervical part is maintained and taking into account the severity of vasa vasorum
, it is advisable to reduce them.
The ideal method of treating such aneurysms is microsurgical exclusion of the aneurysm from the bloodstream with the removal of thrombotic masses to eliminate compression of the surrounding brain structures. However, this task is often difficult and sometimes impossible, since most of these aneurysms have dense, atherosclerotic and calcified walls. Often, during the growth of an aneurysm, the inclusion of the carrier artery or its perforating branches into the wall of the body or neck of the aneurysm occurs, which was the case in the above observation. The above factors, especially with vertebrobasilar localization of aneurysms, often make them inoperable. The introduction of modern endovascular techniques has led to the expansion of indications for surgical treatment of large aneurysms and to improved outcomes of interventions. However, the use of the latter does not completely solve the problem of treating “complex” cerebral aneurysms. In these conditions, vascular neurosurgeons resort to various combinations of two methods for treating cerebral aneurysms, as shown in this work. In our opinion, microsurgical revascularization operations are promising in the surgery of such aneurysms.
A.S. Kheireddin (Moscow)