A popliteal artery aneurysm is a pathological expansion of the main artery running from the lower third of the thigh to the upper third of the leg. It is located quite deep in the leg under the knee. The popliteal artery is a continuation of the superficial femoral artery and below the knee it divides into the anterior, posterior tibial arteries and peroneal artery. These arteries supply blood to the leg and foot, so blocking blood flow in the popliteal artery leads to severe circulatory failure in the leg below the knee. The normal diameter of the vessel is about 6-10 mm.
Popliteal aneurysm is a risk factor for sudden acute limb ischemia and subsequent amputation. Unoperated aneurysms lead to leg amputation in 50% of all cases within 3 years.
Popliteal artery aneurysm must be operated on as soon as possible after diagnosis. There is no need to hope that it will “resolve” on its own. The high risk of acute ischemia and good results of planned operations should encourage the patient to consent to surgery. The results of planned interventions are very good.
Treatment technologies at the Innovative Vascular Center
The vascular surgeons of our clinic have significant experience in diagnosing and treating both planned and complicated lesions of the popliteal artery. The main method of treatment in our clinic is autovenous replacement of the popliteal aneurysm. This technology shows better immediate and long-term results. For complicated aneurysms, open surgery allows you to restore the patency of not only the popliteal artery, but also the vessels of the leg. Endovascular interventions for extensions of this localization have very poor results due to the high mobility of the knee joint.
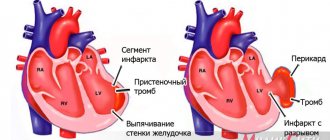
Symptoms of cardiac aneurysms
The cause of the development of cardiac aneurysms is most often the thinning of the muscle wall due to a heart attack. Having a heart attack weakens the tissue, which often causes the damaged area to bulge. The left ventricle of the heart and the interventricular septum are most susceptible to such pathologies. Symptoms in this case can manifest themselves in the form of pressing pain in the heart area, tingling sensations, and shortness of breath. Heart rhythm disturbances and signs of chronic coronary insufficiency may also be observed. Rupture of an acute aneurysm most often leads to death. In this case, the patient experiences severe pallor, loss of consciousness, coldness of the extremities and hoarse breathing. You can learn about treatment methods for cardiac aneurysms here.
Causes
Popliteal artery aneurysms account for about 1% of all surgical vascular diseases and often occur in both legs. The main reason is the congenital weakness of the artery wall, which contributes to their pathological expansion. The majority of patients (95%) are elderly men with an average age of approximately 71 years. The exact reasons for the development of dilation in the popliteal artery are unknown, but there is a clear connection with atherosclerotic changes in the vessel wall. Sometimes the pathology develops as a result of injuries to the popliteal region, dislocations or fractures. Patients with multiple aneurysms in different arteries should have general tissue weakness. The exact nature of this is still unclear. The tendency of the popliteal artery to pathological expansion is associated with frequent flexion and extension of the vessel due to movements in the knee joint.
Experience in surgical treatment of false aneurysm of the deep femoral artery (clinical case)
A.V. MAKSIMOV, E.A. GAISINA, A.K. FEISKHANOV, V.V. GLINKIN
Republican Clinical Hospital of the Ministry of Health of the Republic of Tatarstan, Kazan
Kazan State Medical Academy
Maksimov Alexander Vladimirovich
— Candidate of Medical Sciences, Head of the Department of Vascular Surgery, Associate Professor of the Department of Cardiology, Endovascular and Cardiovascular Surgery
420064, Kazan, Orenburgsky tract, no. 138, tel. 2-686-987, e-mail
False aneurysms of the great arteries in the structure of reconstructive operations on the great vessels range from 0.5% to
8-9%.
Their surgical treatment with the modern development of vascular surgery has been developed quite well. Therefore, the observation of large aneurysms in these localizations today is casuistry. The article presents a clinical case of successful surgical treatment of a giant false aneurysm of the femoral artery. Key words: giant false aneurysm, deep femoral artery replacement.
AV MAKSIMOV, EA GAYSINA, A K. PHEYSKHANOV, VV GLINKIN
Republican Clinical Hospital of the Ministry of Health of the Republic of Tatarstan, Kazan
Kazan State Medical Academy
Experience of surgical treatment of pseudoaneurysm of the deep femoral artery (medical case)
Pseudoaneurysm of the magistral arteries within corrective surgery on great vessels is from 0.5% to 9.8%. Their operative treatment in course of the current development of vascular surgery is worked out good enough. Therefore, the observation of large aneurysms of these locations today is casuistry. The article presents a medical case of successful surgical treatment of a giant pseudoaneurysm of femoral artery.
Key words:
giant pseudoaneurysm, prosthesis of the deep femoral artery.
False aneurysms of the great arteries account for from 0.5% to 8-9% in the structure of reconstructive operations on the great vessels [1, 2]. The most well-known causes of their occurrence are catheterization of the femoral artery during diagnostic and therapeutic procedures, trauma to the vessel, failure of the vascular anastomosis, or arrosive bleeding due to a purulent-inflammatory process.
Diagnosis of aneurysms of superficial arteries (femoral, brachial, carotid) is not difficult. Their surgical treatment with the modern development of vascular surgery has been developed quite well. Therefore, observations of large aneurysms in these localizations today are casuistry. In this regard, we present a clinical case of successful surgical treatment of a giant false aneurysm of the femoral artery.
Patient Z., 69 years old, was admitted to the department of vascular surgery of the Republican Clinical Hospital of the Ministry of Health of the Republic of Tatarstan with complaints of the presence of a painful dense formation in the left groin area and the upper third of the thigh. According to the patient, in 1988 (24 years ago) reconstructive surgery was performed on the left femoral artery. After discharge, he notes a slow growth of formation in the area of the postoperative wound. The patient did not seek medical help regarding this matter. The reason for this patient's visit was the appearance of pain.
Laboratory data on admission: Hb - 127 g/l, Er - 3.09 x 1012/l, L - 6.7 x 109/l, total protein - 64 g/l; creatinine - 64 umol/l; potassium - 0.6 mmol/l; sodium -137 mmol/l, AST - 26 U/l, ALT - 2-2 U/l, PTI - 73%; APTT - 32.5 s.
On examination: the left lower limb is pale, cool on palpation, the veins are empty. In the groin area, along the anterior surface of the thigh, in the projection of the femoral artery, a dense, painful, weakly pulsating formation with a diameter of 18 cm, rising above the skin by 20 cm, is determined. The skin above the formation is thinned, tense, with areas of cyanosis and developing necrosis. Tactile sensitivity and active movements in the limb are preserved. There is no pulsation in the popliteal artery on both sides (Fig. 1).
Rice. 1.
Giant aneurysm of the left femoral artery
Distal arteriography and CT angiography were performed (Fig. 2), and the diagnosis was made: Atherosclerosis. Obliterating atherosclerosis of the arteries of the lower extremities.
Rice. 2.
Arteriography and CT angiography of patient Z
Occlusion of the superficial femoral artery on both sides. Condition after reconstructive surgery on the left femoral artery (1988). Giant false aneurysm of the left femoral artery. Chronic arterial insufficiency of both lower extremities, degree 2B (according to Pokrovsky A.V.). IHD. (PEAKS?). Hypertension of the 1st degree. Common psoriasis, acute stage.
On December 18, 2012, an operation was performed: resection of a giant false aneurysm of the femoral artery on the left. External-iliac-deep-femoral extra-anatomical prosthetics on the left.
Progress of the operation: under epidural anesthesia, from the retroperitoneal approach according to Pirogov, the external iliac artery was isolated on the left and clamped. A longitudinal incision was made to open a false aneurysm in the groin area. The aneurysm cavity is filled with parietal thrombotic masses and tissue detritus from muscles and surrounding tissues with a volume of up to 2-2.5 liters. At the bottom of the aneurysm, the orifice of the deep femoral artery is visualized. The femoral artery, as an anatomical structure, is absent. From a separate access, lateral to the opened cavity of the aneurysm, the unchanged distal segment of the deep femoral artery was isolated. Extra-anatomical ilio-deep femoral prosthesis was performed using an Intergard-Silver 8 mm prosthesis, which was placed extra-anatomically outside the aneurysm cavity through the lacuna musculorum. Thrombotic masses and tissue detritus from the aneurysm cavity were removed, altered tissue of the aneurysm bottom and excess fasciocutaneous flap were excised. The aneurysm cavity was actively drained and sutured in layers. Blood loss was 250 ml.
In the postoperative period - the formation of marginal necrosis of the wound. Healing by secondary intention. Blood flow in the lower limb is compensated. The ankle-brachial index at discharge was 0.7. Discharged with recovery.
LITERATURE
1. Webber GW, Jang J., Gustavson S., Olin JW Contemporary management of postcatheterization pseudoaneurysms // Circulation. - 2007. - Vol. 115. - P. 2666-2674.
2. Righini M. Post-catheterization false femoral aneurysms // Rev. Med. Suisse. - 2007. - Vol. 3 (97). - P. 341-345.; Tisi PV, Callam MJ Treatment for femoral pseudoaneurysms // Cochrane Database Syst. Rev. - 2009; (2): CD004981.
Complaints and symptoms
Patients with an aneurysm complain of a feeling of heaviness in the popliteal region, swelling of the foot of the affected limb, and sometimes shooting pains. Most often, such complaints are vague, and the patient may not be aware that he has such a dangerous disease.
With aneurysm thrombosis, a clinical picture of acute ischemia develops: severe pain in the affected limb, changes in color and skin temperature of the foot. Subsequently, disturbances in sensitivity and movement develop. With advanced acute ischemia, rigor of the leg and foot develops; active and passive movements are impossible due to muscle death.
Symptoms of cerebral aneurysms
The danger of aneurysms of blood vessels supplying the brain is a high risk of cerebral hemorrhage. The development of aneurysms is facilitated by atherosclerosis of the brachiocephalic arteries, head injuries, the presence of tumors, and high blood pressure. With this disease, patients may experience:
- attacks of headaches;
- blurred vision, double or flickering vision;
- dizziness;
- hearing impairment;
- feeling of dumbness in one side of the face and body.
A ruptured brain aneurysm may be indicated by severe headache, severe vomiting, and loss of consciousness.
Course and complications
The main risk from a popliteal aneurysm is associated with embolization - blockage of the underlying arteries with pieces of blood clots or occlusion of the aneurysm cavity. Both of these complications can lead to acute ischemia and gangrene of the legs (sudden loss of blood supply). Blood clots (thrombi) gradually form in the cavity of the vessel. When this clot remains attached to the wall of the vessel, it does not pose any danger. If a clot fragment breaks off, it can travel far from the aneurysm and cause blockages in small arteries, preventing blood flow to downstream tissues. A popliteal aneurysm can rupture (rupture), but this is much less common than embolization. In this case, a pulsating hematoma occurs behind the knee. Simultaneously with the rupture, the next stage is thrombosis of the popliteal artery with the development of signs of acute circulatory failure of the limb. Most people develop severe ischemic changes and death of the leg. Only surgery performed within the next 6-12 hours after the complication will help avoid amputation.
Features of symptoms of aneurysms
Aneurysms that arise in the vessels of the circulatory system can differ in shape, size and growth rate, as well as in localization in a particular vascular basin. Quite often, the symptoms of an aneurysm do not appear at all, remaining unnoticed until rupture. An asymptomatic disease can be detected by chance during examination of blood vessels.
In some cases, patients may exhibit signs of aneurysms, which depend mainly on where in the cardiovascular system the pathology occurs. Aneurysms form in the arteries of the brain, the aorta and peripheral vessels, as well as on weakened walls of the chambers of the heart.
Symptoms of aortic aneurysms
Aneurysms form in all parts of the aorta, sometimes in several sections at once. Aortic aneurysm occurs as a result of injuries to the abdomen and chest cavity, infectious diseases, as well as atherosclerotic lesions. Symptoms depend on the part of the artery where it formed: aneurysms of the ascending aorta, as well as the abdominal or thoracic sections, manifest themselves in different ways, because the aorta is a large vessel passing from the heart through the abdominal cavity. As a rule, aneurysms of the abdominal aorta make themselves felt in the form of pain in the abdomen, back, and pulsating sensations in the navel. When an aneurysm ruptures, the pain becomes very severe and may be accompanied by loss of consciousness and watering. Read more about the symptoms of an abdominal aortic aneurysm in the following publication.
Similar symptoms can be observed with aneurysmal formations in the thoracic aorta. Typically, with thoracic aortic aneurysms, patients complain of pain in the chest, back or abdomen. A rupture may be indicated by sharp pain, low blood pressure, weakness and fainting, numbness of half the body and speech disturbances.
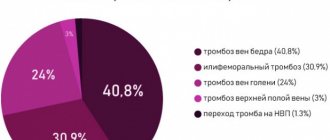
Clinical forms of deep vein thrombosis
Vein thrombosis of the leg
Complaints of swelling of the foot, pain and tension in the calves, pain when pressing on the calf muscles. If thrombosis does not spread, it is almost asymptomatic. Sometimes there is thromboembolism of small branches of the pulmonary artery with cough and the development of pneumonia (pneumonia). Treatment of thrombosis of the veins of the leg can be carried out on an outpatient basis, under the supervision of a phlebologist with control ultrasound examinations.
Thrombosis of the popliteal vein
Has a clear clinical picture. Severe swelling and tension of the lower leg, swollen saphenous veins, severe pain when walking. Thrombosis of the popliteal vein is very dangerous due to frequent pulmonary embolism, so treatment is best carried out in a vascular hospital. Most often, conservative therapy is carried out with antithrombotic drugs (heparin). If the patient had thromboembolism, then urgent surgical treatment is necessary - ligation of the femoral vein above the thrombus.
Thrombosis of the iliofemoral segment (ileofemoral phlebothrombosis)
It is characterized by a severe general condition, pronounced swelling of the entire lower limb, and severe pain. The saphenous veins are sharply dilated, the leg takes on a bluish color. With ascending deep venous thrombosis, thrombosis of the entire venous bed is possible with a block of venous outflow and the development of venous gangrene (blue phlegmasia), which is accompanied by high mortality. Pulmonary embolism often occurs with a fatal outcome. Treatment of ileofemoral phlebothrombosis is only in a hospital. For occlusive thrombosis, conservative treatment is possible, but it is better to remove the thrombus so that post-thrombotic disease does not develop. In case of floating thrombosis, urgent removal of the thrombus (thrombectomy) is necessary, possibly using innovative methods. A vena cava filter can be installed in cancer patients.
Thrombosis of the inferior vena cava
The most dangerous disease. Clinically, it manifests itself as a severe general condition, swelling of both legs. Kidney failure and blood in the urine often develop. With thrombosis of the hepatic segment, liver failure develops resulting in Bud-Chiari syndrome. Treatment of acute thrombosis of the inferior vena cava should be active. It is necessary to remove thrombotic masses, as surviving patients may develop severe inferior vena cava syndrome. For this, it is good to use our innovative methods and systemic thrombolysis. The effectiveness of this treatment is very high.
Sources
- S. Z. Amrakhov, A. S. Vischipanov. Surgical tactics and principles of performing operations in patients with coronary heart disease with post-infarction aneurysm of the left ventricle of posterobasal localization. Bulletin of the Scientific Center for Agricultural Sciences named after. A.N. Bakulev RAMS. 2013; 14 (1): 26-33.
- Koon K. Teo, MBBCh, PhD. Aneurysms of peripheral arteries. // MSD Disease Directory - 2021.
- Mark A. Farber, MD; Thaniyyah S. Ahmad, MD. Aneurysms of the thoracic aorta. // MSD Disease Directory - 2021.
- Brain aneurysms - Research Institute of Emergency Medicine named after. N.V. Sklifosovsky.
Causes and prevention of varicose veins of the lower extremities
The causes of varicose veins in most cases lie in a sedentary lifestyle: we spend a long time in a static position (especially sitting), and do not give the necessary stress to our muscles. The following risk factors may also affect:
- excessively tight clothing (pants, socks),
- uncomfortable shoes (especially high heels),
- disturbances in hormonal balance,
- frequent hot baths, sauna visits,
- prolonged serious physical activity, heavy lifting,
- obesity.
The main prevention of varicose veins is maintaining a healthy lifestyle. Even if you have a sedentary job, try not to sit without moving for several hours in a row: get up, stretch your legs, walk more; and don’t forget about a balanced diet, which, along with moderate physical activity, will protect you from many diseases.
Pregnancy is also one of the serious risk factors for varicose veins. But genetic predisposition is still being studied, and there are even a number of studies that refute it.