A pathological disturbance of the blood supply to the heart muscle, accompanied by attacks of chest pain, intensifying after stress and physical exertion, shortness of breath, dizziness, and weakness. Coronary heart disease (CHD) is the most common cause of death in developed countries. Russia is no exception here. The cause of IHD is coronary atherosclerosis, that is, partial or complete blockage of one or more coronary arteries (arteries that supply blood to the heart itself) with atherosclerotic plaques. However, IHD and coronary atherosclerosis are not synonymous. In order to make a diagnosis of coronary artery disease, it is necessary to prove the presence of myocardial ischemia using functional diagnostic methods.
Often the diagnosis of IHD is made unreasonably, especially in old age. IHD and old age are also not synonymous.
There are several forms of IHD. The most common of them will be discussed below - angina pectoris, unstable angina, myocardial infarction. Other forms of IHD include ischemic cardiomyopathy, silent myocardial ischemia, microcirculatory angina (cardiac syndrome X).
Symptoms
The main manifestation of myocardial ischemia is chest pain. The severity of pain can vary - from mild discomfort, a feeling of pressure, burning in the chest to severe pain during myocardial infarction. Pain or discomfort most often occurs behind the sternum, in the middle of the chest, or inside it. The pain often radiates to the left arm, under the shoulder blade or down to the solar plexus area. The lower jaw and shoulder may hurt. In a typical case, an angina attack is caused by physical (less often emotional) stress, cold, heavy food - everything that causes an increase in the work of the heart. Pain is a manifestation of the fact that the heart muscle lacks oxygen: the blood flow provided by the narrowed coronary artery becomes insufficient under load.
In typical cases, the attack is eliminated (stopped) with rest on its own or after taking nitroglycerin (or other fast-acting nitrates - in the form of sublingual tablets or spray). It must be borne in mind that nitroglycerin can cause headaches and a decrease in blood pressure - these are direct manifestations of its action. You should not take more than two nitroglycerin tablets on your own: this is fraught with complications.
There may be no complaints (this is the so-called silent myocardial ischemia), sometimes the first manifestation of IHD is myocardial infarction or sudden death. In this regard, everyone who has risk factors for atherosclerosis and who is going to engage in physical exercise needs to undergo a stress test (see below) to make sure that myocardial ischemia does not occur during exercise.
Interruptions in the work of the heart (extrasystoles) in themselves are not a sign of coronary artery disease. The cause of extrasystoles most often remains unclear, and extrasystole itself does not require treatment. Nevertheless, in patients with coronary artery disease, extrasystole often occurs during physical activity: if you conduct a stress test and make sure that the extrasystole disappears during exercise, this indicates its benign nature, that it is not life-threatening.
Complaints with ischemic cardiomyopathy are characteristic of heart failure of any other origin. First of all, it is shortness of breath, that is, a feeling of lack of air during exertion, and in severe cases, at rest.
Complications of CVD
According to WHO, cardiovascular pathologies are the main cause of death and often lead to disability. Death is not uncommon with large heart attacks and strokes, massive pulmonary embolism, heart failure complicated by pulmonary edema, and cardiogenic shock. A stroke can lead to a wide range of neurological disorders, and chronic cerebrovascular accident can lead to progressive cognitive impairment. Peripheral arterial pathologies are dangerous due to the development of gangrene with subsequent amputation of the limb (often at a young age). CVDs have a detrimental effect on the state of the reproductive sphere: impotence is often registered in men, and infertility and childlessness in women.
Angina pectoris
Angina pectoris is otherwise called stable angina. Angina is considered stable if its severity remains constant for several weeks. The severity of stable angina may vary somewhat depending on the patient's activity level and ambient temperature.
New-onset angina is called angina that occurred a few weeks ago. This is a borderline state between stable and unstable angina.
The severity of angina pectoris is characterized by its functional class: from the first (mildest), when attacks occur only during heavy physical work, to the fourth, most severe (attacks with little physical activity and even at rest).
Intestinal ischemia
Intestinal ischemia refers to a whole group of diseases that are caused by both chronic and acute processes. But all pathologies are united by a common factor. This is a decrease in blood flow to the gastrointestinal tract and directly to the intestines.
Mesentral embolic ischemia poses a great danger. It comes suddenly. It is characterized by a “sharp belly.” Without the use of comprehensive diagnostic tools, symptoms can be confused with symptoms of acute pancreatitis, appendicitis, or perforated ulcers. But the nature of this pathology is different - a sudden formation of obstruction (occlusion) in the mesenteric vessel - tissue that is involved in attaching the intestine itself to the abdominal wall. This may be a response to infection, injury, blood diseases, portal hypertension - increased pressure in the portal vein, taking certain medications (for example, contraceptives). If the pathology is not promptly diagnosed and measures are not taken, the intestinal walls may begin to necrosis (die).
Another type of pathology is ischemia following mesentral thrombosis (thrombosis of mesenteric vessels). It is characterized by intense, cramping pain. At the initial examination, the symptoms are similar to intestinal colic and intestinal obstruction. But again, the further prognosis depends on the speed of diagnosis. As a rule, the problem is solved by diagnosis and resection. If they are not done on time, death is likely in 70-90% of cases.
But the most common option is colonic ischemia, which develops against the background of vascular atherosclerosis, aortic dissection or the presence of an aneurysm. The disease is accompanied by severe exhaustion. 80% experience weight loss.
Diagnostics
An electrocardiogram (or echocardiography) at rest is NOT a method for diagnosing coronary artery disease. Sometimes these methods, however, make it possible to diagnose or detect coronary artery disease, for example, if signs of a previous myocardial infarction can be detected, or if they are performed against the background of chest pain.
Holter monitoring (ECG monitoring) also does not serve as a method for diagnosing coronary artery disease, although this method is used unreasonably widely for this purpose. ST segment depressions that are detected by Holter ECG monitoring are often nonspecific (i.e., false), especially in women. Holter monitoring only allows you to identify
The main method for diagnosing ischemic heart disease is stress testing.
. The main types of stress tests are: ECG tests with exercise and stress echocardiography, that is, echocardiography performed during exercise (or immediately after its completion) or against the background of the administration of drugs that increase heart function (for example, dobutamine). Myocardial scintigraphy (isotope study of the heart under stress) in Russia is performed in only a few centers and is practically inaccessible.
Based on the results of stress tests, a decision is made whether to refer the patient for coronary angiography. It is almost never necessary to begin the examination with coronary angiography. This is the best method to visualize (examine) lesions of the coronary arteries (atherosclerotic plaques), but coronary angiography often cannot assess their functional significance (whether they cause myocardial ischemia or not).
Establishing diagnosis
The effectiveness of therapy and a favorable prognosis largely depend on the timely diagnosis of coronary heart disease. The sooner the nature of the disease is determined and treatment is started, the higher the chances of restoring health. Despite the fact that the symptoms of IHD are recognized quite well, the doctor needs instrumental confirmation and objective research data:
- electrocardiogram;
- ECG with stress;
- monitoring of cardiac activity during the day using Holter;
- EchoCG;
- ultrasonography;
- Dopplerography and angiography of cardiac vessels;
- computed tomography or magnetic resonance imaging;
- bicycle ergometry.
In addition, the doctor orders laboratory tests. In addition to general blood and urine tests, it may be necessary to study some enzymes, the level of which increases in unstable and pre-infarction conditions. In addition, biochemical analysis determines the level of total cholesterol, HDL and LDL, sugar content, triglyceride levels and nonspecific markers of cytolysis.
Treatment
There are three main treatment options for exertional angina: medication, coronary stenting (angioplasty with stent placement) and coronary artery bypass grafting. In any case, treatment begins with active intervention on risk factors: a low-cholesterol diet, quitting smoking, normalizing blood pressure, etc.
Each patient diagnosed with coronary artery disease should, in the absence of contraindications, take at least three drugs: a beta-blocker (for example, metoprolol, bisoprolol, nadolol), an antiplatelet agent (most often aspirin) and a statin (for example, atorvastatin, rosuvastatin).
It must be borne in mind that neither coronary stenting nor coronary bypass surgery in general prolongs life. There are only select groups of patients for whom this is not true. Thus, bypass surgery prolongs life in patients with damage to several vessels in combination with diabetes mellitus, with severely reduced overall contractile function of the heart, and with damage to the proximal (initial) parts of the left coronary artery.
Stenting for stable angina also has a limited set of vital indications, and generally serves to improve the quality of life (that is, eliminate symptoms), rather than its duration. It must be borne in mind that the stented artery, although it looks like normal on the pictures, in reality it is not. Stents (expanded metal springs) are susceptible to thrombosis and other complications. Therefore, after stenting for a long time, it is necessary to take not only aspirin, but also another antiplatelet agent, clopidogrel, and this, in turn, increases the risk of bleeding.
In any case, the decision on the treatment method must be made together with the attending physician, therapist or cardiologist, and not with the angiographer or cardiac surgeon - those who perform stenting or bypass surgery.
Causes
IHD occurs as a result of atherosclerosis of large (epicardial) coronary (heart) arteries of varying degrees: from a slight narrowing of the lumen in the vessel to its complete blockage by atheroma (cholesterol, fat) masses or a blood clot that has developed at the site of a “vulnerable” (damaged) atherosclerotic plaque (ASP) . Other causes of IHD are spasm of the coronary arteries and damage to the microvasculature in the myocardium. In most cases, they also develop against the background of existing atherosclerosis.
It is possible to identify the population groups most susceptible to the development of coronary artery disease: people suffering from high blood pressure, those addicted to smoking, those suffering from high cholesterol levels, diabetes mellitus, and chronic kidney diseases. . Male gender and old age are also powerful risk factors for the development of coronary artery disease.
Diagnosis and treatment
The modern tactics of treating such patients is to immediately transport them to a hospital, where it is possible to perform emergency stenting of the coronary artery in which the catastrophe occurred. We must act immediately: about half of those who die from myocardial infarction die within the first hour after the first signs appear.
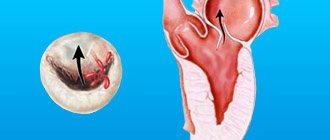
Unstable angina is distinguished from myocardial infarction by the reversibility of myocardial damage: during a heart attack, part of the myocardium supplied with blood from the affected artery dies and is replaced by scar tissue; with unstable angina, this does not happen.
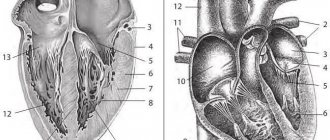
With myocardial infarction, there are characteristic changes in the electrocardiogram, an increase and then a decrease in the level of several proteins - markers of myocardial necrosis, and impaired contractility of several segments of the left ventricle according to echocardiography.
Anterior myocardial infarction has its own complications, while lower myocardial infarction has its own. Thus, with anterior myocardial infarction, cardiogenic shock, pericarditis (the so-called epistenocardiac pericarditis), left ventricular rupture, false and true aneurysms of the left ventricle, dynamic obstruction of the left ventricle, and blockade of the left bundle branch are much more common. Lower infarction is characterized by transient disturbances of atrioventricular conduction, mitral insufficiency, rupture of the interventricular septum, and damage to the right ventricle.
After a period of hospitalization, rehabilitation is carried out: a regimen of physical activity is developed, medications are prescribed for constant use.
Anyone who has had a myocardial infarction should, unless contraindicated, take at least four medications continuously: a beta blocker (eg, metoprolol, bisoprolol, nadolol), an antiplatelet agent (most often aspirin), a statin (eg, atorvastatin, rosuvastatin) and an ACE inhibitor ( enalapril, lisinopril and others). Before discharge from the hospital or immediately after it, it is necessary to conduct a stress test (preferably stress echocardiography) and decide on the advisability of coronary angiography. Share:
Cerebral ischemia
Cerebral ischemia (dyscirculatory encephalopathy, cerebrovascular insufficiency) is a pathology that develops due to a lack of blood flow to the brain. The carotid artery, whose role is to supply blood to most parts of the brain, is especially affected.
Impaired blood flow leads to damage to nerve tissue. If nerve cells die, a stroke occurs.
The mechanism of development of the disease varies from person to person; some are immediately faced with an acute form of the disease, others with a chronic form of the pathology. Much depends on the specific vascular network. In some people, blocked vessels are compensated by neighboring ones, including smaller ones, while in others such compensation does not occur. Neuroses, allergic reactions, neoplasms, and infections can also increase the rate of cell death.
Limb ischemia
Rarely occurs on its own. More often – a manifestation of obliterating atherosclerosis. Deposition of LDL (“bad” cholesterol) on the walls of blood vessels and atherosclerotic plaques provoke blocking and narrowing of the arteries. Blood cannot fully move through the arms and legs.
In the initial stages, we are talking purely about discomfort (hands and feet are constantly cold). Then cracks in the skin and trophic ulcers appear. With advanced disease, there is a high risk of necrosis and gangrene.
A significant breakthrough in the diagnosis of the disease began with the widespread use of duplex scanning of veins and arteries. Timely diagnosis allows you to start treatment as early as possible and avoid amputation of legs and arms.