Angina attack
An attack of angina occurs when there is insufficient blood supply to the heart muscle. Angina should not be considered as an independent disease; rather, it is part of a symptom complex indicating cardiac pathology.
Signs
An integral part of the clinical picture is pain in the chest area. However, if only this symptom is present, it is impossible to talk about a diagnosis. It is necessary to carry out differential diagnosis from pathologies with similar manifestations.
An attack of angina will be indicated by:
- Cardialgia. The pain is pressing and squeezing in nature. Characteristic irradiation to the left half of the body: arm, shoulder, shoulder blade.
- The duration of a painful attack during angina pectoris ranges from a few seconds to 15 minutes.
- It can be triggered by high-intensity stress: both physical and emotional. In case of stable angina, to eliminate pain it is necessary to stop the exercise and take nitroglycerin.
Symptoms of an angina attack differ depending on its type:
- In a stable form, an attack of angina lasts 10-15 minutes. Nitroglycerin and cessation of exposure to provoking factors relieve pain.
- With a progressive form, the duration of the attack is 5-15 minutes. For its development, exposure to a provoking factor is not necessary. Pain can occur at rest, during sleep. Moreover, their intensity increases in the lying position. Nitroglycerin doesn't help.
- The spastic type of angina manifests itself as a short attack - no more than 5 minutes. It can occur in any situation that is accompanied by an increased need for oxygen in the myocardium. Emergency treatment for an angina attack is to take nitroglycerin.
Another sign of angina is difficulty breathing. Its appearance is explained by an increase in the need of myocytes for oxygen, the development of hypoxia, and ischemia. In this case, shortness of breath appears, pain occurs during inhalation, a burning sensation and squeezing in the front of the chest.
Most patients, due to respiratory dysfunction, experience panic attacks due to fear of death.
From the cardiovascular system, the following signs of an angina attack occur:
- numbness of the limbs;
- pale skin;
- high blood pressure;
- change in heart rate;
- increased heart rate;
- headache;
- pre-fainting state.
For patients who tend to have elevated blood pressure, there is a real risk of hypertensive crisis.
8
24/7
Causes
An attack of angina can be a consequence of a number of disorders in the body:
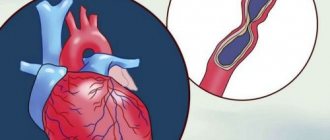
- Myocardial ischemia most often results from atherosclerosis of the coronary vessels - narrowing of the lumen due to the deposition of cholesterol on the walls.
- The myocardial need for oxygen also arises as a result of tachycardia - rapid heartbeat; vessels cannot always cope with the increased load.
- Another reason is arterial hypertension. When blood vessels narrow due to high blood pressure, normal blood flow is disrupted.
Factors that increase the risk of developing an attack include:
- Overweight. The greater the body weight, the higher the likelihood of developing an attack.
- Nicotine addiction.
- High cholesterol levels.
- Diabetes mellitus (increases the risk of developing angina by 2 times).
- Severe stress.
- Hypodynamic lifestyle.
- Arterial hypertension.
- Hypothermia/overheating.
- Drinking alcoholic beverages.
- Spicy food and overeating.
- Increased blood clotting, which increases the risk of blood clots.
In addition to atherosclerotic lesions, the causes of an angina attack may include:
- thromboembolism - blockage of a vessel with a blood clot;
- spasm - a sharp narrowing of the lumen of blood vessels.
Diagnostics
Laboratory tests are required: the patient undergoes a general blood test (CBC) and biochemistry. CBC allows you to determine the level of hemoglobin and platelets. Biochemistry is needed to determine the level of glucose, cholesterol, triglycerides, etc.
Among the instrumental research methods prescribed:
- ECG. Using a cardiogram, they learn about the presence of changes in the heart, myocardial hypertrophy. Prolongation of the cardiac cycle and arrhythmias may indicate a heart attack.
- Holter monitoring. An effective diagnostic method that allows you to take ECG readings over a long period of time (from a day or more). Thanks to the results obtained, it is possible not only to record an attack of angina, but also its duration, and also to identify the causes.
- Load tests. The essence of the procedure is to artificially provoke an attack. The test is accompanied by continuous ECG recording and pressure measurement.
- Scintigraphy. It consists of introducing thallium isotopes into the vessels. Areas affected by ischemia accumulate the substance worse, so there is less radiation from them.
- Echo-KG. During the procedure, the condition of the myocardium is assessed: size, degree of filling of blood vessels, congestion, and impaired blood flow. Angina pectoris is usually accompanied by a deterioration in the mobility of the heart walls in the ischemic area.
- Coronary angiography. Designed to identify vessels affected by atherosclerosis. In addition, you can find out the size of the plaques and the degree of vasoconstriction.
Not all diagnostic methods can be used. The minimum diagnostic set of procedures includes: ECG, EchoCG, stress tests.
The most effective method for studying the severity of angina pectoris and the extent of vascular damage is coronary angiography. It shows the affected areas of the myocardium, their area, and the number of narrowed arteries. Thanks to coronary angiography, thrombosis, tearing of the arterial wall, and spasm are detected. The advantage of the method is the absence of contraindications.
The list of mandatory procedures includes coronary angiography in the following cases:
- angina pectoris of 3-4 functional class, unresponsive/poorly responsive to therapy;
- the presence of symptoms of severe ischemia obtained during ECG, Holter monitoring, stress tests;
- a history of ventricular arrhythmias;
- increase in symptoms despite treatment;
- the need to confirm/refute data obtained as a result of ECG, EchoCG.
8
24/7
How to help someone who is having a seizure
How to relieve an angina attack:
- Control your emotions. You should not panic, as this can lead to increased spasm.
- The patient must be seated in such a way that his legs are down; he is not allowed to stand up. It is important to provide access to fresh air; if a person is indoors, open a window.
- To stop an attack of angina, you need to put a nitroglycerin tablet under your tongue. The concentration of the active substance in the blood after taking the medicine becomes maximum after 4-5 minutes, its decrease is noted after 15 minutes.
- The tablet should be placed under the tongue. Absorption occurs in the oral cavity and the substance quickly reaches the coronary vessels, rather than into the general bloodstream. Vasodilation occurs, blood flow to the myocardium improves, and pain stops.
- Usually the attack goes away within 5-10 minutes after taking the pill. If this does not happen, analgesics should be used, since a prolonged attack may indicate the development of acute myocardial infarction.
- You cannot take nitroglycerin more than 3 times - this can lead to a sharp drop in blood pressure and the development of serious consequences. If the listed emergency aid methods for an angina attack do not help, the patient’s condition does not improve, you need to call a medical team.
It is mandatory to call an ambulance during an angina attack in the following cases:
- the duration of pain is more than 5 minutes, there is no positive dynamics, the pain does not subside;
- first attack of angina;
- intensity increases, accompanied by breathing problems, vomiting;
- in the absence of improvement after taking nitroglycerin.
An attack of angina indicates that the body needs a gentle regime. Therefore, over the next few days, a diet and avoidance of activities with high physical activity are recommended.
Treatment
Treatment of angina pectoris is complex and is aimed at solving the following problems:
- prevention of myocardial infarction and death;
- prevention of disease progression;
- reduction in the number, duration and intensity of attacks.
In addition to taking medications, it is necessary to make adjustments to your lifestyle:
- to refuse from bad habits;
- play sports, providing exercise, the intensity of which has been agreed with the doctor;
- follow a diet and bring your body weight back to normal.
Standard drug treatment includes taking anti-ischemic drugs that reduce myocardial oxygen demand and other medications:
- nitrates;
- beta blockers;
- calcium channel blockers;
- antisclerotic agents;
- antioxidants;
- antiplatelet agents.
8
24/7
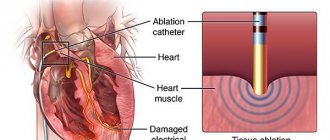
If treatment is ineffective, surgical methods are used:
- coronary artery bypass grafting;
- vascular stenting.
Prevention
It is impossible to completely insure yourself against an attack of angina, but it is necessary to take measures to prevent attacks of angina in order to reduce the risks.
First of all, it is necessary to control body weight, since excess weight is an unobvious impetus for the development of many diseases. All bad habits must be eradicated as early as possible: both smoking and alcohol lead to vasoconstriction, which can result in artery blockage anywhere and at any time.
You cannot neglect existing diseases - the presence of a chronic inflammatory process in the body increases the risk of its spread to the heart.
After an attack of angina, the following recommendations are used as secondary prevention: limit anxiety and the intensity of physical activity, take nitroglycerin before playing sports or emotional situations, and treat existing diseases in a timely manner.
If a person has already experienced an attack, it is necessary to find a specialist who can manage it and monitor it regularly. It is important to prevent the dynamics from deteriorating and not to start the processes of circulatory disorders.
Symptoms
Main symptoms include:
- acute chest pain radiating from the left (or right) side to the lower jaw, arm, shoulder blade
- shortness of breath
- feeling of suffocation and lack of air
- feeling of fear, anxiety
- increased pain in the left chest area when trying to take a deep breath
- increased sweating
- tachycardia
- deviation of blood pressure from normal (low or high).
The main factors in the development of the disease that cause symptoms of angina pectoris include
- age (usually after 40 years)
- gender (men develop CHD on average 10 years earlier than women)
- hereditary factor.
An important role in the formation of the disease is played by excess body weight, a history of diseases such as diabetes, arterial hypertension, increased blood clotting, metabolic syndrome, emotional lability, lack of physical activity, smoking and alcoholism.
Diagnostics
In diagnosing angina, a balanced and competent approach is necessary, because with unstable angina, the patient's condition may worsen until the development of myocardial infarction. Each study must be substantiated.
- ECG
- 24-hour ECG monitoring
- bicycle ergometry or treadmill (stress test with simultaneous ECG recording)
- EchoCG
- stress echocardiography
- coronary angiography
- myocardial scintigraphy
At the EXPERT Clinic, cardiologists are also functional diagnostics doctors. They will weigh all the risks before conducting the examination.