Home→Stenting
We tried to collect the most common questions from our patients and answer them.
- Why is cardiac stenting done?
- How is stenting performed?
- Rehabilitation after stenting
- How long do they live after cardiac stenting?
- Complications, consequences, risks of stenting
- Diet after stenting
- Medications after stenting
- Do they give you disability after stenting?
- Loads after stenting
- Stenting and alcohol
- Is it possible to fly on an airplane after stenting?
- Pain after stenting
Why is cardiac stenting done?
Stenting is carried out in order to restore the patency of the narrowed coronary (coronary) artery, which nourishes the heart, supplies it with oxygen, and thereby return the vital organ to normal functioning. Stenting is performed for coronary heart disease, including its life-threatening manifestation – myocardial infarction.
Stenting in some cases is a modern alternative to open surgery – coronary artery bypass grafting.
How is stenting performed?
Stenting is a minimally invasive operation that is performed under local anesthesia in the cath lab.
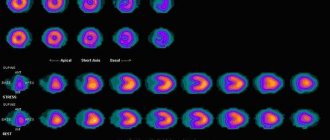
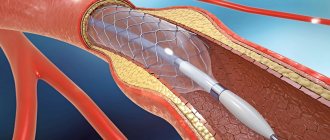
Through puncture of the radial artery in the arm (in most cases) or the femoral artery, the coronary artery is catheterized with a special guiding catheter.
Then a stent is delivered to the area of the coronary artery narrowed by the atherosclerotic plaque through a guidewire. A stent is a metal frame in the form of a compressed tube, placed on a balloon. The balloon is inflated and removed, and the stent remains in the artery as a scaffold, thereby leaving the artery lumen free for blood flow.
Discussion
CEA has proven itself as a method of surgical treatment of ICA stenoses [29, 30]. CAS is an alternative method of correction with equal effectiveness and the absence of complications such as damage to cranial nerves, laryngeal paresis, Horner's syndrome, acute hematomas at the surgical site requiring revision of the paraarterial space, which was also noted in our study [2, 10, 13 , 29, 30].
However, for each of the above methods of correction of the brachiocephalic bed there are specific indications and contraindications, thanks to which CAS, if CEA is not possible, can replace it with less likelihood of dangerous complications [10, 11, 14, 16]. Thus, in our study, clear criteria for choosing CAS were identified in most cases due to the risk of complications associated with a severe comorbid background, which is confirmed in the literature [15, 16, 22, 23, 29, 30].
Perioperative mortality in our study was 2.7% (n=2) compared with 0.7% and 0.6% in the CREST and SAPPHIRE clinical trials, respectively [15–18, 32]. Both cases are associated with a severe comorbid background of patients who had a history of repeated strokes, diabetes mellitus requiring insulin therapy, and post-infarction cardiosclerosis.
Initially, residual symptoms of stroke/TIA occurred in almost half of the patients, which was accompanied by the presence of cysts in the brain. The phenomenon of “luxurious perfusion” after hemodynamic correction aggravates this condition [20, 21, 24, 25, 27]. In addition to the listed reasons, it is necessary to note pronounced atherosclerotic changes in the aorta in the study cohort of patients, which, according to the literature, is a source of atherothrombosis during catheterization of the brachiocephalic arteries during stenting [15–18].
Myocardial infarction, according to foreign authors, is one of the main cardiovascular complications of CAS and CEA in patients with concomitant lesions of the coronary arteries, which is reflected in the presented study [1—10, 15, 17, 24, 32]. This pattern is explained by the presence of multivascular lesions of the coronary bed with high SYNTAX values and occurs due to hemodynamic changes associated with the development of bradycardia during irritation of the carotid glomus and vagus nerve, restoration of normal blood flow after correction of ICA stenosis, as well as artificial hypertension to compensate for cerebral circulation during manipulations with affected carotid artery [1, 5, 10, 29, 30]. Therefore, the cardiac status of each patient must be determined before choosing a carotid revascularization strategy.
Rehabilitation after stenting
Stenting of the heart arteries can greatly improve the patient’s quality of life, but this operation does not stop the atherosclerotic process and does not completely cure coronary heart disease. Therefore, the patient must follow all the recommendations and prescriptions of his attending physician in order to, if possible, stop or slow down the progress of this disease.
Rehabilitation after stenting of the heart arteries includes: drug therapy, physical therapy, diet, lifestyle changes in general: quitting smoking, normalizing body weight if necessary.
The doctor selects drug therapy and exercise therapy for each patient individually.
Rehabilitation period
Recovery after stenting takes minimal time. The patient will stay in the clinic for 6-24 hours, depending on the current condition. This is necessary so that the doctor can monitor the occurrence of complications. You should drink plenty of fluids for 2-3 days after surgery to flush the contrast agent out of your body. It is also necessary to limit physical activity, follow a diet, and give up bad habits. A healthy lifestyle will help prevent the development of complications and restenosis.
Still have questions about carotid artery stenting?
Free consultation with AngioClinic specialists
Author
Salmina Daria Vladimirovna
Geneticist. Graduated from the Chelyabinsk State Medical Academy. She completed an internship at the Northwestern State Medical University named after I.I. Mechnikov.
How long do they live after cardiac stenting?
Stenting does not cure coronary heart disease, but removes the consequences of this disease. The patient's life expectancy depends on many factors, including concomitant pathology. And also in what specific situation the stenting was performed. What is the extent of heart damage? But most of all, the duration depends on the patient’s own attitude. If he changes his lifestyle and follows all the doctor’s recommendations and prescriptions, he will live a long and fruitful life, counting in decades.
Diet after stenting
The diet after stenting includes foods rich in vitamins and fiber, but sharply limits the content of animal fats and the content of quickly digestible carbohydrates.
It is not recommended to eat fatty lamb, beef, pork, butter, lard, mayonnaise and spicy seasonings, sausages, cheese, caviar, pasta from non-durum wheat, chocolate, sweets and baked goods, white bread, coffee, strong tea, alcohol and beer, carbonated sweet drinks.
It is recommended to consume fresh vegetables and fruits, fresh juices, boiled poultry, fish, cereals, durum pasta, cottage cheese, fermented milk products, and green tea.
Medications after stenting
After stenting, it is imperative to take medications prescribed by the cardiologist, such as Plavix or Zilt, and aspirin, to prevent blockage of the stented vessels by a blood clot. The treating cardiologist will select the duration of administration and dosage individually.
And also, in the presence of concomitant diseases, for example hypertension - drugs that lower blood pressure, cholesterol-lowering drugs for high cholesterol levels in the blood, and other necessary medications that were taken before heart stenting.
Is it possible to fly on an airplane after stenting?
If stenting was performed as planned, without previous heart attacks, and in the case of stenting with a myocardial infarction, enough time has passed and the patient has fully recovered, then there are no absolute contraindications to air travel.
In any case, in the process of planning a trip with air travel, the patient must consult with his doctor, undergo the necessary examinations and receive recommendations regarding taking medications before and during air travel.
According to the recommendations of the American Heart Association, air travel is contraindicated in the following situations:
- if less than 6 months have passed since a severe heart attack, and two weeks after an uncomplicated heart attack;
- if a person has manifestations of heart failure that cannot be corrected with medications;
- for severe arrhythmias;
- with persistent arterial hypertension;
- if the patient has unstable angina.
results
The average age of the patients was 65.2±6.6 years (from 45 to 77). The study cohort of patients was characterized by a predominance of males (n=48, 64%), all of them had a long-term history of smoking. The majority of patients (n=70, 93.3%) had NYHA class 1-2 angina. At the same time, a history of myocardial infarction was noted in 17 (22.6%) subjects. All patients suffered from arterial hypertension, while 63 (84%) of them had type 2 diabetes mellitus, 4 (5.3%) had chronic obstructive pulmonary disease, and 11 (14.7%) had chronic renal failure. Atherosclerotic lesions of three arterial territories were noted in 25 (33.3%) people. Multivessel coronary artery disease was observed in 18 (24%) patients.
A history of coronary bypass surgery was performed in 14 (18%) patients. 20 (26.6%) patients had previously undergone percutaneous coronary intervention, 8 had CEA. A history of stroke/TIA was found in 72 (96%) patients, smoking - in 48 (64%) men, bilateral ICA stenoses - in 32 (42.6%) patients.
Among the operated patients, in 5 (6.7%) cases, stenting was performed due to ICA restenosis after CEA, in 7 (9.3%) patients due to high localization of ICA stenosis. The vast majority of patients (n=72, 96%) had a high surgical risk associated with severe comorbid background, while more than half of them (n=37, 54.4%) had symptomatic ICA stenosis ≥80%. A high surgical risk associated with symptomatic stenosis of the carotid arteries up to 50-69% was noted in 4 (5.9%) patients, a risk associated with symptomatic stenosis of the carotid arteries ≥70% in 31 (45.5%) patients. The average severity of atherosclerotic lesions according to the SYNTAX scale in such patients was 17.5±8.1 (from 6 to 41) points, and the average surgical risk according to the EuroScore II scale was 4.7±2.9%.
The in-hospital mortality rate in the total sample of patients was 2.7% (n=2). In one case, the cause of death was ischemic stroke as a result of embolism, in the other - myocardial infarction. Among hospital complications, it is necessary to note stroke and/or transient ischemic attack (TIA) (n=2, 2.7%). 5 (6.6%) patients developed MI. In 2 (2.7%) cases, bleeding occurred from the puncture site of the common femoral artery, which did not require surgical intervention or transfusion of blood components.
Where is stenting performed?
At the Center for X-ray Surgical Methods of Diagnostics and Treatment, employees have extensive experience in endovascular treatment of coronary heart disease. Interventions of varying degrees of complexity are carried out: in acute coronary syndrome, on the trunk of the left coronary artery, bifurcation lesions, as well as recanalization of chronic occlusions using the most modern and innovative instruments. During the year, the department performs approximately 1,500 coronary procedures.
The cost of the work can be found here.
We provide quotas for stenting in more detail.
Documents for obtaining disability
The patient fills out a special form - a referral to medical examination. The examination is carried out at the place of residence of the person counting on disability. If a person cannot get to a medical facility, the commission goes to him.
The documentation package is presented in the Appendix to the Order of the Ministry of Labor and Social Protection:
- passport;
- a referral to ITU filled out by the person or his representative;
- referral from the attending physician for medical examination;
- SNILS;
- medical card, medical history and other documents confirming the patient’s health status;
- a copy of the work book certified by the organization;
- a written description of the nature of work activity and the patient’s responsibilities.
Documents are sent by registered mail to the territorial ITU department. The application (referral) is registered. Within 30 days, the patient undergoes an examination, at the same time an examination must be scheduled - a commission at which specialists will determine the patient’s condition.
During the commission, a protocol is kept on the recognition (not recognition) of a person as disabled. Each member of the commission makes his own verdict on the patient’s condition, after which a report is signed. All votes of participants are summed up.