Memo to a patient who has undergone coronary artery stenting
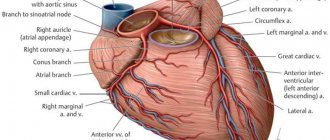
Atherosclerosis is a chronic progressive disease that leads to a decrease in blood flow in the supply area of the artery and oxygen starvation (ischemia) of the organ. Therefore, this disease is called coronary artery disease. If the coronary artery is narrowed, then symptoms of angina pectoris occur; if its lumen is completely blocked, then myocardial infarction occurs. This disease affects a large number of people around the world, incl. in our country. IHD is a leading cause of disability and death. Therefore, treatment of atherosclerosis and coronary heart disease is extremely necessary.
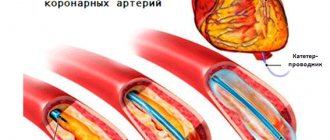
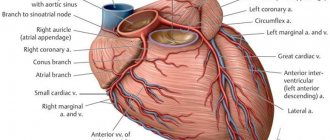
Damage to the coronary arteries can be suspected if characteristic chest pain appears during physical activity, changes during ECG and echocardiography. The most informative method for diagnosing damage to the arteries of the heart is coronary angiography. This study is carried out by puncturing the femoral or radial artery, passing a catheter through the hole to the vessels of the heart and injecting a contrast agent, one at a time, first into the right one. Then into the left coronary artery. The injected X-ray contrast agent, mixing with the blood, flows through the vessels, and at this time the X-ray machine is turned on and records the image in movie mode. After recording the entire series of images, the catheter is removed and the puncture site is pressed to stop bleeding. By assessing changes in the arteries, the X-ray endovascular surgeon can reliably say which treatment tactics can improve the patient’s quality of life - further drug therapy or invasive intervention (angioplasty with stenting or coronary artery bypass grafting).
Angioplasty and stenting of the heart arteries is currently the leading and most effective method of treating coronary heart disease due to a number of advantages:
- access does not require tissue incision and, accordingly, general anesthesia and associated complications;
- the patient communicates freely with the doctor during the entire procedure and usually does not experience any pain;
- The operation itself does not last long, and after it the person must remain in bed for 24 hours, and after a few days he can be discharged for outpatient treatment.
- This intervention can be performed several times throughout life as the disease progresses.
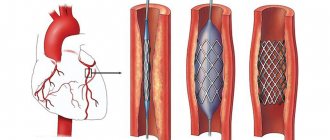
The essence of the technique is to expand the narrowed lumen of the vessel from the inside
a special balloon catheter, which is brought directly to the atherosclerotic plaque. By inflating a balloon selected to the size of the affected segment of the vessel, the plaque is crushed and the lumen of the artery is restored. To ensure that the artery segment remains dilated as long as possible, the arteries are strengthened by installing a special metal mesh tubular frame - a stent.
IMPORTANT! The effect of the intervention depends not only on what and how the stent is installed, but also on the patient’s further compliance with the following rules:
1. Strict blood pressure control
2. Quitting bad habits - smoking and alcohol
3. Regular exercise
With physical activity, blood supply to all organs and systems improves, the emotional state improves, weight decreases, and postoperative recovery accelerates.
4. Compliance with the principles of rational nutrition
- Limiting salt to 3-5 g/day (1 level teaspoon)
- Limiting animal fats (sour cream, fatty meats, poultry)
- Adequate dietary fiber intake
- Limiting cholesterol (offal, egg yolk)
- Consumption of vegetable oils (sunflower, olive, corn) - sources of omega-3 fatty acids
5. Learn to resist stress, avoid conflict situations and not create them
6. Strictly follow all prescriptions and recommendations of the doctor - regularly take medications and undergo prescribed examinations.
IMPORTANT! After stenting, the first step is to take medications that prevent the formation of blood clots: aspirin 75-100 mg/day. for life and clopidogrel 75 mg/day. at least 12 months.
IMPORTANT! You should also take statins, which significantly reduce mortality and the incidence of complications of coronary heart disease. In this case, the target values should be:
- total cholesterol less than 4.5 mmol\l
- low density lipoproteins less than 2.5 mmol/l
If symptoms of angina pectoris return, you should immediately consult a doctor.
It must be remembered that by strictly adhering to the recommendations, you can be sure of improving your quality of life for a long time.
Developed by the head of the RCC of the Central region Bolshovaya E.V.
How to avoid complications after stenting of heart vessels and coronary arteries
Patients most prone to complications after coronary artery stenting are those with various serious chronic diseases - kidney pathologies, diabetes mellitus, various disorders of hematopoietic and coagulation functions. Factors that increase the risk include old age and poor general condition of the patient’s body at the time of surgery.
In order to prevent the development of complications associated with the above reasons during coronary artery stenting, a thorough examination of the health status of the candidate for angioplasty is carried out even at the stage of preparation for the operation. This includes not only an assessment of the condition of the blood vessels, but also a comprehensive examination with attentive attention to all the patient’s complaints, taking into account all the medications he is taking and their possible reactions with medications administered during and after the operation.
Material and methods
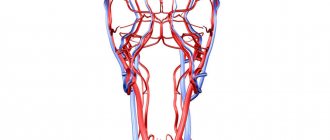
The study included 75 patients with MFA who underwent ICA stenting during the period from 2011 to 2015 at the Kemerovo Cardiology Clinic. All patients underwent CAS with preoperative duplex scanning of the ICA, computed tomography and angiography of the BCA. Indications for CAS were: high stenosis of the ICA, impossibility of performing CEA due to severe comorbidity and the associated perioperative risk of complications. Contraindications for CAS: sharp bends of the vessel and other anatomical and topographical features, allergies to radiopaque agents, calcification of the vessel, extended lesions, stroke within the last 2 months, severe atherosclerosis of the aorta in the area of the ostia of the BCA, severe occlusive-stenotic lesions of the arteries of the extremities [28— thirty].
Indications for CEA included: symptomatic ICA stenosis greater than 60%; asymptomatic damage to the ICA with stenoses of 50-60% in the presence of an unstable atherosclerotic plaque (hematoma inside the plaque, intimal flotation, ulceration, mural thrombus) and stroke/TIA in the last 6 months; asymptomatic stenoses of the ICA 70-99%. Also, based on the latest recommendations, CEE was indicated for patients in the period 6-8 weeks after stroke and 2 weeks after TIA. Contraindications for CEA were: extensive stroke, difficult-to-correct arterial hypertension, MI in the last 6 months, progressive brain pathology (Alzheimer’s disease, etc.), unstable angina, high functional class of heart failure, complicated comorbid background [28-30].
Carotid artery stenting technique
Access is made through the common femoral artery or radial artery. 10,000 units of heparin are administered to prevent thrombus formation under the control of increasing the activated partial thromboplastin time by 2 times the normal value. A controlled catheter or a long guidewire is installed under the bifurcation of the common carotid artery. Next, one of the methods of cerebral protection is used: installation of a filter, distal balloon occlusion, endovascular clamping of the carotid artery, or reversal of blood flow. However, to date, none of them has shown its advantage over the others. To reduce irritation of carotid baroreceptors, glycopyrrolate is administered at a dose of 0.6 mg or atropine at a dose of 0.6-1.2 mg. In case of subocclusion of the artery, for the convenience of stent installation, the stenosis is predilated, then a self-expanding stent is installed. The use of balloon-expandable stents is avoided due to the risk of damage to the vascular wall. This is followed by partial postdilatation (to reduce the risk of embolization) and removal of the mechanical brain protection device.
Endpoints included death, myocardial infarction, stroke, TIA, and bleeding.
Statistical processing of the obtained data was carried out using the Statistica 10 for Windows software package (StatSoft, USA). The samples were checked for compliance with the normal distribution law using the Shapiro-Wilk test.
Introduction
In recent years, carotid artery stenting has partially replaced carotid endarterectomy in many patients [1–5].
However, there are no data from prospective randomized trials comparing two-stage carotid artery stenting and coronary artery bypass grafting (CABG) with a combined surgical approach [6–10]. Long-term results of techniques including brachiocephalic artery (BCA) stenting in addition to myocardial revascularization have also not been published [11, 12]. After carotid artery stenting, there is a need for aggressive antiplatelet therapy, including clopidogrel for at least 1 month and acetylsalicylic acid. Restoration of blood flow through the internal carotid artery (ICA) can provoke hemodynamic changes such as bradycardia and hypotension. These facts make BCA stenting unfavorable for the treatment of patients with severe coronary artery disease (CAD) [1, 5, 9, 13, 14].
The CREST report (2011) showed risk factors for perioperative cardiovascular complications that are common to both endarterectomy and stenting: age over 75 years, operator/surgical experience, mild cognitive impairment or dementia, early post-acute coronary artery disease syndrome [15-18]. Other risk factors are more relevant for increasing the incidence of complications with stenting (large extent of calcified lesion and excessive tortuosity of the ICA). Some risk factors are specific to carotid endarterectomy (CEA) (congestive heart failure, very high or very low stenoses, period after radiation therapy, ipsilateral CEA for contralateral ICA occlusion).
Discussions regarding the choice of method for revascularization of extracranial arteries continue [4, 8, 9, 19, 20]. Thus, K. Ziada et al. in 2005 presented the results of carotid artery stenting and CABG. Among the complications of this tactic were myocardial infarction (3%) and acute cerebrovascular accident (ACVA) (2%) [21].
F. Versaci et al. in 2007 reported the results of a new surgical strategy consisting of a sequential hybrid approach with carotid stenting followed by CABG. The procedure was performed in a group of 37 patients. The total incidence of stroke, myocardial infarction and mortality was 8.1%, 2 (5.4%) patients died, 1 patient suffered a stroke after ICA stenting [22-24].
Lack of data in large numbers of patients and unclear long-term results, as well as the need for aggressive antiplatelet therapy, limit widespread adoption of this approach [3, 20, 25, 26]. In the event of bleeding, postoperative antiplatelet treatment with this strategy may have to be delayed, compromising the patency of the stented ICA.
In addition, when considering the issue of ICA stenting versus CEA, one should keep in mind the data of J. McPhee et al [27]. In a study including all 2005 ICA revascularization procedures in the United States (n=135,701), the authors found that ICA stenting increased the incidence of postoperative stroke and mortality by 4-fold (4.6% vs 1.4%, p<0 .05) in comparison with FEE. In addition, ICA stenting doubles the overall risk of postoperative stroke (1.1% vs. 0.57%, p<0.05) compared with the surgical approach.
M. Van der Vaart et al. in 2008 reviewed 12 randomized trials of carotid artery stenting versus CEA. According to the authors, there is no evidence that carotid artery stenting has an advantage in preventing stroke compared with CEA [28].
In a 2010 study of 2502 patients, T. Brott et al. [17] showed that the incidence of stroke or death over 4 years of follow-up in patients with ICA stenting was 6.4%, and in the CEA group it was 4.7% (p = 0.03). When the MI rate was included in the analysis, the overall rate was 1.1% for stenting versus 2.3% for endarterectomy (p=0.03).
Of interest are also the data from the EVA-3S study, which was stopped early due to a high percentage of stroke and significant mortality in the ICA stenting group compared to the CEA group [29, 30].
When talking about the choice of surgical tactics (CEE or carotid angioplasty with stenting (CAS)), one must take into account the possible risks of complications of each treatment method. Thus, with CEE, damage to the hypoglossal and vagus nerves and laryngeal paresis occur much more often. In the early postoperative period, acute paravasal hematomas may occur, causing compression of surrounding tissues, neck organs and displacement of the trachea, which leads to impaired respiratory function [8-10, 14, 19, 20, 31]. With CAS, during catheterization of the carotid arteries and with severe atherosclerotic lesions of the aorta, damage to its intima and embolism of the BCA by atherothrombotic complexes are possible, which is highly likely to lead to the development of stroke [1, 2, 6]. According to the ICAROS study, echo-negative atherosclerotic stenoses contribute to the formation of the largest percentage of emboli during CAS [29, 30].
The purpose of this study is a retrospective analysis of in-hospital results of ICA stenting in patients with multifocal atherosclerosis (MFA).