Sometimes problems with the cardiovascular system become so serious that conservative treatment methods no longer have the desired effect. If the patient is diagnosed with atherosclerosis, which has seriously affected one or more vessels, surgical intervention is indicated. In the problem area, certain manipulations are carried out aimed at restoring normal vascular patency and the correct functioning of the entire cardiovascular system.
If blood vessels are blocked by atherosclerotic deposits, the heart tissue experiences oxygen starvation. This leads to the occurrence of coronary disease. This condition is extremely dangerous for the patient’s life, especially in the case of complete blockage of the vessel, which entails myocardial infarction. However, today there are effective methods for treating coronary heart disease - stenting and bypass surgery.
What is coronary artery stenting?
More than 2 million stents are implanted annually. And this is understandable, because stents are used to treat one of the most common diseases - coronary heart disease.
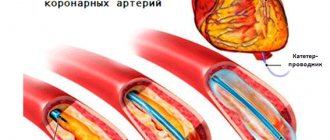
Coronary angioplasty and stenting is an intravascular treatment for coronary heart disease. The basis of coronary heart disease is the narrowing of the blood vessels that supply the heart (coronary arteries) by cholesterol plaques. Stenting allows narrowed arteries to widen. To do this, a special balloon is placed inside the artery and inflated, thus “flattening” the cholesterol plaque and restoring blood flow through the artery. After this, a metal frame—a stent—is implanted into the narrowing site to “fix” the result. In this case, there is no need to open the chest and all manipulations are carried out through a small puncture in the artery in the arm or groin.
Possible risks of coronary angioplasty
Although angioplasty is less invasive than bypass surgery, the procedure still carries some risks. Risks may be associated with the procedure itself and its long-term outcomes.
Early risks:
- Bleeding. There may be bleeding in the leg or arm where the vessel was accessed. Usually it just develops as a bruise, but sometimes there is serious bleeding that may require a blood transfusion or surgery.
- Heart attack. Coronary circulation disorders develop very rarely during surgery, but sometimes, due to technical reasons, a rupture or dissection of the coronary artery may develop. These complications may require emergency coronary artery bypass surgery.
- Kidney problems. The contrast agent used in angioplasty and stent placement can cause kidney damage, especially in people who already have kidney problems. If you are at higher risk, your doctor may take steps to protect your kidneys, such as limiting the amount of contrast material and increasing fluid intake to dilute the contrast.
- Ischemic stroke. During angioplasty, a stroke can occur if pieces of plaque break off as the catheter is passed through the aorta. Stroke is an extremely rare complication of coronary angioplasty. To prevent it, drugs that reduce blood clotting are prescribed.
- Heart arythmy. During the procedure, the heart may beat too fast or too slow. Such arrhythmias are usually short-lived, but sometimes a temporary pacemaker is required.
Late complications
- Repeated narrowing of the artery (restenosis). With angioplasty without stenting, the rate of restenosis is approximately 30% of cases. Stents have been developed to reduce restenosis. The use of plain metal stents reduces the risk of restenosis to 15%, and the use of drug-eluting stents reduces the risk to less than 10%.
- Stent thrombosis. Blood clots (thrombi) can block an artery, causing a heart attack. To reduce the risk of thrombosis, it is important to take aspirin, clopidogrel (Plavix), which helps reduce the risk of blood clots forming in the stent. Never stop taking these medications without talking to your doctor.
Who is indicated for cardiac stenting?
Stenting of cardiac vessels is indicated for patients with severe angina pectoris, after myocardial infarction and pre-infarction conditions, patients with proven ischemia (lack of blood to the heart) based on the results of stress tests. In this case, the decision on stenting is made only based on the results of coronary angiography - a contrast study of the heart vessels. Coronary angiography, like stenting, is performed in the cath lab. Often coronary angiography “transitions” into vascular stenting because performed through the same puncture in the artery.
General recommendations after surgery
Patients after bypass surgery and stenting are advised to have a proper, varied diet. It is necessary to avoid eating fatty, fried and salty foods. Products with high cholesterol content are strictly prohibited. At the request of the patient, you can receive a referral to a nutritionist who will write out the optimal individual diet.
The rehabilitation period after surgery involves taking medications. In addition to the standard set of medications, you must take anticoagulants prescribed by your doctor. Many people refuse them due to the high cost. However, ignoring the cardiologist’s instructions can lead to the formation of a blood clot in the installed stent/replaced area of the vessel.
What alternative methods to stenting exist?
- Drug therapy. You need to understand that it is tablets, and not stents, that primarily reduce the risk of myocardial infarction and determine the prognosis in patients with coronary artery disease. Therefore, in many patients with controlled angina pectoris, in the absence of objective evidence of severe myocardial ischemia (lack of blood), coronary stenting can be abandoned, despite significant narrowing in the coronary arteries.
- Coronary bypass surgery. Abdominal surgery, which is often performed using a heart-lung machine. During bypass surgery, bypasses (shunts) are constructed from the patient’s arteries and veins, allowing blood to be supplied to the heart, bypassing areas of the arteries affected by cholesterol plaques.
Preparation for coronary angiography
To plan the operation, it is necessary to obtain information about the condition of the coronary arteries and heart function. For this purpose, diagnostic tests are carried out, which in an emergency include an ECG and laboratory diagnostics, and in a planned case, a more detailed examination is necessary.
Examination before elective surgery includes:
- ECG (including Holter monitoring)
- Echocardiography (including with load)
- MSCT coronary angiography or preliminary coronary angiography
- Gastroscopy (EGD)
- X-ray of the lungs
Before surgery, you may be given a loading dose of antithrombotic drugs to avoid early thrombotic complications.
How to choose between stenting, bypass surgery and drug therapy?
This is the task of your cardiologist, who takes into account the following data:
- The severity of symptoms, namely: the severity of angina pectoris, the severity of shortness of breath, in other words, how much ischemic disease “interferes with the life” of the patient.
- Objective evidence of myocardial ischemia (lack of blood). Most often this is a stress test, ideally stress echocardiography, which should be performed by qualified doctors in a center with a large number of such studies.
- Coronary angiography data. With widespread severe damage to all three coronary arteries, the results of bypass surgery are better.
- Accompanying illnesses. If a patient has diabetes mellitus and multivessel disease of the heart arteries, for example, coronary bypass surgery is usually indicated.
Disadvantages and advantages
Each method of surgical intervention has its own pros and cons. The doctor evaluates them before deciding on stenting or bypass surgery.
Installation of a shunt preserves the effect of the operation and improves the patient’s quality of life. Another plus is that there is less need for repeat surgery. The shunt allows you to cope with complex cases when drug therapy, stenting or angioplasty do not help.
But this type of operation has many contraindications. It is difficult for the doctor and the patient with a long rehabilitation period. The intervention requires open access.
Stenting solves the problem of single plaques. The operation is minimally invasive and is performed under anesthesia. The advantages include relative cheapness, speed and ease of implementation, and short rehabilitation.
But after stenting, there is a need to operate due to relapses of vascular blockage. The life expectancy of patients after stent installation is shorter than after bypass surgery.
Technique for stenting coronary arteries (with professional jargon)
“We install the introducer”
To get to the heart vessels, the doctor needs to get into the patient’s arterial system. For this purpose, one of the peripheral arteries is used - the femoral (in the groin) or the radial (on the forearm). Under local anesthesia, a puncture is made in the artery and an introducer is installed - a special tube, which is the “entry gate” for all the necessary instruments.
"Let's put a guide"
Then a special thin-walled tube about a meter long - a guiding catheter (“guide”) is passed through the patient’s arteries and stops, slightly short of the heart, in the aorta. It is from the aorta that the coronary arteries that supply the heart depart. The tips of the catheters are curved in such a way that it is convenient for the doctor to enter one of the coronary arteries, right or left. By controlling the catheter, the doctor “enters” one of the coronary arteries. Half the job is done.
“Starting a conductor”
But how to get to the point of maximum narrowing in the artery? To do this, we need a “rail” along which all our tools will “ride”. This rail is the coronary guidewire - a thin (0.014 inch = 0.35 mm) metal “lint” with a soft tip (so as not to “scratch” the artery during the operation). Sometimes it is quite difficult to place a guidewire behind the site of narrowing; the tortuosity of the artery, the angle of departure of the branches of the artery, or pronounced narrowing due to the presence of plaques interfere. You can take a “harder” or “slipperier” conductor. Well, or just a favorite, because every doctor has his own preferences. One way or another, the guide ends up behind the site of narrowing on the periphery of the artery that we want to stent.
"Ballooning"
The first instrument that gets to the site of narrowing of the artery is a coronary balloon with a diameter most often from 1 to 3.5 mm and a length of 10-20 mm. The balloon is put on the conductor and moves along it to the point of maximum narrowing where it inflates. The pressure inside the cylinder reaches 15-20 A
Next, along the conductor, to the place that was narrowed before the balloon was inflated, the same balloon is inserted, on the surface of which a stent is fixed in a folded state. The balloon is inflated, the stent is expanded and “pressed” into the artery wall. The stent does not always expand perfectly and then the final stage of the procedure is needed - postdilatation (in simple terms - re-inflation).
"Let's blow it out"
A rigid balloon is placed inside the implanted stent and inflated with high pressure (up to 25 atmospheres). Most often, after this, the stent straightens and adheres well to the walls of the artery.
Contraindications for surgery
- If intervention is required in an artery with a diameter of less than 3 mm.
- If the patient has a large number of cholesterol plaques, more than 1 centimeter in length.
- If the patient is allergic to iodine-containing drugs.
- If the patient has a large number of cholesterol plaques, more than 1 centimeter in length.
- If the patient has poor blood clotting.
- If the patient has a serious condition, accompanied by a drop in blood pressure, impaired consciousness, shock, liver, kidney or respiratory failure.
- The patient has malignant tumors that cannot be treated.
If a patient is contraindicated for stenting, but still wants this operation, then in some cases he may insist on having it performed at his own risk.
Hemostasis
What to do with a hole in an artery?
If the intervention was carried out through the radial artery (on the arm), a special bracelet with a cushion (hemostatic cuff) is put on the wrist, which will put pressure on the injection site and prevent bleeding. Depending on the situation, the cuff will remain on the arm from 3 to 12 hours.
In case of femoral access, there are 2 main options:
- Manual (manual) hemostasis. After the introducer is removed, the doctor presses with his hands on the injection site for 15 minutes. Then apply a pressure bandage for 6-8 hours. The patient should lie on his back with his leg straight.
- Closure devices are special “plugs” that allow you to close the artery from the inside. In this case, there is no need to put pressure on the leg and a pressure bandage is not needed. A special patch is applied to the injection site and several hours of bed rest are recommended.
Stenting is completed.
Recovery period
During this period, a set of measures is formed for the patient that will help him recover faster and reduce the risk of complications and recurrence of the disease.
After the operation, the patient lies in bed for 1-3 days in the hospital. At this time, doctors closely monitor the patient. After this, the person is discharged home, where he must also be at emotional and physical rest and observe bed rest. He should not take a bath or shower or exert himself physically.
During the recovery period, drug treatment is prescribed for six months, designed to reduce the risk of re-stenosis, thrombosis and heart attack. And increase the length and quality of life.
During the recovery period, the doctor prescribes everything necessary to:
- Improve a person's physical abilities.
- Restore heart functionality.
- Slow down the process of ischemia.
- Bring laboratory parameters back to normal.
- Prevent possible complications after surgery.
- To form in the patient a correct lifestyle that ensures longevity.
- Provide psychological comfort.
Bypass surgery: dangers and possibilities of surgery
Coronary artery bypass grafting is an operation in which normal blood supply to the myocardium is restored by creating a bypass for blood flow through the attached vessels. The coronary arteries run from the aorta to the heart and fill the organ with blood. If the blood flow in them is disrupted, stenting or bypass surgery of the arteries is performed. Bypass surgery makes it possible to shed life for patients with myocardial infarction and increase the body's endurance.
Need for surgery
The decision to perform an intervention is made based on coronary angiography data and clinical manifestations of pathology. Indications based on the results of coronary angiography are:
- obstruction of the left coronary vessel by more than 50%;
- obstruction of all coronary vessels by more than 70%;
- stenosis of 3 coronary vessels, accompanied by severe angina.
Clinical manifestations that are indications for surgery include:
- angina pectoris of 3-4 functional class, not responding to drug treatment;
- acute coronary syndrome;
- acute myocardial infarction no later than 4-6 hours after the attack;
- reduced load tolerance during stress tests;
- severe ischemia detected during Holter monitoring;
- heart defects complicated by ischemia.
8
24/7
Carrying out the operation
Bypass surgery can be performed planned or emergency. In case of emergency hospitalization of a patient, for example, with acute myocardial infarction, preoperative preparation and coronary angiography are carried out, which may result in stenting or bypass surgery.
In such cases, diagnostic procedures are minimal - the most important tests are taken (blood type and blood clotting indicators are determined), and an electrocardiogram is performed.
If bypass surgery is carried out as planned, the list of diagnostic measures expands significantly. It includes:
- electrocardiogram;
- Ultrasound of the heart;
- chest x-ray;
- general blood and urine tests;
- blood biochemistry and clotting test;
- tests for infections (HIV, syphilis, hepatitis);
- coronary angiography.
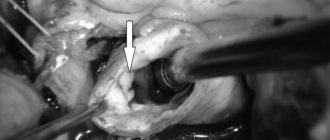
The preoperative stage involves intravenous administration of drugs for anesthesia. Bypass surgery is an intervention in which general anesthesia is given. Its duration is 4-6 hours. Traditionally, the intervention was performed using a sternotomy, which involved cutting the chest. Thanks to modern technologies, it has become possible to carry out minimally invasive manipulations. During this gentle procedure, the heart is accessed through a small intercostal incision. Minimally invasive surgeries last less - about 2 hours, and require less recovery time.
Often, bypass surgery is performed with the connection of artificial circulation, but it can be performed on a beating heart. Coronary bypass surgery, performed on an open heart without connecting artificial blood circulation, significantly reduces the likelihood of complications.
During the operation, the surgeon clamps the aorta, selects a vessel that will be used as a shunt, and attaches it to the affected coronary artery on one side and to the aorta on the other. As a result, a bypass path is created through which blood flow will pass without affecting the damaged vessel. During bypass surgery, several shunts can be installed, their number can range from 2 to 5, and is determined by the number of damaged arteries.
After these manipulations are completed, the edges of the sternum are connected with staples, the surgeon suturing the soft tissues and applying an antiseptic bandage. Drainage must be done, with the help of which hemorrhagic fluid is removed from the pericardial area. The sutures and bandage are removed after 1-1.5 weeks, during which daily dressings are performed.
Contraindications
Contraindications include:
- decreased contractility of the left ventricle;
- poor general health of the patient associated with kidney failure, acute stroke, cancer or lung disease;
- diffuse damage to the coronary vessels (the presence of multiple plaques, which makes it impossible to attach a shunt);
- severe heart failure.
Possible complications
Bypass surgery of the heart vessels rarely leads to negative consequences. At the same time, there is a possibility of developing complications that will affect both the heart and other organs.
The early recovery period can be dangerous for the development of acute myocardial necrosis, which develops into acute infarction. The risks in this case are directly related to the time for which the heart-lung machine was connected - the longer the heart does not work, the higher the likelihood of complications. The prevalence of postoperative infarction is 2-5%.
There is still a small chance that venous bypass grafts may become blocked due to blood clotting in the first weeks after cardiac bypass surgery. The reason for this is the slow conduction of blood by small arteries beyond the implant junction. This process can be prevented by taking aspirin.
Disturbances in the functioning of other organs and systems occur extremely rarely. As a rule, they are caused by chronic diseases and the age of the patients. Possible consequences include acute heart failure, stroke, exacerbation of bronchial asthma, etc. Related to this is the importance of undergoing a full diagnostic examination before surgery and comprehensive preparation of the patient, taking into account all existing pathologies.
8
24/7
Recovery period after surgery
The wound itself heals quite quickly, but the chest wall may take 5-6 months to heal.
Rehabilitation begins in the early postoperative period. They include:
- diet;
- breathing exercises;
- basic physical activity.
Breathing exercises are a mandatory part of recovery procedures. The patient is offered a special device like a balloon. The inflation process leads to the expansion of the lungs, which is the prevention of venous stagnation.
At the initial stage, gymnastics is performed in a lying position. On the 3-4th day you are allowed to get out of bed and move around the ward. Then you are allowed to walk along the corridor. It is advisable to start activity as early as possible, if there are no contraindications to exercise - this will prevent the development of thromboembolism.
In a quarter of patients, normalization of heart rate occurs within 3-4 days after the intervention. As a rule, rhythm disturbances are atrial fibrillation, which is a temporary phenomenon and a direct consequence of the operation.
Be sure to follow a diet - avoid fatty, fried, salty and spicy foods. The basis of nutrition should be vegetables and fruits, fermented milk products, lean meats and fish.
It is necessary to control the level of pressure, taking medications if necessary to lower it.
After discharge, the intensity of physical activity is determined by the physical therapy doctor. The exercises are aimed at strengthening and training the heart muscle and blood vessels. The daily routine should include walking and light morning exercises. Experts recommend spending several weeks after the intervention in a specialized sanatorium. On average, the duration of the rehabilitation period is 1.5-3 months.
Forecast
The prognosis after surgery depends on many factors.
First of all, this is the duration of operation of the shunt. The internal mammary artery has the longest service life. In almost 90% of patients it continues to serve after 5 years. The radial artery is characterized by high efficiency.
Bypass surgery reduces the chance of sudden cardiac death over the next 10 years to 3%. After the intervention, endurance increases and the frequency of angina attacks decreases. More than half of the patients do not experience angina. The probability of developing myocardial infarction during the first 5 years is low and is about 5%.
Registration of disability
Due to the long recovery that is required after bypass surgery, temporary disability is issued - up to 4 months. After this period of time, the patient undergoes a medical and social examination, at which the issue of assignment of disability is decided.
Group III is assigned to people who have an uncomplicated course of the postoperative period with angina FC 1 and 2 (without or in the presence of heart failure). Activities are allowed in areas that do not pose a danger to human cardiac activity. Disability group II is established in the case of a complicated course of the postoperative period.
Group I is given to people with severe heart failure who require care from third parties.
How much heart bypass surgery costs is one of the key questions of concern to patients. The price of bypass surgery depends directly on the surgical technique and consumables. The total cost of bypass surgery may also differ depending on the comfort level of the clinic. Don't waste your precious time - book a consultation with a cardiologist today!
8
24/7
Indications
In what cases is stenting of coronary vessels performed? Often the reason for this is atherosclerosis. It begins due to the accumulation of cholesterol molecules on the walls of the arteries, gradually forming plaques. This complicates blood flow in this area, and the heart muscle experiences a lack of oxygen. As a result, the patient develops coronary disease, the symptom of which is angina pectoris. Retrosternal pain or pain in the heart area, shortness of breath, weakness, make themselves felt during physical activity. Read more about the characteristic signs of an angina attack here.
Cardiac stenting helps prevent the dangerous consequences of coronary artery disease: heart attack and acute coronary syndrome. Coronary stenting is a help for advanced stages of the disease or for emergency treatment of acute coronary syndrome. However, if both vessels are affected or the diameter of the vascular lumen is too small, bypass surgery, an open operation, will give better results.
Rehabilitation
The patient spends the first few hours in the intensive care unit, where the doctor monitors blood pressure levels and heart parameters. If there are no contraindications, during rehabilitation it is recommended to drink more fluid (about two liters per day) so that the body quickly removes the contrast fluid. It is better to avoid heavy lifting and intense exercise. A few days after discharge from the hospital, the patient returns to his normal life.
After surgery, it is important to strictly follow the doctor’s recommendations and attend scheduled cardiologist appointments on time. Taking blood-thinning drugs: aspirin (Cardiomagnyl, thrombo ACC, Cardiasca, etc.) and clopidogrel (Plavix) requires special attention.