BP - blood pressure
LV - left ventricle
CPAP therapy - therapy using continuous positive airway pressure (Russian transcription of the English abbreviation CPAP - continuous positive airway pressure)
OSA - obstructive sleep apnea syndrome
AF - atrial fibrillation
HM - Holter monitoring
ECG - electrocardiogram
Obstructive sleep apnea syndrome (OSA), observed in 22% of men and 17% of women, is closely associated with the incidence and adverse outcomes of various cardiovascular diseases, such as arterial hypertension, coronary heart disease, heart failure, and stroke [1, 2 ]. Patients with OSA are often diagnosed with cardiac rhythm and conduction disorders. It is believed that they may be to blame for cases of sudden nocturnal death, the risk of which is greatly increased in this pathology [3].
In severe OSA, nocturnal bradyarrhythmias are recorded in every second patient [4], and atrial fibrillation is recorded in almost all cases [5, 6]. The use of assisted ventilation (CPAP therapy, the Russian translation of the English abbreviation CPAP - continuous positive airway pressure - constant positive air pressure) allows you to correct breathing disorders during sleep.
Clinical observations [7, 8] and works [4, 9, 10] have been published, which show the possibility of eliminating arrhythmias in patients with OSA with effective CPAP therapy. However, in the existing international and domestic recommendations for the treatment of bradycardia [11] and atrial fibrillation (AF) [12], issues related to the management of this category of patients are not sufficiently covered. In this regard, descriptions of observations of each such patient are important.
Indicative is the clinical case we present of a combination of OSA with long night pauses in the heart rhythm against the background of AF and the successful correction of these disorders using therapy aimed at eliminating obstructive respiratory disorders.
Patient C
., 46 years old, was admitted with complaints of shortness of breath with minor physical exertion, progressive weight gain, loud snoring and “stopping” breathing during sleep (according to relatives).
From the anamnesis it is known that the patient suffered from arterial hypertension for a long time with blood pressure (BP) rising to 180/100 mm Hg; he took antihypertensive drugs irregularly. Approximately 1 month before admission, he noted the appearance of a dry cough, which worsened in a horizontal position, an increase in body temperature to 37.5 °C, and severe weakness. When visiting a doctor at the place of residence, an electrocardiogram (ECG) (see Fig. 1) revealed AF and signs of anterior myocardial infarction with the formation of a left ventricular (LV) aneurysm. The patient was hospitalized in the intensive care unit of the 71st City Clinical Hospital, an elevated troponin level was determined, which made it possible to make a diagnosis of acute myocardial infarction. During therapy with heparin, captopril, furosemide, spironolactone, bisoprolol, aspirin, atorvastatin, and ceftazidime, the patient's condition stabilized and shortness of breath decreased. For further treatment he was transferred to the Research Institute of Cardiology named after. A.L. Myasnikov Federal State Budgetary Institution RKNPK Ministry of Health of the Russian Federation.
Rice. 1. ECG of patient S., 46 years old. AF, heart rate 80 beats/min, signs of focal scar damage to the myocardium of the anterior and lateral wall of the LV with possible formation of an aneurysm.
Upon examination, the patient's condition was moderate. Height 177 cm, body weight 179 kg, body mass index 57 kg/m2. Swelling of the feet and legs up to the middle third. Heart sounds are irregular, atrial fibrillation, heart rate (HR) 84 beats/min, blood pressure (BP) 110/70 mm Hg. In the lungs, breathing is vesicular, with a hard tint, weakened in the lower sections on both sides. The liver is not enlarged.
During clinical and biochemical blood tests, attention was paid to leukocytosis up to 12.5 109/l, an increase in ESR to 70 mm/h, carbohydrate (glucose 7.66 mmol/l; glycated hemoglobin 7.79%) and purine (uric acid 575) disorders .6 µmol/l) exchange.
X-ray of the chest organs revealed signs of venous congestion in the lungs, bilateral pleural effusion (hydrothorax) with the upper border at the level of the VI rib, a slight enlargement of the left chambers of the heart, and a cardiothoracic index of 53%.
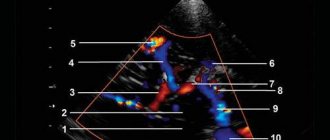
According to echocardiography, the left atrium is enlarged to 4.6 cm, the LV cavity is expanded towards the apex, zones of akinesia with elements of dyskinesia of the apical segments of the interventricular septum and anterior wall are identified, visually the thickness of these segments is reduced (aneurysm), the total LV ejection fraction is preserved (50% ); hypertrophy of the posterior wall of the LV and the unaffected part of the interventricular septum up to 1.2 cm, the aortic and mitral valves without pathology; signs of moderate pulmonary hypertension.
Coronary angiography was performed: the right type of blood supply to the heart, the anterior descending artery in the middle segment is narrowed by 60%, occluded at the border of the middle and distal segments, the circumflex and right coronary arteries have stenoses of up to 40%.
Taking into account the absence of angina pectoris and the presence of pronounced disturbances of local contractility, which corresponded to the zone of blood supply to the occluded anterior descending artery, revascularization was considered inappropriate.
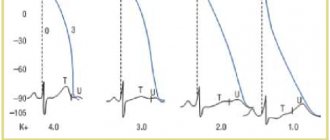
During Holter monitoring (HM) of the ECG against the background of the morning intake of bisoprolol 7.5 mg, atrial fibrillation was recorded during the day with an average heart rate of 86 beats/min, a maximum heart rate of 138 beats/min (when walking around the ward), 22 pauses were identified during night sleep , the maximum of which lasted 14.3 s (see Fig. 2).
Rice. 2. ECG of patient S., 46 years old. fragment of the HM ECG recording after the morning intake of bisoprolol 7.5 mg: against the background of AF, a pause lasting 14.3 s is recorded (arrows indicate the beginning and end of asystole).
Based on the totality of clinical and instrumental data (snoring and “stopping” breathing during sleep, severe obesity, arterial hypertension and long pauses in the heart at night according to HM-ECG data), a diagnosis of obstructive sleep apnea syndrome was made (according to the Berlin questionnaire, it was determined 3 positive categories, indicating a high probability of OSA).
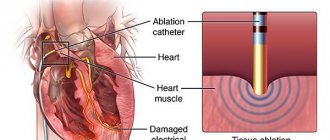
Taking into account the current clinical situation, the danger of reappearance of asystoles in case of delay in prescribing treatment, it was decided to refrain from conducting a control polysomnographic study in order to objectify the severity of OSA. The following night, CPAP therapy was started using the SOMNObalance e device (Weinmann, Germany) under continuous monitoring of the patient’s condition and heart rhythm in an intensive care unit.
When using CPAP therapy with a minimum and maximum air flow pressure level of 4-15 cm H2O, the apnea/hypopnea index was 5.1 episodes per 1 hour of sleep, which meets the criteria for the effectiveness of treatment in relation to the correction of respiratory disorders. According to bedside ECG monitoring, no episodes of asystole lasting more than 2.5 s were recorded against the background of AF.
CPAP therapy was continued on subsequent nights. During treatment, the patient's condition remained stable, no clinically significant pauses in cardiac function were recorded. On the 5th day, sinus rhythm was restored, not accompanied by the development of bradycardia (see Fig. 3). The patient was switched to taking sotalol 120 mg/day, the rest of the drug therapy was left the same. With HM-ECG for 3 days, against the background of sotalol and CPAP therapy (lasting from 6 to 7 hours each night), sinus rhythm was maintained with a minimum heart rate of 53 beats/min, an average heart rate of 81 beats/min, and a maximum heart rate of 117 beats. /min, there were no pauses.
Rice. 3. ECG of patient S., 46 years old. fragment of the HM ECG recording on the 5th day: restoration of sinus rhythm is recorded (the arrow indicates the moment of cessation of AF).
Thus, during CPAP therapy in a patient with persistent AF, sinus rhythm was restored, with no pauses in the heart, which made it possible to refuse the implantation of a pacemaker. The patient was discharged from the hospital with recommendations to follow a diet with limited carbohydrates, animal fats, liquids and table salt, continue taking selected medications and use a CPAP therapy machine every night.
When re-examined after 3, 6, 12 and 24 months, the patient’s condition remains satisfactory, he leads an active lifestyle and works. There is a decrease in body weight from 179 to 91 kg. Signs of coronary and heart failure are not observed. Blood pressure is within 110/70-140/80 mm Hg. The patient continues to use the CPAP machine continuously for an average of about 6 hours per night, which indicates a high degree of compliance with the prescribed treatment regimen.
During the entire observation period, the patient did not report episodes of rapid or irregular heartbeat. With repeated HM-ECG, sinus rhythm was recorded with a minimum heart rate of 45-47 beats/min, an average of 68-72 beats/min and a maximum of 109-115 beats/min without clinically significant disturbances in cardiac rhythm and conduction.
According to echocardiography performed after 24 months, positive dynamics were noted in the form of a decrease in the severity of LV hypertrophy and the size of the left atrium (up to 4.2 cm); the overall contractile function of the LV remains satisfactory (ejection fraction 50%), enlargement of the right heart is not observed, and systolic pressure in the pulmonary artery has normalized.
Causes
There are several reasons for the occurrence of such a problem as reflex cardiac arrest:
- ventricular fibrillation is multidirectional and scattered contractions of the myocardial fiber bundles of the cardiac ventricles;
- ventricular asystole - when the electrical activity of the heart stops;
- gastric paroxysmal tachycardia, in which there is no pulse in large vessels;
- electromechanical dissociation - there is no mechanical activity of the heart in the presence of electrical activity.
Risk factors that increase the causes of cardiac arrest may include:
- coronary heart disease (a disease caused by insufficient blood circulation in the myocardium);
- myocardial infarction (death of cardiac muscle tissue);
- alcohol abuse for heart problems;
- arterial hypertension;
- advanced age;
- smoking;
- drug abuse;
- stress that caused shock;
- effect of low temperatures;
- pulmonary embolism;
- cardiac tamponade;
- pneumothorax;
- receiving electrical injury;
- breathing disorder.
Heart rate in healthy men and women during night sleep
| Age | Men | Women |
| 18-50 years old | max heart rate - 75, min - 45 | max heart rate - 70, min - 40 |
| 51-80 years | max heart rate - 85, min - 50 | max heart rate - 80, min - 45 |
It should be added that the parasympathetic system gains the greatest “power” over the heart around 4 o’clock in the morning - it is at this time, in the deep sleep phase (stage 3), that the maximum slowdown in heart rate is normally observed.
Working at night or not getting enough quality sleep at night leads to an imbalance of the autonomic nervous system - its sympathetic department begins to predominate both day and night. The result is nocturnal tachycardia (an increase in heart rate beyond normal values), rapid depletion of the heart muscle and rhythm disturbances.
Diagnostics
Since sudden cardiac arrest is an emergency, diagnosis can be made within minutes. Cardiac arrest during sleep is common. Conventional measures, which take a lot of time, are inappropriate in this case.
Held:
- physical examination - absence of consciousness and breathing, absence of pulsation is established. Dilated pupils and a pale bluish tint to the skin are also noticeable.
- Electrocardiography (ECG) is a confirmation of heart activity and is used to determine the effectiveness of treatment.
Heart Attack Symptoms
The cessation of cardiac activity ends in clinical death - a reversible condition. If resuscitation is performed correctly, the victim can be brought back to life.
It is important for all adults to know the signs of a borderline state.
If the heart stops, the following symptoms occur:
Advertising:
- loss of consciousness due to oxygen starvation of brain cells (the victim cannot be revived by any effort);
- disappearance of the pulse in the carotid artery;
- uneven breathing (noisy breaths at intervals of up to 2 minutes);
- the skin instantly turns pale and blue;
- dilation of the pupils occurs 2 minutes after blood circulation stops;
- the occurrence of seizures.
Treatment
Emergency care for cardiac arrest includes the following measures, which provide first aid for cardiac arrest:
- indirect cardiac massage (this is a quick blow to the sternum with a fist or the edge of the palm);
- defibrillation (pulsed electrical therapy that helps restore the heart's rhythm);
- 100% oxygen through a mask or through an endotracheal tube.
Emergency drug therapy:
- adrenomimetics (drugs that improve the performance of impulses through the heart and increase the number of its contractions);
- antiarrhythmic drugs (drugs that restore the normal rhythm of contractions);
- m-anticholinergics (drugs that increase contractions and facilitate the conduction of impulses through the heart).
Surgery:
- pericardiocentesis (this is the collection of fluid from the pericardium, which is necessary for cardiac tamponade);
- puncture of the pleural cavity and its further drainage for the treatment of tension pneumothorax.
Complications
The patient will survive if the heart begins to function adequately within ten minutes after it stops. If the person survives, the negative consequences of cardiac arrest may be as follows:
- ischemic damage to the brain, kidneys or liver (as a result of lack of blood supply);
- rib fractures or pneumothorax.
Prevention
Prevention of cardiac arrest includes:
- all cardiovascular diseases that can provoke this condition must be diagnosed and treated in time;
- healthy lifestyle, quitting smoking and alcohol;
- moderate physical activity (light exercise, jogging);
- careful monitoring of blood pressure;
- proper and balanced nutrition;
- tracking and controlling cholesterol levels. An increase in cholesterol is extremely dangerous for the body, as it can cause coronary artery disease, which provokes the risk of cardiac arrest;
- exclusion of low temperatures;
- protection from severe injuries that may result in blood loss;
- control of taking certain medications. These are barbiturates (effective drugs with a hypnotic effect), anesthetics and narcotic painkillers, phenothiazine derivatives and cardiac glycolysis.
Sleep disturbances in anxiety and anxiety-depressive disorders
Combination of sleep disorders and anxiety disorders
It is known that the relationship between sleep disorders and anxiety disorders is observed, on the one hand, when sleep disorders can provoke the development of anxiety disorders [5], and on the other, when the onset of an anxiety disorder precedes the onset of sleep disorders.
Complaints about problems related to sleep are typical for patients with all diseases included in the group of anxiety disorders. In the case of major generalized disorder and post-traumatic stress disorder (PTSD), sleep disturbances are one of the criteria necessary for diagnosis. There are objective reasons for the development of sleep disorders within the framework of anxiety disorders, namely: anxiety is manifested by increased cortical activation, which entails difficulty falling asleep and maintaining sleep. In the clinic, anxiety manifests itself as restlessness, irritability, motor agitation, decreased concentration, and increased fatigue [6].
The most striking manifestation of anxiety disorders is generalized anxiety disorder (GAD), which is diagnosed based on the presence of at least 3 of the following symptoms: restlessness, fatigue, difficulty concentrating, irritability, muscle tension, and sleep disturbances. The duration of the disease must be at least 6 months, the symptoms must cause psychosomatic discomfort and/or social maladjustment.
Sleep disturbances in this situation are one of the 6 diagnostic criteria for GAD. The main symptom of GAD is excessive, persistent anxiety, which is the main factor predisposing to the development of insomnia. Insomnia and GAD are closely related, usually comorbid, disorders. The difference between insomnia due to an anxiety disorder and primary insomnia not associated with other diseases is the nature of the experience during the process of falling asleep. In the case of GAD, the patient is worried about current problems [7] (work, study, relationships), which interferes with the process of falling asleep. In the case of primary insomnia, it is the disease itself that causes concern.
A polysomnographic study can reveal changes characteristic of insomnia: increased time to fall asleep, frequent awakenings, decreased sleep efficiency, and a decrease in its total duration.
Another striking example of anxiety disorders is panic disorder, which is manifested by recurrent states of severe anxiety (panic). The attacks are accompanied by phenomena of depersonalization and derealization, as well as severe autonomic disorders. The patient's behavior shows avoidance of situations in which the attack first occurred. Fear of loneliness and a recurrence of the attack are possible. A panic attack occurs spontaneously, outside of formal situations of danger or threat.
Panic disorder is more common in women and usually begins around age 20. A distinctive feature of panic disorder is spontaneous episodes of panic attacks, characterized by attacks of fear, anxiety and other vegetative manifestations. About 2/3 of patients suffering from this disorder experience some kind of sleep disturbance. Patients complain of difficulty falling asleep, non-restorative sleep, as well as characteristic nocturnal panic attacks. It should be noted that the presence of certain sleep-related problems can lead to worsening anxiety disorders, including panic disorder.
Polysomnographic testing can detect frequent awakenings, decreased sleep efficiency, and a reduction in total sleep duration [8]. It is not uncommon to observe a combination of depression and anxiety disorders, and therefore there is a possibility that the presence of other changes in sleep structure in patients with panic disorder is associated with comorbid depression, therefore it is necessary to exclude the diagnosis of depression in patients with similar sleep disorders.
Sleep paralysis, a characteristic of narcolepsy, can also occur with panic disorder. It is a motor paralysis that occurs when falling asleep or waking up, during which patients experience fear, a feeling of tightness in the chest and other somatic manifestations of anxiety. This symptom also occurs in patients with post-traumatic stress disorder.
Nocturnal panic attacks are a common occurrence in this disease [9]. They manifest themselves with a sudden awakening and all the symptoms characteristic of panic attacks. Awakening occurs during the slow-wave sleep phase, which most likely excludes their connection with dreams. It was also found that night attacks are an indicator of a more severe course of the disease. It must be remembered that patients, fearing a repetition of such episodes, deprive themselves of sleep, which leads to more serious disorders and generally reduces the quality of life of these patients.
PTSD is a disease from the group of anxiety disorders in which sleep disturbances are a diagnostic criterion. Sleep disturbances in this disease include 2 main symptoms: nightmares and insomnia. Other phenomena inherent in PTSD and associated with sleep are: somnambulism, sleep talking, hypnagogic and hypnopompic hallucinations. The changes detected by polysomnography are not specific and in some cases may be absent. Possible changes include: an increase in the representation of the 1st stage of sleep, a decrease in the representation of the 4th stage of sleep. Also, with PTSD, breathing disorders during sleep are often found.
Agoraphobia, which is defined as anxiety that arises in response to situations from which, in the patient’s opinion, is difficult to escape, can also be a manifestation of anxiety disorders. In the clinical picture, as a rule, there is a persistent fear of the patient being in crowded places, public places (shops, open squares and streets, theaters, cinemas, concert halls, workplaces), fear of independent long trips (on various types of transport). The situational component of agoraphobia syndrome is expressed in the confinement of phobic experiences to certain situations and in the fear of getting into situations in which, according to patients, a repetition of painful sensations is likely. Often agoraphobic symptoms cover many fears of various situations, forming panagoraphobia - fear of leaving the house with the development of deep social maladaptation. The patient's attempts to overcome his own experiences are observed; in unfavorable cases, social activities are limited.
Specific phobias are characterized by the connection of anxiety with certain situations (air travel, contact with animals, the sight of blood, etc.), also accompanied by an avoidance reaction. Patients are critical of their experiences, however, phobias have a significant impact on various areas of the patients’ activities. The following forms are found: cardiophobia, cancerophobia, claustrophobia, etc. Sleep disturbances in these patients are nonspecific, and from the patient’s point of view they are a minor manifestation of the disease.
In general, the most common manifestations of sleep disorders in anxiety states are presomnia disorders. The initial phase of sleep consists of 2 components: drowsiness, a kind of desire to sleep, and falling asleep itself. Often, patients have no desire to sleep, no desire to sleep, muscle relaxation does not occur, and they have to perform various actions aimed at falling asleep. In other cases, the desire to sleep is present, but its intensity is reduced, and drowsiness takes on an intermittent, wave-like character. Drowsiness occurs, muscles relax, perception of the environment decreases, the patient takes a comfortable position for falling asleep, and a slight drowsy state appears, but soon it is interrupted, disturbing thoughts and ideas arise in the mind. Subsequently, the state of wakefulness is again replaced by slight drowsiness and superficial drowsiness. Such changes in states can be repeated several times, leading to emotional discomfort that prevents the onset of sleep.
In a number of patients, worries about disturbed sleep can acquire an overvalued-hypochondriacal coloring and, according to the mechanisms of actualization, come to the fore; often an obsessive fear of insomnia arises - agripnophobia. It is usually combined with an anxious and painful expectation of sleep, certain demands on others and the creation of the special conditions noted above for sleep.
Anxious depression is characterized by the patient's constant experience of anxiety, a sense of impending threat and uncertainty. Anxious experiences change: worry about your loved ones, fears about your condition, your actions. The structure of anxious depression, as a rule, includes anxious fears, feelings of guilt, motor restlessness, fussiness, fluctuations in affect with worsening in the evening hours, and somatovegetative symptoms. Anxious and melancholy affects often occur simultaneously; in many cases it is impossible to determine which of them is leading in the patient. Anxious depression most often occurs in people of involutionary age and occurs in protracted phases. In addition, it is actually the leading type of depression of the neurotic level [10].
The patient exhibits a variety of symptoms of anxiety and depression. Initially, one or more somatic symptoms may be detected (for example, fatigue, pain, sleep disturbances). Further questioning reveals depression and/or anxiety.
Signs of anxious depression:
- low mood;
- loss of interests;
- pronounced anxiety.
The following symptoms are also often detected:
- sleep disorders;
- physical weakness and loss of energy;
- fatigue or decreased activity;
- difficulty concentrating, fussiness;
- impaired concentration;
- agitation or inhibition of movements or speech;
- appetite disorders;
- dry mouth;
- tension and anxiety;
- irritability;
- tremor;
- heartbeat;
- dizziness;
- suicidal thoughts.
Often with anxious depression, variants of presomnia disorders are observed, in which the desire to sleep is pronounced, drowsiness increases quickly, and the patient falls asleep relatively easily, but after 5–10 minutes he suddenly wakes up, drowsiness completely disappears, and then for 1–2 hours he does not can fall asleep. This period without sleep is characterized by unpleasant ideas, thoughts, fears, reflecting, to a greater or lesser extent, the experienced conflict situation and the reaction to the inability to sleep. Hyperesthesia to sensory stimuli is also observed. Those suffering from this form of sleep disorder react extremely painfully to the slightest sensory stimuli, even outbursts of passion.
Disturbed sleep patterns are characterized by a prolongation of the drowsy period. This drowsy state is often accompanied by motor, sensory and visceral automatisms, sharp shudders, vivid perceptions of sounds and visual images, palpitations, and sensations of muscle spasms. Often these phenomena, awakening the patient, cause various painful ideas and fears, sometimes acquiring an obsessive character.
Sleep disorders and their polysomnographic manifestations among mental illnesses have been most studied for depressive disorder. Among the sleep disorders associated with depressive disorder, the most common is insomnia. The severity and duration of insomnia are manifestations of a more severe depressive disorder, and the appearance of insomnia during remission indicates the imminent occurrence of a repeated depressive episode [1]. In addition, sleep disorders in this disease are the most persistent symptom. The close relationship of this disorder with sleep disorders is explained by the biochemical processes characteristic of depression. In particular, in depressive disorder there is a decrease in the level of serotonin, which plays a role in initiating REM sleep and organizing delta sleep [11]. Depressive disorder is characterized by the following manifestations of sleep disturbances: difficulty falling asleep [10], non-restorative sleep, and, as a rule, reduced total sleep time. The most specific symptoms for depression are frequent awakenings at night and early terminal awakening. Complaints of difficulty falling asleep are more often observed in young patients, and frequent awakenings are more common in older patients [12].
With masked depression, complaints of sleep disturbances may be the only manifestation of the disease. With depression, in contrast to primary insomnia, there are complaints of sleep disturbances that are typical for this disease: frequent awakenings, early morning awakening, etc. [12].
In a polysomnographic study, the following changes are observed: an increase in the time it takes to fall asleep, a decrease in sleep efficiency. The most common symptoms specific to depressive disorder are shortened REM sleep latency and decreased delta sleep. It has been found that patients with a higher proportion of delta sleep remain in remission longer compared to patients who experience a decrease in the proportion of delta sleep [13].
Attempts have been made to explore the possibility of using depression-specific sleep disturbances as markers of depressive disorder. Due to the heterogeneity of the manifestations of sleep disorders, this issue remains not fully resolved.
The characteristics of sleep disturbances in various types of depression were also highlighted. Patients with a predominance of the anxiety component are more likely to have difficulty falling asleep and early awakenings. With this type of depression, dream plots are associated with persecution, threats, etc. In addition, these patients generally had a high level of wakefulness before falling asleep. For depression with a leading affect of melancholy, early morning awakenings and dreams of static types of gloomy content are most characteristic. Depression with apathy affect is characterized by early awakenings and rare, unsaturated dreams. Also typical for depression with apathetic affect is the loss of the sense of boundaries between sleep and wakefulness. Patients with bipolar disorder have a similar polysomnographic picture [14].
Features of sleep disturbance in bipolar disorder are a significant decrease in sleep duration during a manic episode and a greater tendency of patients to hypersomnia during depressive episodes compared to the unipolar course of the disorder. There are usually no complaints of sleep disturbances during manic episodes.
Treatment
For the treatment of anxiety and depressive disorders, drugs of various pharmacological groups are used: tranquilizers (mainly long-acting or short-acting benzodiazepine drugs), selective serotonin reuptake inhibitors, selective serotonin reuptake stimulants, tricyclic antidepressants. All of these drugs, to one degree or another, affect a person’s sleep, making it easier to fall asleep, reducing the number and duration of night awakenings, thereby affecting the recovery processes that occur during night sleep. When developing tactics for treating sleep disorders combined with anxiety and depressive symptoms, it is important to remember that insomnia itself can increase anxiety, worsen well-being, and mood, usually in the morning after poor sleep [15]. In this regard, the use of hypnotics in treatment may be promising if insomnia symptoms are predominant in the clinical picture in order to prevent exacerbation of anxiety and depressive disorders. In this regard, the most effective assistants can be hypnotics that affect the GABAergic (GABA - γ-aminobutyric acid) system - histamine receptor blockers (Valocordin®-Doxylamine) and melatonin preparation. The most convenient to use in the treatment of insomnia is Valocordin®-Doxylamine, which is available in drops, which allows you to select an individual dose of the drug.
Valocordin®-Doxylamine is a unique drug used as a hypnotic. Most of the known hypnotic drugs (benzodiazepines, cyclopyrrolones, imidazopyridines, etc.) act on the GABAergic complex, activating the activity of somnogenic systems, while histamine receptor blockers act on the waking systems, not sleep, reducing their activation. A fundamentally different mechanism of hypnotic action allows Valocordin®-Doxylamine to be used more widely: when changing one drug to another, reducing the dosage of “habitual hypnotics,” as well as when it is necessary to discontinue hypnotics.
A study of the drug in healthy subjects showed that doxylamine succinate leads to a decrease in the duration of night awakenings and stage 1 sleep and an increase in stage 2 sleep without a significant effect on the duration of the 3rd and 4th stages of sleep and REM sleep. There was no significant subjective effect on the reports of healthy volunteers; however, compared with placebo, doxylamine increased the depth of sleep and improved its quality [16].
In Russia, one of the first studies was carried out under the leadership of A.M. Wayne [17]. It has been shown that under the influence of doxylamine, such subjective characteristics of sleep as the duration of falling asleep, the duration and quality of sleep, the number of night awakenings and the quality of morning awakening improve. Analysis of objective sleep characteristics showed that while taking doxylamine, there is a reduction in the time of wakefulness during sleep, a decrease in the duration of falling asleep, an increase in sleep duration, REM sleep phase time, and the sleep quality index. It was also shown that doxylamine did not reduce the effectiveness of the use of other drugs in patients, such as antihypertensive, vasoactive, etc. The results of a study of the effect of doxylamine on patients with insomnia indicate the effectiveness of this drug in these patients. Subjective feelings of a positive effect are confirmed by objective studies of the structure of sleep, which is undergoing positive changes, which affect indicators such as sleep duration, duration of falling asleep, REM sleep phase. Of great importance is also the absence of any changes in the results of questionnaire data regarding drowsiness and sleep apnea syndrome, which indicates the absence of an aftereffect of the drug in relation to the worsening of obstructive apnea syndrome. However, if obstructive sleep apnea is suspected, doxylamine should be prescribed with caution.
Modern clinical studies do not reveal serious side effects when treated with therapeutic doses of the drug, but it is always necessary to remember the possible appearance of symptoms that arise due to the individual characteristics of the body, and contraindications (glaucoma; difficulty urinating due to benign prostatic hyperplasia; age under 15 years; increased sensitivity to the drug).
Simultaneous use of the drug Valocordin®-Doxylamine and sedatives that affect the central nervous system (CNS): antipsychotics, tranquilizers, antidepressants, hypnotics, analgesics, anesthetics, antiepileptics, may enhance their effect. Procarbazines and antihistamines should be combined with caution to minimize CNS depression and possible drug potentiation. During treatment with Valocordin®-Doxylamine, alcohol should be avoided as it may unpredictably interfere with the effects of doxylamine succinate.
While using this drug, it is recommended to avoid driving a car and operating machinery, as well as other activities accompanied by an increased risk, at least in the first stage of treatment. It is recommended that the attending physician evaluate the individual reaction rate when choosing a dose. These features of the drug’s influence are important to consider when treating patients with insomnia in order to increase the effectiveness of the drug Valocordin®-Doxylamine and eliminate possible undesirable effects.
Conclusion
When diagnosing the disease, it is important to remember that, as a rule, problems falling asleep indicate the presence of severe anxiety, early awakenings are a manifestation of depression. When choosing treatment tactics at all stages of the development of anxiety-depressive syndrome (ADS), the prescription of modern sleeping pills at the stage of unexpressed ADS is a promising tactical approach aimed at reducing the risk of further increase in symptoms of anxiety and depression.
From the history
The term sudden death first appeared in 1917 in the Philippines, where the syndrome was called “bangungut”. Then, in 1959, Japanese doctors called it “smoke”; specialists from Laos, Vietnam and Singapore also wrote about a similar phenomenon.
But as an independent disease, sudden cardiac death syndrome began to stand out in the 80s of the 20th century, thanks to American researchers. During this time, the American Centers for Disease Control in Atlanta recorded an unusually high mortality rate (25 cases per 100,000 people) among young people of Southeast Asian descent. It was noted that their deaths mostly occurred at night, and all the dead were men aged 20 to 49 years. Moreover, most of them were outwardly absolutely healthy, did not suffer from excess weight and did not have bad habits (alcohol, smoking, drugs).
Having compared the data obtained with information from colleagues from the countries of the Far East and Southeast Asia, the researchers found that it is in these regions that cases of this pathology are very common, and more often among young people. At the same time, such a syndrome practically does not occur among African-Americans.