On average, 7-10% of Russians have chronic heart failure (CHF), 4.5% suffer from clinical symptoms of heart failure that reduce quality of life and ability to work, and among people over 65 years of age, half of patients with cardiovascular diseases have symptoms of CHF, and These numbers are increasing every year.
Heart failure is a syndrome caused by abnormal structure and decreased function of the heart. It can be the outcome of diseases such as arterial hypertension, coronary heart disease, heart defects, arrhythmias, kidney and thyroid diseases, cardiomyopathies, hereditary or as a result of infections, intoxications, metabolic and other disorders.
Classification
There is a classification of CHF according to the stages of development of the disease (N.D. Strazhesko, V.Kh. Vasilenko):
Stage I (initial) - signs of deficiency appear only during physical activity, there are no symptoms at rest.
Stage II is divided into two periods:
- period A – clinically pronounced disorder of the right or left side of the heart, congestion in the pulmonary or systemic circulation, shortness of breath and symptoms occur with little physical effort;
- period B – stagnation in both circles of blood circulation (manifested by shortness of breath, swelling), performance is sharply reduced.
Stage III (final) - changes in the structure of organs and tissues, due to impaired blood supply and trophism, shortness of breath at rest.
The severity of the disease is determined by the functional class (FC), which shows how limited the patient’s physical activity is.
- I FC - no restrictions on physical activity. Normal physical activity does not cause excessive shortness of breath, fatigue, or palpitations;
- FC II - minor limitation in physical activity. Feel comfortable at rest, but normal physical activity causes shortness of breath, fatigue, or palpitations;
- III FC is a clear limitation of physical activity. Feeling comfortable at rest but doing less physical activity than usual causes excessive shortness of breath, fatigue, or palpitations;
- IV FC - inability to perform any physical activity without discomfort. Symptoms may be present at rest. With any physical activity, discomfort increases.
The disease should not be allowed to develop; timely diagnosis will help prevent the occurrence of pathology. Our cardiology center of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency invites you to undergo a comprehensive heart examination. Timely identification of the cause of heart failure and its treatment will help maintain your quality of life.
The first signs of illness
Chest pain and discomfort behind the sternum are not the only sign of vascular and heart diseases. You can notice deviations in the functioning of the heart and blood vessels using other signs if you carefully monitor the condition of the body.
The main manifestations of the disease also include:
- arrhythmia that appears in the absence of negative external factors;
- shortness of breath that occurs with obesity, physical activity of an untrained body, excessive overload, the development of vascular and heart diseases;
- swelling, in which there is an accumulation of fluid (usually in the lower extremities towards the end of the day);
- regular headaches, accompanied by increased blood pressure and increased heart rate;
- pathological changes in skin color - pallor in the area of the nasolabial triangle, cyanosis, and also against the background of swelling of the legs.
If such signs appear, you must immediately contact a medical facility for help. You can refute or confirm your fears after an appointment with a specialized physician. For diagnosis, examination, listening to the heart, taking an anamnesis, taking EC and measuring blood pressure is usually sufficient.
Causes of heart failure
The causes of heart failure may lie in concomitant diseases:
- arterial hypertension;
- cardiac ischemia;
- myocardial infarction;
- cardiomyopathy;
- heart defects;
- diabetes.
Experts identify a number of factors that can affect the development of the disease:
- arrhythmia;
- hypertensive crises;
- pneumonia;
- psycho-emotional or physical stress;
- ARVI;
- long-term use of certain medications;
- significant weight gain;
- alcoholism.
Eliminating risk factors will help avoid and prevent the onset of heart failure.
Treatment of functional disorders of the cardiovascular system
Healing from this disease implies complex and individual therapy, which is carried out only under the close supervision of a cardiologist, neurologist and always a psychotherapist. Treatment of a functional disorder of the cardiovascular system depends on the manifestation of symptoms in the patient. It is recommended to avoid stressful situations, proper rest and good nutrition are recommended. Massage, water treatments and reflexology are also prescribed. It is possible to prescribe medications: lemon balm, St. John's wort, valerian, motherwort, glycine, antidepressants, glutamic acid.
Symptoms of heart failure
The symptoms are associated with the inability of the heart to provide adequate blood circulation and the development against this background of congestion in the pulmonary and systemic circulation (in the vessels of the lungs and the vessels of other organs and systems). Stagnation of blood in the lungs interferes with its normal saturation with oxygen and is manifested by shortness of breath. Edema - stagnation in the systemic circulation disrupts the functioning of almost all organs. Patients feel:
- increased fatigue;
- shortness of breath;
- swelling of the legs and feet;
- pain or discomfort in the abdominal cavity due to liver enlargement.
Symptoms of heart failure develop gradually and can sometimes go unnoticed for a long time, so it is necessary to undergo regular medical examinations. At the cardiology center of the Federal Medical and Clinical Center of the Federal Medical and Biological Agency, you can undergo a comprehensive heart examination in order to promptly recognize this syndrome and the diseases that accompany it.
Atypical symptoms of cardiovascular pathology
Every practicing physician, regardless of specialty, regularly encounters complex cases of diseases that occur with atypical symptoms. Uncharacteristic manifestations often cause late diagnosis and untimely initiation of adequate therapy, which significantly worsens the prognosis and increases the frequency of deaths among such patients. Pathology of the cardiovascular system most often occurs with various symptoms typical of other localizations of disorders. The reason for this is that the heart muscle and blood vessels provide blood flow with essential nutrients and oxygen to all organs. Insufficient blood supply is naturally accompanied by disturbances in the functioning of one or another tissue, which is manifested by symptoms of the corresponding localization.
Patients do not always feel the well-known attacks of intense chest pain typical of coronary artery disease [1]. The localization may be different: in other parts of the chest, in the area of the shoulder joints, in the abdomen. The close proximity of the heart muscle to the organs located in the epigastrium causes pain in the upper abdomen, which can be observed when the ventricles of the heart expand due to myocardial ischemia, cardiosclerosis, certain heart rhythm disturbances, defects or carditis [2, 3]. A decrease in the left ventricular ejection fraction, regardless of the immediate cause, causes insufficient blood supply to all abdominal organs, which forms the corresponding pathology: ischemic enterocolitis, gastritis, pancreatitis, hepatitis [4]. Dysfunction of these organs is, to one degree or another, accompanied by nausea, sometimes vomiting, changes in stool, and pain, which often becomes a reason to consult a gastroenterologist. The results of endoscopic, ultrasound and laboratory examinations reveal deviations in accordance with one or another pathology. However, standard therapy, in the absence of adequate treatment of cardiac disease, does not give the expected result.
To illustrate the course of ischemic gastroenterocolitis against the background of coronary heart disease, I give clinical example No. 1.
Man Ya., 46 years old, consulted a therapist with complaints of colicky pain throughout the abdomen with an imperative urge to defecate when jogging, which required stopping the exercise. Within a few hours after the workout, I noticed loose, pasty stools 2-3 times over the course of several hours.
From the anamnesis: the pain first appeared about a week ago. During this period, he noted an increase in fatigue, but denied shortness of breath and palpitations. Previously, he was involved in active sports at the amateur level regularly, for 25 years, but did not participate in competitions. Annual planned examinations as part of medical examination were carried out regularly, no chronic pathology was previously identified, and no drugs were prescribed for continuous use.
On examination: condition is satisfactory. The skin is a little pale. There is no swelling. On auscultation, breathing is vesicular, there are no wheezes, the respiratory rate is 17 per minute. Heart sounds are slightly muffled, 78 beats per minute, rhythmic, no murmurs are heard. Blood pressure - 125/80 mm Hg. Art. The abdomen is soft, the liver is not enlarged. Preliminary diagnosis: irritable bowel syndrome. An additional examination was prescribed: clinical and biochemical blood tests; stool tests: coprogram, bacteriological and dysbacteriosis; ultrasound examination of the abdominal organs, esophagogastroduodenoscopy (EGDS), colonoscopy. Therapy: loperamide 2 mg - 2 capsules 2 times a day, probiotics, sedative herbal medicine.
According to the results of an additional examination: there are no deviations from the norm in the clinical blood test. Biochemical blood test: total cholesterol - 5.6 mmol/l, low-density lipoproteins - 4.3 mmol/l, triglycerides - 3.2 mmol/l, aspartate aminotransferase - 56 U/l, alanine aminotransferase - 21 U/l, total bilirubin - 13 µmol/l. Stool tests revealed remains of undigested food, a moderate amount of digestible fiber, otherwise no pathology, no pathogenic agents or dysbiotic changes. An ultrasound examination of the abdominal organs also revealed no pathological changes. According to the results of endoscopy: chronic gastritis, pathological conclusion: chronic moderately severe inactive gastritis without atrophy and metaplasia, test for Helicobacter - negative. According to the results of colonoscopy: no pathology was detected.
After 7 days, despite regularly taking prescribed medications, the complaints persist.
Due to the lack of effect of treatment, significant data for a gastroenterological disease, but at the same time an increase in aspartate aminotransferase with normal values of alanine aminotransferase and total bilirubin [5, 6], an electrocardiographic study (ECG) was prescribed.
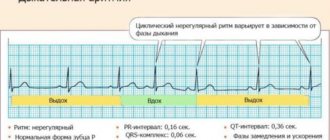
ECG: sinus rhythm, 74 beats per minute, normal position of the electrical axis of the heart, supraventricular and ventricular extrasystole. To clarify the nature of the rhythm disturbance, Holter ECG monitoring was performed.
Analysis of the recording revealed frequent supraventricular and ventricular extrasystole of type 4b/5 according to Lown-Ryan, mainly during physical activity, and episodes of sinus tachycardia. 7728 supraventricular extrasystoles were registered, including 25 couplets, as well as 5458 polymorphic (type 3) ventricular extrasystoles, including 12 couplets, 4 triplets.
In Fig. Figure 1 shows a recording section of 24-hour ECG monitoring, containing supraventricular and ventricular extrasystoles in isolated form, as well as a triplet. An example of identified ventricular couplets is presented in Fig. 2, and supraventricular - in Fig. 3. In the ECG recording area in standard lead II for 1.5 minutes (Fig. 4), frequent extrasystole recorded in this patient is visible.
According to echocardiography (carried out against the background of frequent extrasystole): ejection fraction 52% (according to Teicholtz), hypertrophy of the interventricular septum (18 mm), impaired diastolic function of the left ventricle type I, zones of local hypokinesia and akinesia were not identified, there is no evidence of heart disease.
An additional study in the blood serum: MB-creatine kinase - 18 U/l, troponin I - negative, C-reactive protein - 7 mg/l, anti-myofibrillar antibodies to the myocardium were detected in a titer of 1:80, which indicates an inflammatory process in the myocardium.
Based on the data obtained, a diagnosis was formulated: probable myocarditis, supraventricular and ventricular extrasystole. The diagnosis was confirmed by the results of magnetic resonance imaging of the heart with contrast and ECG synchronization, which meets modern requirements for the diagnosis of these diseases [7].
Thus, the presented example demonstrates the possibility of cardiac pathology with symptoms more characteristic of a gastroenterological disease. However, the appearance or increase in complaints with increasing physical activity indicates heart failure as the immediate cause. A decrease in blood supply to the organs of the gastrointestinal tract can occur with a decrease in the ejection fraction of the left ventricle, both due to the inflammatory process in the heart muscle itself, and independently of this, due to frequent ventricular extrasystole. In other cases, this is possible with increasing coronary insufficiency in patients with coronary heart disease. For the purpose of differential diagnosis, it is necessary to pay attention to the condition of the skin, possible swelling, and during auscultation - to a decrease in the sonority of heart sounds, new noises or rhythm disturbances [8]. This will undoubtedly reduce the likelihood of misdiagnosis.
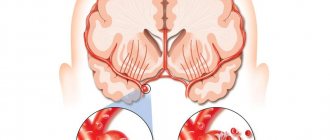
An atypical picture of cardiac pathology can develop with a predominance of completely different symptoms. Impaired blood supply to the brain against the background of various heart pathologies is manifested by typical complaints of dizziness for discirculatory encephalopathy, sometimes fainting, unsteadiness when walking, deterioration in information perception and memorization, noise or ringing in the ears [9]. Possible impairment of vision and/or hearing. In some cases: with endocarditis with the formation of vegetations on the valves and the inner wall of the left ventricle, with atrial fibrillation, severe dilatation of the heart chambers with the absence of adequate antithrombotic therapy, the deterioration of the patient’s condition is associated with thromboembolism. In such situations, the clinical picture usually corresponds to an acute disruption of cerebral blood supply, as confirmed by the results of computed tomography or magnetic resonance imaging. Just as with gastroenterological manifestations, in order to relieve neurological symptoms it is necessary, first of all, to use adequate treatment regimens for cardiac pathology.
A decrease in blood supply to the kidneys naturally leads to the formation of renal failure, which is accompanied by characteristic changes, primarily in laboratory parameters: an increase in creatinine and urea in the blood serum. Other abnormalities are often associated: hyperkalemia, hyperuricemia, hypercalcemia. Complaints of weakness, skin itching, swelling with a predominant localization in the face and with maximum severity after sleep, usually appear later. Signs of renal failure in patients with cardiac pathology, accompanied by a decrease in ejection fraction, are possible in the absence of any independent disease of the renal parenchyma or the collecting system. Successful correction of cardiac parameters in such patients leads to a significant improvement in renal function and relief of clinical symptoms.
Practice shows that patients with cardiac pathology often complain of pain in the joints, back, and muscles. Normalization of the left ventricular ejection fraction and relief of rheological disorders in many cases leads to a noticeable improvement in the subjective and objective characteristics of motor function and a marked decrease in the intensity of pain.
Left ventricular heart failure in any heart pathology is naturally accompanied by an accumulation of blood volume in the pulmonary circulation. Patients are usually bothered by a dry or wet cough, sometimes streaked with blood [1, 10]. It is well known that most often this is manifested by moist, silent rales that are auscultated over the lower parts of the lungs. However, there may be other variants of symptoms, which significantly complicates differential diagnosis. In patients who are in a horizontal position most of the time, wheezing quite often spreads to all parts of the chest, which must be differentiated from developing pulmonary edema. The appearance of fluid in the alveoli gives crepitus, and accumulation in the tissues can lead to compression with narrowing of the lumen of small caliber bronchi, which is accompanied by obstructive wheezing. This situation turns out to be the most difficult, since all the symptoms characteristic of broncho-obstructive syndrome develop: expiratory shortness of breath with wheezing exhalation and reliable signs of obstruction based on the results of an assessment of external respiratory function. A distinctive feature that should be paid special attention to is the insignificant or incomplete effect of the bronchodilators commonly used in such situations. In some cases, due to tachycardia and natural myocardial ischemia developing against their background, health deteriorates with increasing shortness of breath or pain.
To illustrate another variant of the atypical, but at the same time natural course of cardiac pathology, I give clinical example No. 2.
Man K., 39 years old, consulted a therapist with complaints of paroxysmal dry cough, mixed shortness of breath when walking at a moderate pace, and dizziness.
From the anamnesis: deterioration of health was noted within 3 weeks, when coughing and fatigue when walking appeared. I took herbal expectorants on my own, but without effect. Previously, similar symptoms were of concern in acute respiratory diseases. However, unlike previous episodes, this time there was no runny nose, sore throat, or fever. Denies smoking and other bad habits. There were no allergic reactions. No chronic pathology was previously detected.
Upon examination, the condition is closer to moderate. Body temperature - 36.7 °C. Overweight (122 kg with a height of 182 cm) Moderate pasty legs. The skin is slightly pale, the lips are cyanotic. On auscultation, breathing is harsh, carried out in all parts, scattered wheezing in a small amount, in the lower parts - moist, silent wheezing on both sides. The respiratory rate is 22 per minute. Heart sounds are muffled, arrhythmic, heart rate is 106 beats per minute. Blood pressure - 128/92 mm Hg. Art. The abdomen is soft, the liver is +2 cm from the edge of the costal arch.
Preliminary diagnosis: acute obstructive bronchitis.
An additional examination and therapy were prescribed: azithromycin 500 mg per day, probiotics, inhalations with Berodual 4 times a day, Lazolvan 90 mg per day.
Based on the data obtained, it was determined: in the clinical blood test - without pathological abnormalities; in biochemical - total cholesterol - 6.8 mmol/l, low-density lipoproteins - 4.9 mmol/l, triglycerides - 4.2 mmol/l, creatinine - 145 µmol/l, urea - 12.3 µmol/l. The x-ray shows an increase in the vascular pattern, signs of congestion in the pulmonary circulation, a pronounced enlargement of the heart in diameter: cardiothoracic index = 72%.
During treatment, after 5 days the patient notices a deterioration in health, and therefore further examination is carried out to determine the condition of the heart.
The ECG recorded an abnormal supraventricular rhythm with a frequency of 102–140 per minute, atrial fibrillation, repolarization disturbance (ST depression up to 1.5 mm) in the lateral regions.
According to the results of echocardiography, the left ventricular ejection fraction (according to Teicholz) is 44%, pronounced atrial dilatation, moderate ventricular dilatation. There is no evidence of heart disease.
Taking into account the identified changes, a diagnosis was made: atrial fibrillation of unknown duration, cardiomyopathy (?) of unknown etiology, circulatory failure stage II B according to Strazhesko-Vasilenko, functional class III according to NYHA [1, 10]. Rhythm restoration is not indicated due to atrial dilatation.
Treatment was prescribed in accordance with the data obtained: rivaroxaban, carvedilol, starting with small doses; spironolactone, torsemide, maintenance dose of digoxin with heart rate adjustment. With this therapy, the patient's well-being improved significantly. Cough and dizziness do not bother me. He tolerates household physical activity much better.
When examined after 3 weeks: the condition is satisfactory. There is no swelling. The skin is of normal color. Auscultation: vesicular breathing, no wheezing. The respiratory rate is 16 per minute. Heart sounds are muffled, arrhythmic, heart rate is 70 beats per minute. Blood pressure - 118/82 mm Hg. Art. Liver +1 cm from the edge of the costal arch.
During further examination, cardiac magnetic resonance imaging with contrast was performed, which confirmed the presence of dilated cardiomyopathy in the patient.
The presented example shows the possibility of symptoms atypical for cardiac pathology that naturally accompany severe heart pathology in the absence of any significant other disease.
Thus, cardiac diseases can naturally occur with symptoms of pathology of other organs and systems. The correct diagnosis can be made with a thorough analysis of the history, examination and the results of additional examination.
Literature
- Belenkov Yu. N., Oganov R. G. Cardiology: national guide. M.: GEOTAR-Media, 2007. 1232 p.
- Ruzhentsova T. A. Diagnosis and treatment of myocardial lesions in children with acute intestinal infections (clinical experimental study). Author's abstract. dis. ... doc. honey. Sci. M., 2021. 48 p.
- Ruzhentsova T. A. Infectious myocarditis // Practicing doctor today. 2013; 1:48–56.
- Maev I.V., Kazyulin A.N., Kucheryavyi Yu.A. Chronic pancreatitis. M.: Medicine, 2005. 504 p.
- Rosly I. M., Abramov S. V. Principles for assessing enzymological blood parameters in infectious pathology (I message) // Infectious diseases. 2003; 1(1):58–63.
- Rosly I. M., Abramov S. V., Belova E. G., Eremushkina Ya. M. Principles for assessing enzymological blood parameters in patients with infectious pathology (II message): intoxication syndrome // Infectious diseases. 2004; 2 (1): 12–18.
- Caforio AL, Pankuweit S, Arbustini E et al. Current state of knowledge on aetiology, diagnosis, management and therapy of myocarditis. A position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases // Eur. Heart J. 2013; 34:2636–2648.
- Ruzhentsova T. A. Gastroenterological masks of cardiovascular pathology // Experimental and clinical gastroenterology. 2016; 130(6):114–117.
- Tobias JD, Deshpande JK, Johns JA, Nichols DG Inflammotary heart disease/Ed. DG Nichols et al. Critical Heart Disease in Infant and Children. 2nd ed. — Philadelphia, PA: Mosby. 2006: 899–925.
- Yancy CW, Jessup M, Bozkurt B et al. ACCF/AHA guideline of management of heart failure: a report of the American College of Cardiology Foundation: American Heart Association Task Force on Practice Guidelines // J. Am. Coll. Cardiol. 2013; 62:1495–1539.
T. A. Ruzhentsova, Doctor of Medical Sciences
Federal Budgetary Institution Central Research Institute of Epidemiology of Rospotrebnadzor, Moscow
Contact Information
Diagnostics
When collecting anamnesis, the doctor pays special attention to the presence of complaints of shortness of breath and fatigue. Collects information about the existence of other diseases. If heart failure is suspected, the patient is referred for instrumental studies and laboratory tests.
The Cardiology Center of the Federal Medical and Clinical Center of the Federal Medical and Biological Agency carries out a full range of diagnostic measures:
- ECG in 12 leads;
- ECHO-KG;
- Holter monitoring;
- ECG with dosed physical activity;
- transesophageal ECHO-CG;
- ABPM (24-hour blood pressure monitoring);
- Ultrasound of the abdominal organs;
- general blood analysis;
- biochemical blood test (lipid spectrum, blood glucose, liver and kidney function indicators);
- thyroid hormones;
- coagulogram (a test to determine blood clotting);
- general urine analysis;
- spirometry (respiratory function test);
Symptoms of functional disorders of the cardiovascular system
Symptoms of FNS include increased sweating, pallor or slight redness of the skin on the face, periodic fainting, headache, paroxysmal or constantly increased beating of the heart muscle (tachycardia), tachypnea, heaviness and pressure in the chest, impaired blood pressure, shortness of breath. The patient may also experience rapid fatigue, decreased attention and memory, be overly hot-tempered, irritable, suffer from insomnia and experience a constant state of anxiety. There may be various jumps in body temperature (from 35 to 37-38 degrees), nausea, vomiting, belching, diarrhea, frequent urination, anorgasmia with normal sexual desire, constipation. All this signals the Federal Tax Service.
Treatment of heart failure
When treating heart failure, the main focus is on eliminating the cause of the disease. Depending on the nature of the disease, its course and the general condition of the patient, the doctor chooses a treatment method.
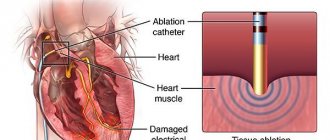
On the basis of our cardiology center, the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency, there are therapeutic and surgical departments. You may be required to undergo examination and selection of drug therapy in our hospital. If drug treatment is not effective enough, the cardiologist may recommend surgery. Specialists of the Cardiac Surgery Department of the Federal Scientific Center for Medical and Biological Agency successfully use advanced methods of treating heart failure. This could be an operation to correct valve disease, coronary heart disease, or arrhythmias. Our clinic performs unique minimally invasive surgeries.
Causes of functional disorders of the cardiovascular system
Nowadays, there are many reasons that can lead to the acquisition of the Federal Tax Service. The cause of this disease can be the harmful effects of various factors on the human nervous system. Our body is one whole, and the fact that negative influences on the nervous system lead to changes in the functioning of the entire organism has long been no secret.
The reason for the FTS may be factors such as:
- Impact of chronic diseases
- Improper lifestyle (disturbance in daily routine, poor sleep, etc.)
- Depression
- Severe stress
- Heredity