Bundle branch block is a disorder of intracardiac conduction, characterized by a slowdown or complete cessation of the conduction of excitation impulses along one or more branches of the His bundle. Bundle branch block can be detected only during instrumental examination or symptomatically manifested by rhythm disturbances, dizziness, and attacks of loss of consciousness. Bundle branch block is diagnosed using electrocardiography. Treatment of bundle branch block is reduced to eliminating the causes of conduction disturbances; In some cases, it may be necessary to install an artificial heart pacemaker.
Causes
Diseases such as:
- congenital and acquired heart defects - stenosis of the aortic and mitral valves, pulmonary artery stenosis, stenosis and coarctation of the aortic mouth, aortic valve insufficiency, atrial septal defect;
- cardiomyopathy, myocardial dystrophy of various origins - endocrine (thyrotoxicosis, diabetes mellitus), metabolic (anemia), nutritional (alcoholism, obesity), autoimmune (systemic lupus erythematosus, rheumatoid arthritis);
- cardiac ischemia;
- cardiosclerosis, as the outcome of many cardiac diseases, leads to the replacement of part of the muscle fibers with scar tissue, including atypical muscle fibers;
- myocarditis of viral or bacterial origin;
- heart damage due to rheumatism - endocarditis, myocarditis;
- myocardial infarction;
- long-term arterial hypertension, leading to myocardial hypertrophy;
- intoxication with cardiac glycosides;
- pulmonary embolism;
- chronic lung diseases (chronic obstructive bronchitis, pulmonary emphysema, severe bronchial asthma), leading to the formation of cor pulmonale - stagnation of blood in the right atrium and ventricle with their hypertrophy and expansion.
In young children and adolescents, incomplete single-fascicle right blockade may accompany minor anomalies in cardiac development, and in the absence of organic heart damage is considered a normal variant. One- or two-fascicular left blockade is almost always associated with acquired rather than congenital heart diseases and cannot be regarded as a normal variant.
Symptoms
Many clinical cases of the disease occur without any symptoms. Incomplete single-fascicle blocks almost never show symptoms, so they are detected only by ECG during a routine examination. But with complete blockade of the right leg, symptoms are usually observed in a person even in the absence of organic heart damage. These include:
- various changes when listening to heart sounds;
- dizziness;
- presyncope and fainting;
- feeling of lack of air;
- dyspnea;
- decreased performance;
- poor exercise tolerance;
- fatigue and weakness;
- sometimes pain in the heart area;
- feeling of interruptions in the work of the heart.
In addition, it is possible that a clinical picture will appear that corresponds to the underlying disease - both cardiac and affecting other organs and systems. The most serious symptoms appear in acute cardiac pathologies - heart failure, myocardial infarction, which are most often accompanied by various heart blocks against the background of damage to the ventricular myocardium.
What is right bundle branch block and how to live with it?
Every year, more and more people suffer from diseases of the cardiovascular system, which pose a serious threat not only to health and well-being, but also to life. Failures in the normal functioning of the heart are increasingly being identified in people of a younger age category, which is associated with lifestyle (the influence of cigarettes, alcohol, lack of sleep, stressful situations, etc.). Cardiac pathologies include disruptions in electrical conductivity; this process is called right bundle branch block, which provokes a slowdown in the contractile function of the heart.
Dysfunction of impulse conduction is not formed as a primary process; it usually acts as an addition to cardiac pathologies and manifests itself as a manifestation of the primary pathology. Right bundle branch blocks affect older men more than women. That is why all elderly patients should regularly visit the cardiology office at their place of residence.
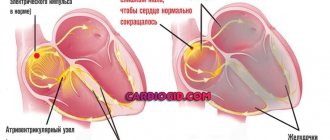
The His bundle is the concentration of atypical fibers in the heart muscle. In the intracardiac septum, fibers form the right and left legs, along which excitation waves pass, responsible for normal contraction of the myocardium.
What are the risk factors?
Taking into account the variants of the course in clinical cardiology, this process is conventionally divided into partial and complete.
With partial damage, the wave passes along the right leg, the work of the left or one of its branches is preserved, the waves pass through healthy fibers, but this process occurs with a delay - this is exactly what a first-degree blockade happens.
If excitation occurs in an incomplete volume, grade 2 is diagnosed.
When a condition such as complete blockade of the right bundle branch develops, the signals are completely blocked.
8
24/7
During an electrocardiographic test, pathology can occur as intermittent (periodic) or permanent. In some patients, blockade occurs only when the heart rate increases or decreases.
Blockade of the right bundle branch is always preceded by valvular disorders or pathologies of the coronary system; they are visible on the ECG. In clinical cardiology, it is customary to distinguish the following pathological factors:
- overdose or long-term use of certain medications: antiarrhythmic drugs;
- persistent increase in the number of thyroid hormones in the body;
- water-electrolyte imbalance;
- history of severe endocrine pathologies;
- alimentary (primary) obesity;
- iron deficiency in the body;
- prolonged use of alcohol in large doses;
- insulin-resistant syndrome;
- disorders of the functioning of the immune system (autoimmune processes);
- PE (blockage of the pulmonary artery by a thrombus or its branches);
- COPD;
- smoking for a long period.
The set of anatomical structures of the heart has a complex structure, which is why the disease occurs in the following types:
- conduction failure on one fiber;
- along two fibers (along the right and anterior left branches);
- All branches of the bundle are involved in the process.
Why does it happen?
Cardiac failures, as provocateurs of blockade along the right bundle branch, are as follows:
- congenital or acquired heart disease throughout life: stenosis of the atrioventricular orifice and aortic valve, coarctation of the aorta, valvular insufficiency, anomalies of the interatrial septum);
- diseases that result in structural and functional disorders in the myocardium, in the absence of pathologies of the coronary arteries and valve apparatus, as well as under conditions of normal blood pressure;
- cardiac ischemia;
- dystrophic processes in the myocardium;
- Brugada syndrome (gene mutation characterized by a high risk of sudden cardiac death);
- history of myocardial infarction;
- pathological hypertrophy of the left ventricular wall;
- fibrous changes in impulse conduction fibers;
- myocarditis.
Clinical picture
The disease can occur without symptoms or have changes on the ECG; blockade of the right bundle branch can be expressed by dizziness, even fainting, and a slowing of the heart rate (bradycardia).
At an appointment with a specialist, right bundle branch block is diagnosed based on changes detected during a preventive electrocardiogram or when looking for other cardiovascular diseases; usually this diagnosis is spontaneous.
In the absence of symptoms, the doctor’s main task is timely prevention of further manifestations.
A single-bundle lesion does not have specific symptoms. Clinical signs are observed as a result of three-fascicle blockade and manifest themselves in the form of severe bradycardia (with heart rate less than 30 beats per minute), disturbances in the frequency and depth of respiratory function in the absence of physical activity, arrhythmia, dizziness, short-term fainting and the appearance of cyanosis on the skin.
Diagnosis of pathology
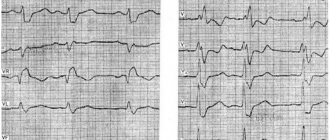
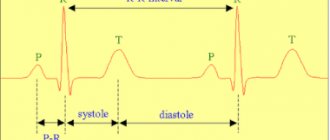
Conduction disorders can be identified during an examination by a cardiologist based on complaints, most often on an ECG; long-term ECG recording is carried out, which is characterized by recording electrocardiogram indicators for 24 hours or more using a special portable device. This method makes sense if the disease was caused by cardiac diseases.
8
24/7
TEE is necessary to assess rhythm and cardiac contractility by applying small doses of electrical current to the area of the heart that is closest to the esophagus.
Laboratory tests are not very informative; they are not able to detect right bundle branch block; blood tests are prescribed to determine the underlying cause of the disease.
After making an accurate diagnosis, consultation with specialists in the field of cardiology and cardiac surgery is required.
Therapy at different stages
Treatment of people with right bundle branch block with drugs involves reducing the severity of the primary disease. If disruption of the electrical impulse is accompanied by heart failure, persistent hypertension or angina, maintenance therapy is indicated, for example: drugs of the nitrate group, antiarrhythmic and cardiotonic herbal drugs and antihypertensive drugs.
In the presence of a latent course, patient management tactics involve monitoring the condition with a cardiologist.
If atrioventricular (AV) or trifascicular block occurs, the cardiologist, together with the cardiac surgeon, offers patients the installation of a pacemaker, in other words, a pacemaker, which regulates the contraction cycle and normalizes the heart rhythm.
Forecast
Detection of the disease in the early stages allows for the necessary treatment and increases the patient’s chances of living longer.
How long do they live?
Why is right bundle branch block dangerous and what awaits the patient in the future? The prognosis of life is directly related to the root cause of development, an important place is occupied by the clinical variant of the course and the severity of the symptomatic complex. When diagnosing a single-bundle lesion, the prognosis is conditionally favorable.
Blockade of the right bundle branch without appropriate measures can lead to sudden death; life expectancy with such disorders does not exceed 4 years. If the causative factor is myocardial infarction, and during the course of the pathology angina pectoris, an increase in heart size, and atrial fibrillation are added, there is a significant deterioration in the patient’s condition and the risk of death increases.
Disease prevention
Pathologies of the heart and blood vessels have many symptoms that can worsen the quality of life and influence the development of severe conditions that pose a huge danger to life. By adhering to some recommendations, you can reduce the risk of developing CVS pathologies in the future:
- it is necessary to adjust the diet: include fresh fruits and vegetables in the daily diet, give up fatty, fried foods, smoked and pickled foods; It is preferable to choose lean varieties of meat;
- compliance with the drinking regime - at least 1.5-2 liters of water per day;
- adequate sleep, at least 8 hours a day;
- It is very useful to take daily walks in the fresh air and do gymnastics;
- give up alcoholic drinks and cigarettes;
- If possible, reduce stressful situations and nervous experiences.
Only timely confirmation of right bundle branch block will allow the necessary examination to be carried out and adequate treatment to be prescribed. At the first symptoms of cardiac disorders, you should immediately seek qualified medical help, often this can save a person’s life.
8
24/7
Diagnostics
The diagnosis of bundle branch block can be established on the basis of a general examination, palpation of the pulse, auscultation (listening) of the heart, general and biochemical blood and urine tests, and analysis of hormonal status - it can reveal causes of blockage not related to heart disease. To make a diagnosis, you will also need electrocardiography (ECG) data, which allows you to identify changes characteristic of each type of blockade. Also necessary are indicators of daily ECG monitoring (Holter monitoring) - a diagnostic procedure that involves the patient wearing a portable ECG device throughout the day. At the same time, a diary is kept in which all the patient’s actions are recorded (getting up, eating, physical activity, emotional anxiety, deterioration in health, going to bed, waking up at night). ECG and diary data are compared, thus identifying intermittent cardiac conduction disturbances associated with physical activity, food intake, stress, or night blockades. Data from an electrophysiological study (stimulation of the heart with small electrical impulses with simultaneous recording of an ECG) can be informative. The procedure is performed through the esophagus (the electrode is inserted through the esophagus; only the atria can be stimulated) or invasively (the electrode is inserted into the heart cavity by inserting a special catheter through a large blood vessel). It is used in cases where ECG results do not provide unambiguous information about the type of blockade, fainting, and also to assess the condition of the conduction system of the heart. Ultrasound examination of the heart can identify cardiac causes of blockade.
Complications, prognosis
Complications of bundle blockade include: ventricular fibrillation, paroxysmal tachycardia, thromboembolism, heart failure (acute, chronic) and asystole.
The prognosis in this case depends on the underlying disease, since bundle block is just a sign of it. The most favorable prognosis is with blockade of the right leg.
If you still have questions, including whether they are drafted into the army for a bundle branch block, make an appointment and consult with a doctor. Registration is carried out on the website and by telephone.
Related services: Cardiac Check-up Diagnosis of heart rhythm disorders by ECG monitoring
Treatment
There is no special course of therapy to treat the pathology. A patient with right bundle block does not require treatment. To a patient who has a single-fascicle or double-fascicular blockade, the cardiologist prescribes antioxidants, vitamins, sedative herbal medicines, antihypertensive drugs for arterial hypertension, ananginal drugs for coronary heart disease, antiplatelet agents to prevent the formation of blood clots in the heart and blood vessels. In severe cases, surgical intervention is required - installation of a pacemaker. With complete right blockade, when myocardial infarction develops, temporary cardiac pacing is required. In this procedure, an electrode is inserted into the right ventricle through a central vein. Permanent pacing is required with a three-fascicular block in the event of a Stokes attack (loss of consciousness).