We present the next article in our series of publications devoted to various forms of IHD (coronary heart disease). Today we will talk about arrhythmias.
Heart rhythm and conduction disorders are a large group of transient or permanent disorders, mainly arising from organic lesions of the cardiovascular system. They are caused by violations of the most important functions of the myocardium: automaticity, excitability and conductivity.
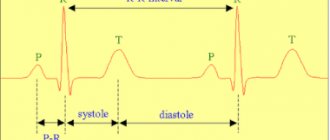
Cardiac arrhythmias is a collective concept for a number of different disturbances in the frequency, rhythm and sequence of heart contractions. Diagnosis of coronary heart disease is carried out using an ECG.
The resting heart rate of most healthy people is 60–75 beats per minute.
What it is
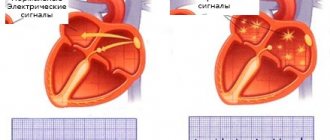
Normally, the impulse originates in the sinus node of the right atrium - where the superior vena cava flows into it.
Next, the wave travels through the atria and ends up at the next control point - the atrioventricular localization node. From here the excitation goes through the His bundle and gradually spreads to the apex. His fibers are special cells of the interventricular septum that form three branches. The right bundle branch (RBBB) delivers signals to the walls of the right ventricle. Along the left (LNPG), which is divided into anterior and posterior branches, there is coverage of the left ventricle. At the end, the branches divide into Purkinje fibers. This structure allows the impulse to be transmitted without loss and ensures uninterrupted heart function.
Conduction is slow and impaired - is there a difference?
In a healthy organ, impulses move from top to bottom in a set rhythm, with the required speed. With pathology, their conduction is slowed down or disrupted. If the passage of the signal is inhibited, excitation reaches the end point, but this process occurs at a slower speed. If conduction is disrupted, the impulse is interrupted in a certain area or is completely absent.
Impairment and slowing of intraventricular conduction occur at different ages. We cannot unambiguously estimate how often this pathology is detected. Failures in the conduction system of the heart often remain asymptomatic and are detected accidentally during a preventive examination. According to the medical literature, various types of conduction disorders are diagnosed mainly after 50 years (5–7% of cases). At 60–70 years of age, the frequency of detection of such conditions reaches 30%.
Failure of intraventricular conduction belongs to the group of bradyarrhythmias. Intra-atrial conduction disorders belong to this category. The causes and symptoms of the development of these conditions are similar. An accurate diagnosis can only be made after an examination.
Ventricular conduction system
To understand exactly how such pathological conditions develop, it is necessary to know what exactly the conduction system consists of, which is responsible for transmitting impulses through the ventricles. Thus, the leading role in this process belongs to the so-called His bundle, consisting of two structural parts:
- Left leg. It is represented by the anterior and posterior branches, each of which is responsible for its own wall in the left ventricle. Their branches form the Purkinje fiber system.
- Right leg. It is represented by one bundle, branching in the lower parts of the right ventricle.
To cause excitation in the ventricles, an impulse from the pacemaker passes through the interventricular septum and then simultaneous excitation of both ventricles occurs. It takes approximately 0.12 seconds for this to happen.
If blockades are noted on one of the conduction pathways, not only the path along which the impulse passes changes, but also the time during which the ventricles are excited.
Reasons for the development of pathology
All possible causes of failure can be divided into two large groups: cardiac - caused by heart pathology and non-cardiac - provoked by other disorders.
Cardiac factors:
- heart defects;
- myocardial infarction;
- myocarditis;
- cardiac ischemia;
- cardiomyopathy;
- atherosclerosis of coronary vessels;
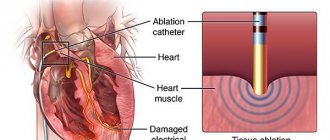
- consequences of previous surgical interventions (for example, due to valve replacement, radiofrequency catheter ablation).
Non-cardiac factors:
- vegetative-vascular dystonia;
- endocrine problems: hypothyroidism, diabetes;
- disorders of the respiratory system with tissue hypoxia - bronchospasms, chronic inflammation;
- irrational use of medications;
- arterial hypertension;
- alcohol poisoning;
- taking drugs;
- pregnancy.
Signal failure does not always indicate pathology. For example, partial disruption of conduction along the right bundle branch is considered a normal variant, characteristic of some young people.
Violation of the conductive function of the myocardium can be permanent or transient. Temporary “problems” are detected against the background of physical activity (for example, during training and competitions). If after rest the situation returns to normal, there is no cause for concern. But if the problem persists and changes are visible on the ECG, you need to be examined by a specialist.
What is the disease expressed in?
Right leg lesion
In situations where there is a complete block of the right leg, excitation of the right ventricle is carried out in a different way. The impulse to the right ventricle comes from the left parts of the interventricular septum. That is, the excitation of the left sections is initially noted, and only then the right ones. If there is an incomplete block, the right ventricle is excited correctly, but the impulse conduction speed will decrease.
Typically, the causes of right leg blockade are the following diseases:
- Chronic lung pathologies.
- Mitral stenosis.
- Cardiac ischemia.
- Myocardial infarction with a large ischemic zone.
- Congenital malformations.
- Diseases accompanied by damage to the valvular apparatus of the heart.
- Also among the factors that increase the risk of developing this pathology are hypertension, as well as improper use of adrenergic blockers. It is also worth noting that in some athletes, conduction disturbances in the right leg may be a normal variant.
One of the features that is necessary for the occurrence of this lesion is overload of the right ventricle. This type of disease practically does not occur in healthy people.
Lesion of the left anterior branch
For this disorder to occur, there must be an obstacle that interferes with the conduction of the impulse to the lateral and anterior wall of the left ventricle. In this case, the excitation passes through the healthy branch and from the lower wall passes to the parts of the heart that remain without an impulse.
The main cause of occurrence can be called pathological processes affecting the left side of the heart in one way or another, namely:
This blockade does not occur as an independent disease.
Lesion of the left posterior branch
The following pathologies lead to the development of this condition:
- Myocardial infarction.
- Atherosclerosis.
- Inflammatory diseases of the myocardium.
- Sclerosis of the conduction system.
With a complete blockade, the impossibility of the impulse to travel along a typical path is noted, therefore, as in the case of a blockade of the anterior branch, excitation passes from bottom to top, through the Purkinje fibers. Most often, there is a combined lesion of both the left posterior branch and the right leg.
Double bundle lesions
The causes of blockades affecting two bundles are diseases such as:
- Rheumatic carditis.
- Myocarditis of diphtheria nature.
- Severe atherosclerosis.
- Myocardial infarction.
The following variants of double-bundle blockades are distinguished:
- Complete blockade of the left leg.
- Blockade of the posterior branch of the left leg with complete blockade of the right.
- Blockade of the anterior branch of the left leg with complete blockade of the right.
Most often, two-bundle blockades are harbingers of damage to all bundles and the occurrence of a three-bundle blockade.
Trifascicular lesions
The same lesions as in the case of two-fascicles lead to the formation of a blockade of all three bundles. When there is a complete loss of the ability to conduct along the His bundles, pauses in the work of the ventricles occur. Thus, an independent rhythm of excitation of these parts of the heart occurs. At the same time, the atria continue to work as usual. This can lead to complete atrioventricular block.
Symptoms: what most often bothers a person
Intraventricular conduction failure has no specific symptoms. Often this condition remains unrecognized for a long time. The patient does not complain about anything, and the problem is discovered by chance - during medical examination, undergoing a medical examination before starting work or study, serving in the army, before surgery, etc.
Possible signs of pathology:
- feeling of “freezing” in the chest;
- interruptions in the functioning of the heart - the appearance of extraordinary contractions;
- slow heart rate;
- dyspnea;
- feeling of lack of air;
- dizziness;
- worry, anxiety.
As the process progresses, Morgagni-Adams-Stokes syndrome (MAS) develops. At the beginning of the attack, the patient turns pale and loses consciousness. After the condition improves, redness of the skin persists. Such episodes last 1–2 minutes and are caused by insufficient blood supply to the brain due to a sharp decrease in cardiac output. Neurological complications are usually not observed.
Degrees and their symptoms
Heart blocks are classified not only by the place of its development, but also by the degree of severity, which reflects the danger of the disease to human health and approaches to treating a particular stage of heart block. There are three main stages of heart block
First degree heart block
The first degree is the mildest form of manifestation. There is a delay of a fraction of a second in the time required for electrical impulses to travel through the atrioventricular junction. Complete blocking does not occur and the impulses reach the desired point.
First-degree heart block usually does not cause any noticeable symptoms and is diagnosed by examining other medical conditions in the person. Treatment may be limited to eliminating risk factors that affect heart health.
Second degree heart block
As the second degree develops, there is a series of increasing delays in the time it takes for the atrioventricular junction to conduct an impulse into the ventricles until the heart beat is missed. Partial blocking of impulses is possible.
The second degree is divided into 2 types:
- The first type of Mobitz. This is a less serious type of second-degree heart block. Characterized by slow conduction of impulses. May cause symptoms of mild dizziness and weakness. Usually does not require treatment.
- Mobitz's second type. Electrical signals reach the ventricles slowly or may be completely blocked. This type of heart block can often progress to third degree heart block. May cause symptoms of dizziness and fainting, accompanied by bradycardia. Requires medical consultation and full treatment.
Third degree heart block
Third degree heart block is the most dangerous degree for a person’s health and life and requires immediate medical attention. It is characterized by complete blocking of the transmission of electrical impulses from the atria to the ventricles due to the lack of communication between the atrioventricular junction and the ventricles.
In this case, the ventricles can partially take over the function of a pacemaker, but they are not able to ensure full functioning of the heart.
Third degree blocks can be congenital or acquired as a result of other heart diseases or injuries.
Symptoms include:
- shortness of breath;
- weakness;
- fainting conditions;
- chest pain;
- pale skin, spots;
- arrhythmia.
Many cases of third-degree congenital heart block are diagnosed during pregnancy because ultrasound scans can often determine whether the baby has bradycardia.
Important! If the diagnosis is missed during pregnancy, symptoms of third-degree congenital heart block usually do not appear until the baby is older and his heart is more developed.
Clinical case
Patient M., 65 years old, was admitted to the therapeutic department. At the time of examination, he complains of shortness of breath during physical activity, frequent attacks of dizziness, and general weakness. There were repeated losses of consciousness.
During the interview, we found out that similar symptoms had been bothering her for more than a year. Over the course of 14 months, severe weakness, headaches, and dizziness are noted. For six months there were losses of consciousness - about once a week. Over the past month, fainting has occurred almost daily. The patient loses consciousness for one minute, then general weakness is noted.
During further examination, changes were detected on the ECG. Ultrasound and Doppler sonography were performed and left ventricular failure and valvular stenosis were detected. Diagnosis: Coronary heart disease; rhythm disturbances such as bifascicular blockade and attacks of MAS; heart failure stage I
The patient was fitted with a pacemaker, her condition improved, and she was discharged.
Based on the nature of the violations, they are distinguished:
- Incomplete blockade. Impulse conduction is slow, but it is preserved. Excitation of the myocardium occurs due to intact branches. This condition occurs in healthy people, but can also indicate pathology. Changes are usually discovered incidentally on an ECG. The patients have no complaints, sometimes there is general weakness and increased fatigue.
- Complete blockade. The impulses do not reach the lower parts of the ventricles. There is a high probability of cardiac arrest due to bradycardia. This condition is accompanied by obvious clinical symptoms.
By type of violation there are:
- Focal changes are observed in certain areas of the myocardium closer to the Purkinje fibers, the impulse partially passes through the ventricles.
- Arborization changes - signal transmission is preserved in all parts of the conduction system, except for its terminal sections.
Classification of bundle branch blocks
According to the generally accepted classification, all blocks of impulse conduction to the ventricles are divided as follows:
- One-, two-, or three-beam. This is determined by exactly how many beams are involved in the incorrect conduction of impulses.
- Local. Conduction disturbances are not observed in all leads during an ECG examination.
- Transitional. Incorrect impulse conduction alternates with normal impulse conduction.
- Arborization. Impulse blockade occurs in the Purkinje fibers. More precisely, in their lower sections.
- Complete blockades.
- Incomplete blockades.
- Alternating blockades. When conducting research, one or another option is revealed.
Diagnostics: signs on ECG and Holter
Electrocardiography is the main method for diagnosing the pathological process. Violation of intraventricular conduction on the ECG will manifest itself with specific signs.
A block along the right leg of the heart leads to expansion and deformation (the appearance of notches) in the QRS complex. Such changes are determined through the right chest leads.
Left heart branch block also widens and distorts the QRS, but pathological signs are detected through the left precordial leads. If the left anterior branch is affected, then a deviation of the electrical axis of the heart to the left is observed. The diagnosis can be confirmed by comparing ECG waves - in the second and third leads, S will be higher than R. If the impulses do not go through the left posterior branch, then the axis deviates to the right, S is higher than R in the first lead.
Nonspecific heart blockades deserve special attention. An ECG reveals changes that do not correspond to a specific pathology. For example, the QRS complex changes - it splits and deforms without widening. Such symptoms are observed with local damage to heart tissue against the background of a heart attack, inflammatory process, etc.
Additional information is provided by the following research methods:
- cardiac echocardiography;
- X-ray of the lungs;
- functional tests;
- CT scan.
We obtain significant information about the work of the heart muscle when conducting Holter ECG monitoring. The study lasts 24 hours. This method allows for continuous recording of signals and identification of abnormalities that are not visible on a conventional cardiogram. Such a recording shows changes that occur not only at rest, but also during movement and physical activity. The compact recorder is attached to the belt. The patient leads a normal lifestyle, and the system records the work of the heart in a continuous mode.
It is important to understand: the success of diagnosis will directly depend on whether the blockade is permanent or transient and how often attacks occur in the latter case. If conduction disturbances are observed daily, daily monitoring will reveal this on the ECG. Sometimes cardiogram monitoring is required for 7-30 days.
Diagnosis of intraventricular block
To diagnose pathology, standard methods are used such as:
- ECG;
- 24-hour ECG monitoring
It will not be difficult for a specialist to notice typical changes characteristic of pathology on the electrocardiogram. When monitoring, even blockades of a non-permanent nature are detected, which occur occasionally when the heart rate increases.
Diagnostics may also include:
- Ultrasound of the heart. The technique will allow us to identify defects of the septum and heart valves, as well as previous heart attacks.
- Coronary angiography. This technique allows you to study the patency of the coronary arteries. Typically, an examination is performed before installing a shunt or stent.
Principles of treatment
Moderate conduction disorders do not require treatment. Incomplete blocking in the right branch of the His bundle is not dangerous. In this situation, we recommend seeing a cardiologist, undergoing an annual medical examination and having an ECG. But this is if the patient has no other complaints or concomitant pathologies. If deviations are detected, appropriate therapy is indicated.
Left ventricular block is more dangerous. Against this background, blood flow disorders and heart failure often develop. We recommend taking cardiac glycosides, antiarrhythmic and other drugs. The treatment regimen is determined individually based on the severity of the condition, the patient’s age, and concomitant diseases.
It is important to know: specific treatment for intraventricular block has not been developed. The proposed drugs only increase the excitation of heart tissue, but do not eliminate the cause. It is necessary to treat the underlying pathology - the one that caused a malfunction of the conduction system. This is the only way to slow down the progression of the disease.
If drug therapy is ineffective or the patient's condition is severe, surgical treatment is suggested. A pacemaker is installed - a device that imposes its own rhythm on the heart. The implanted device ensures uninterrupted myocardial activity.
Prevention
- Compliance with the work and rest regime.
- A rational and balanced diet (eating foods high in fiber (vegetables, fruits, herbs), avoiding fried, canned, too hot and spicy foods).
- Elimination of stressful situations.
- Taking medications under the supervision of a physician.
- Timely diagnosis and treatment of diseases of the heart and other organs.
- Contact a specialist if symptoms of the disease appear.
Read more about pediatric cardiology at the YugMed clinic
Expert advice: when to install a pacemaker
Installation of a pacemaker is a surgical procedure and is prescribed only when indicated.
There is no point in carrying out the procedure in the absence of obvious symptoms of pathology. If the patient feels well, the introduction of an artificial pacemaker is not indicated. Surgery is not recommended if the identified symptoms are associated with reversible causes. You need to cope with the underlying disease - and the heart muscle will be able to function fully again. Indications for installation of a pacemaker:
- bradycardia with a heart rate less than 40 beats/min and rhythm disturbances in the presence of obvious symptoms;
- complications that threaten the patient's life;
- MAS attacks;
- persistent conduction disturbances after myocardial infarction.
The possibility of installing a pacemaker is being discussed when the pulse is less than 40 beats/min in the absence of obvious clinical symptoms. The procedure is performed at any age.
Prevention of cardiac conduction disorders has not yet been developed. Do not delay treatment, avoid risk factors. This will reduce the chances of developing pathology. To identify the problem in time, regularly undergo preventive examinations with a therapist with an ECG assessment (as necessary).
Heart rhythm and conduction disorders - changes in the normal order of heart contractions due to disorders of the functions of automaticity, excitability, conductivity and contractility. Rhythm disturbances are one of the most common manifestations of heart disease and other pathological conditions. The same rhythm disturbances are observed in children as in adults, but the causes of their occurrence, course, approaches to treatment and prognosis have a number of features.There are no reliable data on the prevalence of rhythm disturbances in children. In the structure of cardiovascular diseases in childhood, arrhythmias account for (according to the incidence) from 2.3 to 27%, but they are often detected in healthy children. Heart rhythm and conduction disturbances are found in children of all ages, including newborns; they are detected even in the fetus. The frequency increases during puberty.
Etiology and pathogenesis
Rhythm disturbances can be congenital or acquired and are caused by cardiac, extracardiac and combined causes. Cardiac causes of arrhythmia include congenital and acquired heart defects, rheumatic carditis and non-rheumatic carditis, infective endocarditis, cardiomyopathies and other heart diseases.
A clear relationship between rhythm disturbances and MVP and other minor anomalies of cardiac development has been revealed. Arrhythmias can develop with diseases of the nervous and endocrine systems, many somatic disorders, acute and chronic infectious pathologies, intoxication, overdose or inadequate reaction to medications, deficiency of certain microelements (magnesium, selenium). The formation of rhythm disturbances is influenced by emotional and physical overload, as well as vegetative dystonia syndrome and psychogenic disorders associated with extracardiac pathology.
The main pathogenetic factor of arrhythmias is considered to be disturbances in the formation of impulses and/or the speed of excitation as a result of inhibition of the function of the sinus node, activation of ectopic pacemakers and the functioning of additional pathways. These disorders arise as a result of inflammatory, dystrophic, necrotic and sclerotic processes in the cardiac muscle and cardiac conduction system or as a result of electrolyte imbalance, leading to changes in cellular metabolism and the ionic composition of the internal environment of cardiomyocytes.
In childhood, arrhythmias are more often of extracardiac origin. In this case, perinatal pathology plays an important role (unfavorable course of pregnancy and childbirth, prematurity, intrauterine malnutrition, infection), leading to disruption of morphogenesis and functional immaturity of the conduction system of the heart. Perinatal damage to the central nervous system can lead to disruption of neurovegetative rhythm regulation with a change in the relationship between the sympathetic and parasympathetic parts of the autonomic nervous system, resulting in electrical instability of the myocardium and conduction system of the heart, as well as a decrease in the functional reserves of adaptation of the sympathoadrenal link of heart rate regulation.
Classification
- Automatic disorders (nomotopic - sinus arrhythmia, tachycardia and bradycardia, heterotopic - extrasystole, paroxysmal and non-paroxysmal tachycardia, flutter and fibrillation of the atria and ventricles).
- Conduction disorders (sinoauricular, intraatrial, atrioventricular, intraventricular blockade).
- Combined arrhythmias (sick sinus syndrome, atrioventricular dissociation, premature ventricular excitation syndrome).
Clinical picture
The history of children with rhythm disturbances often reveals an unfavorable course of the perinatal period, a family history of cardiovascular pathology, repeated acute infectious diseases and foci of chronic infection. During examination, hypertensive-hydrocephalic syndrome, residual neurological symptoms, various psychovegetative disorders, manifestations of connective tissue dysplasia, and sometimes delayed motor development and puberty are often detected.
Rhythm disturbances in children are often asymptomatic, which makes it difficult to accurately determine the time of their onset. In approximately 40% of cases, arrhythmias are detected by chance (on an ECG) or during examination in connection with a history of acute respiratory viral infection. Children are much less likely than adults to complain of palpitations, a feeling of interruptions in the activity of the heart, and its freezing, even with severe forms of arrhythmia. Along with this, in prepubertal and pubertal age, rhythm disturbances can have a strong emotional coloring, caused by psycho-vegetative disorders, and be accompanied by other cardiac and extracardiac complaints: pain in the heart, increased excitability, sleep disturbances, and meteosensitivity. With arrhythmias, weakness, dizziness and fainting are possible (with sinus bradycardia, atrioventricular block, sick sinus syndrome, paroxysmal tachycardia).
An objective examination of children with rhythm disturbances can reveal an increase or decrease in the pulse, a change in its character (irregular with periodic drops, alternating periods of increase and decrease, temporary or permanent weakening of the pulse wave, the presence of a compensatory pause). Assessing other basic characteristics of the cardiovascular system (blood pressure, heart size, sonority of sounds, heart murmurs) makes it possible to establish or exclude cardiac pathology as the cause of arrhythmia.
Diagnostics
The main method for identifying and assessing arrhythmias is ECG. With its help, it is possible to detect such asymptomatic rhythm disturbances as single extrasystoles, Wolff-Parkinson-White syndrome, slowing of atrioventricular conduction, and pacemaker migration. Often, when performing an ECG in children, sinus arrhythmia and isolated incomplete blockade of the right bundle branch are detected, which are a variant of the age norm.
Clinical electrocardiographic examination allows us to establish the type of rhythm disturbances (functional or organic), especially extrasystoles. Extrasystoles of functional origin are most often detected in the pre- and pubertal periods; they are not constant, usually disappear or are significantly reduced with changes in body position and physical activity. Extrasystoles most often originate from the right ventricle or are of supraventricular origin.
In order to clarify the origin of rhythm disturbances, cardio-intervalography, daily Holter ECG monitoring, functional tests are performed: stress tests (test with dosed physical activity, bicycle ergometry, treadmill test) and medicinal tests [atropine, with propranolol, isoprenaline (isadrine), gilurhythmal, etc. ]. If organic heart disease is suspected, an x-ray examination and echocardiography are performed. An assessment of the child’s vegetative and psychological status, a neurophysiological examination [EEG, echoencephalography (EchoEG), REG], consultations with a neurologist, otolaryngologist, endocrinologist, and ophthalmologist are also necessary.
Holter monitoring allows much more often than a standard ECG to detect rhythm disturbances even in healthy children (pacemaker migration, extrasystole, etc.) and determine their relationship with periods of the day and night sleep (circadian dependence), which is important for the choice of treatment method.
A study of the state of the autonomic nervous system confirms the significant role of its dysfunction in arrhythmias. Thus, the predominance of parasympathetic with insufficiency of sympathetic influences is found in cases of extrasystoles, slowing of atrioventricular conduction, as well as in children with chronic tachyarrhythmia and even atrial fibrillation.
In difficult cases, in a specialized hospital, electrography of the atrionodal conduction system, surface ECG mapping (for topical diagnosis of rhythm disturbances) and other special research methods are performed.
Flow
A number of arrhythmias (isolated tachy- and bradycardia, rare intermittent monotopic extrasystoles, mild degrees of conduction disturbances, pacemaker migration) are usually not accompanied by organic cardiac pathology and distinct subjective manifestations and proceed quite favorably. Some forms of rhythm disturbances, especially persistent ones, can worsen the patient's condition, adversely affect hemodynamics, cause a decrease in cardiac output and impaired coronary circulation, and as a result lead to an unfavorable outcome. This is possible with ventricular and supraventricular tachycardia, frequent polytopic extrasystoles, significant slowing of heart rate, atrioventricular block, long Q-T interval syndrome (Romano-Ward syndrome).
In newborns and young children, rhythm disturbances can be asymptomatic or severe, with complications. In older children, the prognosis for arrhythmias is usually favorable, but persistent arrhythmias, especially severe forms, can also lead to an unfavorable outcome.
Treatment
Treatment of rhythm disturbances, especially life-threatening ones, is carried out strictly individually depending on their origin, form, duration, impact on the child’s well-being and the state of his hemodynamics. It is necessary to stop the arrhythmia and carry out maintenance therapy to prevent recurrence. For all types of arrhythmias, cardiac and extracardiac causes should be treated simultaneously.
- Basic therapy includes a course (at least 2-3 months) of nootropics [piracetam, pyritinol (for example, encephabol), gamma-aminobutyric acid (for example, aminolone), glutamic acid, phenibut, carbamazepine, hopantenic acid (for example, pantogam), nicotinoyl , gamma-aminobutyric acid (picamilon)] for the correction of neurovegetative disorders and normalization of trophic processes in the nervous system. The effectiveness of the use of cell membrane stabilizers and antioxidants [vitamins E and A, cytochrome C, vetoron, etidronic acid (xidifon)], agents that correct metabolic processes in the myocardium [vitamins C, B1, B2, B15, benfotiamine, potassium orotate, inosine ( for example, riboxin), levocarnitine, orotic acid, magnesium salt (magnerot)], as well as electrolyte imbalance [potassium and magnesium asparaginate (for example, asparkam, panangin), potassium chloride, calcium glycerophosphate]. In complex treatment, vasodilators [vinpocetine (for example, Cavinton), vincamine, pentoxifylline (for example, Trental)], angioprotectors [pyricarbate (parmidine)], bellataminal, and biogenic stimulants (tinctures of aralia, lemongrass, ginseng, zamanikha) are used. Consistent use of these drugs often helps to normalize the well-being of patients, eliminate arrhythmias or improve their tolerability. Fainting and palpitations require a special therapeutic approach, since they can be the result of not only severe rhythm disturbances, but also concomitant hemodynamic and other disorders.
- Antiarrhythmic drugs [procainamide (procainamide), amiodarone, lidocaine, verapamil, etc.] are used in children with certain restrictions due to the fact that they are not always quite effective and can cause adverse reactions (decreased blood pressure) much more often than in adults. pressure and contractility of the myocardium, worsening of arrhythmias, slower conduction). Their use is justified in cases of severe subjective intolerance to arrhythmias, significant hemodynamic changes, as well as in conditions with an unfavorable prognosis (paroxysmal tachycardia, frequent ventricular and supraventricular extrasystoles, atrial fibrillation). Attacks of paroxysmal tachycardia can be stopped by the administration of propranolol (for example, obsidan) or verapamil (for example, isoptin). Determination of indications for the use of antiarrhythmic drugs and their individual selection is carried out in the hospital.
- In case of conduction disturbances (isolated or accompanying other forms of arrhythmias), it is possible to use adrenomimetics [isoprenaline (isadrin), orciprenaline (for example, alupent), norepinephrine), atropine, as well as glucocorticoids (for high-degree atrioventricular blockades). Long QT syndrome requires long-term administration of beta-blockers.
- For some persistent, prognostically unfavorable, life-threatening rhythm disturbances (paroxysmal supraventricular and ventricular tachycardia, atrial fibrillation), cardiac defibrillation is indicated to restore sinus rhythm. In case of high degree atrioventricular blockade, and in some cases also in case of sick sinus syndrome, a pacemaker is implanted. Cardiac surgery may be indicated for patients with treatment-resistant chronic non-paroxysmal and paroxysmal supraventricular tachycardias and atrial fibrillation.
Dispensary observation
Clinical observation should be regular; its frequency is determined depending on the underlying disease (rheumatism, non-rheumatic carditis, congenital heart defects, autonomic dystonia syndrome, etc.), the form of arrhythmia and the characteristics of its course.
Dynamic ECG monitoring is required; 24-hour Holter monitoring and other studies are prescribed according to indications. They also monitor the implementation of medical prescriptions and the effectiveness of therapy. Clinical observation of children with arrhythmias has no time limits, and it is often continued until the patient is transferred under the supervision of an adolescent therapist. Children treated in a hospital are observed monthly in the first quarter, up to 1 year - at least once every 3 months, then - once every six months.
Prevention
Prevention of rhythm and conduction disorders is aimed at eliminating predisposing factors. In order to timely detect arrhythmias, it is advisable to conduct regular ECG monitoring, especially during periods of greatest risk of their development (in newborns, at 4-5, 7-8 and 12-13 years). Secondary prevention involves maintaining normal rhythmic activity of the heart and preventing the progression of arrhythmias and includes a complex of non-drug interventions (psychological correction, restorative measures, exercise therapy) and drug treatment (courses of nootropic, membrane-stabilizing drugs, antioxidants, etc.) depending on the characteristics of a particular case.
Forecast
Most arrhythmias in childhood are benign, reversible and do not affect the prognosis of life. However, in newborns and young children they can cause the development of arrhythmogenic cardiomyopathy or heart failure, which can lead to early disability and even death. Chronic non-paroxysmal and paroxysmal tachycardia, atrial fibrillation, and acquired complete transverse heart block have an unfavorable prognosis. Diseases associated with a high risk of sudden death (usually due to asystole or ventricular fibrillation) include long QT interval syndrome, severe dysfunction of the sinus node, some tachyarrhythmias, especially ventricular ones, accompanied by fainting, myocardial ischemia, acute heart failure, arterial hypertension.
Source: Children's diseases. Baranov A.A. // 2002. Illustrations from the site: © 2011 Thinkstock