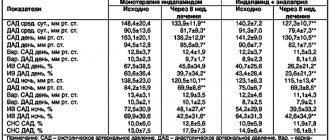
Currently, various electrocardiographic methods are used to identify patients at high risk of developing life-threatening arrhythmias: high-resolution ECG (HR ECG), heart rate variability (HRV) analysis, and Holter monitoring. The dynamics of the indicators of these methods have been quite well studied in the acute, subacute and long-term periods of myocardial infarction [1, 2].
Electrocardiographic markers of sudden cardiac death in myocardial ischemia have been studied to a lesser extent [3]. In this regard, attention is drawn to the data on the possibility of using assessment of changes in the duration and amplitude of the QRS complex during myocardial ischemia (stress test, acute coronary syndrome (ACS), chronic ischemic heart disease) according to HR ECG data [4–9] and analysis of heart rate variability [10]. In the literature available to us, we have not found sufficiently complete data on the dynamics of the amplitude and temporal characteristics of the QRS complex and HRV indicators in patients with ACS.
The purpose of this study was to study ECG parameters of HR and HRV in patients with ACS to assess the electrical instability of the myocardium and the severity of the disease.
A single cause of electrical instability of the conduction pathways in all structural and pathological diseases of the heart.
Khabchabov R.G.
Dagestan State Medical Academy, Department of Polyclinic Therapy, Cardiology and General Medical Practice, Makhachkala.
Khabchabov Rustam Gazimagomedovich, candidate of medical sciences. Address and work: Makhachkala, Lenin Square 1, ind. 367000. Dagestan State Medical Academy (DSMA), Department of Polyclinic Therapy, Cardiology and General Medical Practice. Tel, cell. 8963-413-67-20, house. 8(8722) 60-25-70, el. address
Summary
The cause of the development of life-threatening arrhythmias, which leads to sudden and overall mortality from cardiovascular diseases, still remains unclear; all cardiologists in the world are searching in this direction. Damage to the connective tissue insulating membrane of the conduction pathways of the heart can lead to atrial or ventricular flutter with the subsequent development of fibrillation; previously no one considered this cause as electrical instability of the heart.
Key words: electrical instability of the heart, flutter, flicker.
Cardiovascular diseases (CVDs) are the leading causes of disability and mortality among the working-age population worldwide. In Russia, the prevalence of CVD is growing, and our country is one of the first in the world in terms of mortality from them, which necessitates the need for doctors to search for modern and effective methods of their treatment and prevention.
After reading the article to the end, many will understand that in our lives, without realizing it, we have modeled an electrical system similar to our heart, in which there are power plants, conductive paths, electric generators, a transformer station, etc.
Many authors in ongoing studies on electrical instability of the heart (ECI) often focus their attention only on necrotic-scarring processes (NCP) in the myocardium in coronary heart disease (CHD). But patients with other CVDs are also susceptible to the development of general and sudden cardiac death (SCD). The authors for some reason ignore such diseases, meanwhile, it is obvious that the ENS is the same for all structural heart pathologies (SHR) and patients do not die from myocardial infarctions ( MI), but from lethal arrhythmias.
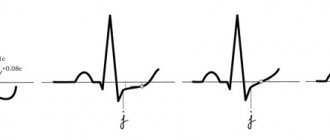
If we analyze all the arrhythmias, then they are well amenable to reason, but the reason for the development of flutter remains unclear, and the mechanism of flicker is confused, due to the presence of contradictions in electrocardiography (ECG) students.
At a young age, fluttering and flickering occur in patients with rheumatism, myocarditis, mitral heart defects, and in old age - most often with coronary heart disease, acute myocardial infarction, chronic heart failure, mitral stenosis, hypertension, cardiomyopathy, myocarditis, etc. . [9,10].
The determining condition for the occurrence of lethal arrhythmias is the presence of SPS, which turns into an unstable substrate under the influence of various functional factors. Such structural changes that predetermine the development of life-threatening arrhythmias (VAs) can include: pronounced hypertrophy, dilatation, cardiac aneurysm, necrotic and sclerotic processes of the myocardium, inflammation with edema of myocardial tissue, etc. These changes, according to many researchers, constitute the anatomical substrate with different mechanisms of VA occurrence [11].
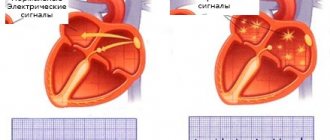
From the definition of ECG textbooks [9,10]: Atrial and ventricular flutter is the correct and rhythmic movement of a powerful excitation wave along the same path with the development of the re-entry mechanism (but what is the reason and how is such a macro-re-entry mechanism formed? , remained unclear to researchers at that time). Atrial and ventricular fibrillation is a disordered, chaotic excitation and contraction of individual groups of muscle fibers, each of which is actually a kind of ectopic source of impulse. After reading this definition and returning back to the chapter “function of automaticity”, you can read in it that the cells of the sinoatrial node (SU) and the conduction system of the heart have the function of automaticity: the atrioventricular (AV) connection, the conduction system of the atria and ventricles, and the contractile myocardium is devoid of function automaticity [9,10]. This suggests that with atrial fibrillation, “individual groups of muscle fibers” cannot generate and there is no “electrical instability of the myocardium”; the myocardium only conducts electrical impulses, but does not generate them, even if the myocardium or cardiomyocytes change their properties. Some may argue that the myocardium may be devoid of electrical activity, but there may be a zone of inhomogeneity in the myocardium after an MI that can interfere with the conduction of electricity; in fact, electrical impulses easily bypass such a zone, even with extensive NRP. At the same time, it can be assumed that there is multiple generation of ectopic foci (EF), which are located in the distal cardiac pathways (PPC), their power is weak, but they flicker well, like “garlands” on a Christmas tree and trigger the micro-re-entry mechanism. The myocardium really cannot ectopize on its own, since all ectopic nodes are located along the PPS, like beads on a string and have a single connective tissue insulating membrane (CTI), which starts from the SG. Without damage to this membrane, electrical impulses cannot reach the myocardium, and only Purkinje fibers do not have such a membrane, through which the myocardium is excited (not all textbooks indicate that there are Purkinje fibers in the atria).
First of all, it should be noted that the PPS are located in the same way as the electrical wires in the walls of our houses, they also have an insulating sheath, but in the wall the wires are not mobile and wear out little, and in the working myocardium with the presence of the PPS they can quickly become unusable , and their damage often occurs with the development of blockades or damage to only the STIO. It may also be interesting that in our homes there are peculiar Purkinje fibers - these are sockets, switches, etc., where the wires are exposed.
In many cases, with pronounced SPS, overstretching can occur with a rupture or tear of only the STIO of the main PPS (by the way, a similar mechanism is described in Alzheimer’s disease, when the myelin sheath of the nerve is damaged by atherosclerosis and nerve impulses are scattered into the surrounding tissue, is it possible that atherosclerotic damage to the PPS is also possible?) , which contributes to the activation of nearby EO. This leads to the fact that the electrical impulse coming out of the EO will pass through such damage along the least path of resistance (the electrical impulse will not branch into many small conducting paths and pass through the ectopic nodes located in them), it will break out into the myocardium with a powerful an electrical impulse (70-80% of the total electrical impulse, it is precisely this mechanism of flutter development that is described in ECG textbooks, but the reason for this phenomenon remains unclear to researchers), as a result of which large F flutter waves are formed. If this happens in the atria, then such a powerful electrical impulse will twist in the myocardium according to the type of macro-re-entry mechanism, and the AV node will not receive a full electrical impulse and only from 2-3, etc. ectopic excitation of the AV node will be able to transform a full-fledged electrical impulse for the ventricles. The longer the fluttering, the more the compensatory forces of the main EO decrease, and as soon as it weakens, many smaller EOs will be activated, which will lead to flickering.
One may ask why the STIO damage theory is correct? The fact is that the most powerful source of ectopia during supraventricular paroxysmal tachycardia and atrial flutter is in the atria (flickering does not count, it is caused by multiple ectopia), but the ECG shows a different picture, why? Because in the first case, the electrical impulse has to overcome obstacles, passing through many small pathways and ectopic nodes in the atria, and then it enters the myocardium with a not so powerful impulse in order to spin the macro-re-entry wave. And in the second case, it unhinderedly breaks out with a powerful electrical impulse onto the myocardium through the damage to the STI and spins a wave of macro-re-entry. This macro-re-entry mechanism gives a small difference in heart rate between supraventricular paroxysmal tachycardia and atrial flutter. In other words, paroxysmal tachycardia damages the STIO PPS and turns into flutter, but the source of ectopia remains the same, that is, it is the same type of arrhythmia, only with a different mechanism of action. The same mechanism for the development of ventricular flutter.
It should be noted that paroxysmal tachycardia generally leads to damage to the STI, although damage to the TIO itself can activate EO with the development of flutter, a clear example of this is the appearance of a necrotic zone during MI. With the development of acute MI, myocardial necrosis does not always damage the STIO of the main ventricular pathways, even with an extensive infarction, but if this occurs, EO may immediately become activated with the development of flutter and subsequent ventricular fibrillation.
Usually, only in two cases can arrhythmia develop (extrasystole, ventricular or paroxysmal tachycardia): 1. Super-powerful supply of electrical impulses to one of the ectopic nodes, which can also be facilitated by sympathetic stimulation of beta-adrenergic receptors. 2. On the contrary, the ultra-low power of electrical impulses, which can also be facilitated by the influence of parasympathetic innervation. That is, not only heart rate affects the development of arrhythmia, but also the current voltage in the conduction system. It looks like this: if your house receives insufficient or over-powerful frequency of electricity, then so that all your electrical equipment does not fail, you disconnect from the central networks and turn on your own electric generator. Extrasystole, ventricular and paroxysmal tachycardia are just trying to interrupt the unstable operation of the central generator (this effect can be called a protective mechanism of ectopic nodes from the unstable power of electrical impulses of the SG or conducting AV node). In some cases, the power of the triggered ectopic generator may become uncontrollable in supplying electrical impulses in the opposite direction, which leads to temporary or permanent deactivation of the sinus or AV node, and when the compensatory forces of the main EO are depleted, multiple ectopia (flicker) develops. The nervous regulation of the SG is more advanced due to the simultaneous participation of the sympathetic and parasympathetic divisions of the autonomic nervous system in it, which stabilizes the power of electrical impulses.
Additional factors in the development of arrhythmias with the presence of SPS may be: 1. Weakness of the proximal ectopic node (blockade I, II, III - type AV block), as a result of which weak electrical impulses arrive to the distal node and it is activated (that is, sometimes there is a syndrome weakness of the ectopic node). 2. Overstretching of the conduction pathways (especially in the locations of ectopic nodes) with pronounced hypertrophies, dilations, etc., leads to an increase in electrical conductivity, which also contributes to the delay of electrical impulses and activation of EO.
The triggering factor for damage to the STIO PPS in SPS can be any sudden movements or damage to the myocardium: all types of tachycardias and extrasystoles, a jump in blood pressure (BP), an increase in myocardial contractility (especially with pathologically reduced contractility), NRP, inflammation of myocardial tissue, etc.
According to localization, the thinnest and most easily damaged segments in the ventricles are the right leg and the anterior branch of the left leg. Next, in descending order according to their vulnerability, you can place the main trunk of the left leg, the bundle of His and, finally, the posterior branch of the left leg. However, conduction disturbances can occur in any segment or in several segments simultaneously [10]. Most likely, the Wenckebach, Bachmann and Thorel pathways are most often damaged in the atria.
In some cases, when performing electrical cardioversion, it is possible to interrupt atrial flutter or fibrillation at the initial stage (paroxysmal, persistent), while all generation centers are discharged, and the electrical stability of the heart can be restored with normal functioning of the systolic system. With the development of atrial flutter, it is possible to drug suppression of ectopic activity for 5-7 days with the transition of flutter to fibrillation, this will give time for favorable scarring of the connective tissue damage to the PPJ, after which an attempt can be made to restore the functioning of the AC. The prophylactic use of reparants in patients with SPS can help prevent damage to the STIO PPS; by the way, such reparants include; Potassium orotate, ATP and solcoseryl. Resuscitation measures using a defibrillator for ventricular flutter and fibrillation in patients with SPS are rarely successful. It is possible that the emergency use of a device, such as an artificial pacemaker and the presence of a probe in the form of a long insulating needle to a bare tip, which can be urgently inserted into the myocardium, through the intercostal space immediately after unsuccessful resuscitation measures, will allow the heart to work and restore blood circulation in vital organs, and In the future, a pacemaker can be installed. Additional resuscitation measures using such a pacemaker are good because in this situation there is nothing to lose, the patient is practically dead.
Next, we will analyze the literature with modern views of authors and researchers on the problem of ENS. First of all, it should be noted that many authors write about electrical instability of the myocardium, although it would be more correct to write “electrical instability of the heart.” Also, many authors try to fit the ENS to one structural-pathological heart disease and, most often, this is acute MI.
For the occurrence of life-threatening VA (sustained VT, VF), a combination of several causes predisposing to ENM is required: the presence of a substrate (structural heart disease) that modulates the dysfunction of the autonomic nervous system and triggering factors for VA. The morphological substrate that creates inhomogeneity of impulse conduction after MI is the myocardial zone bordering the necrotic tissue, formed from intertwined islands of viable myocardial fibers and connective tissue. In this place, the path of the impulse is lengthened due to the fact that the islands of connective tissue become barriers to the path of the excitation wave, and the conduction speed slows down as a result of a violation of the parallel orientation of the muscle fibers. Thus, myocardial zones with delayed ventricular depolarization may represent an anatomical and physiological substrate for re-entry, the main mechanism for the development of VA [1,4,22]. In this study, the author was close to the truth, but could not understand that the source of development of VA is not the border myocardium, but damage in this zone due to necrosis of the main PPS with the development of ventricular flutter.
As evidenced by the results of the work of JD Kramer et al., the presence of a long path of impulse rotation is not necessary; the presence of a small diameter of myocardial tissue that has changed its electrophysiological properties due to acute myocardial ischemia or the heterogeneity of its structure due to fibrous-necrotic changes is sufficient to trigger the mechanism of re- entry [17]. The fibers of the conduction system are more resistant to hypoxia and myocardial ischemia is unlikely to lead to the re-entry mechanism, and fibro-necrotic changes can damage the STIO PPS and trigger the macro-re-entry mechanism in the myocardium with the development of flutter.
According to modern concepts, the etiology and pathogenesis of VA in patients with coronary artery disease involves the interaction of many factors: structural changes in the heart [20], electrical instability of the myocardium, neurohumoral mechanisms [15], circadian biorhythms [12], and genetic defects [16].
Many noninvasive techniques have been proposed for risk stratification in patients with structural myocardial defects. Unfortunately, the capabilities of most of them are limited. An ejection fraction of less than 40% and non-sustained ventricular tachycardia (VT) during Holter monitoring and electrophysiological studies in patients who have suffered acute MI remain the main prognostic markers of high risk of SCD today [14]. A recent study in patients with implantable cardioverter defibrillators demonstrated that sudden onset of ventricular tachycardia or ventricular fibrillation (VF) typically occurs with preserved ejection fraction; with reduced contractility, before attacks of VT or VF, there is usually a gradual increase in ventricular ectopic activity. There is no doubt that the presence of heart failure is an important arrhythmogenic factor and a marker of the risk of sudden arrhythmic death in patients with coronary artery disease. The presence of a cardiac aneurysm, post-infarction scars and clinical manifestations of heart failure increases the likelihood of an unfavorable outcome. A decrease in left ventricular contractility increases the risk of SCD not only in patients with coronary artery disease, but also in patients with other heart diseases [13].
Another important risk factor for SCD in patients with coronary artery disease is myocardial ischemia. This disorder, as mentioned above, is the main cause of sudden SCD. Severe (more than 50%) atherosclerotic narrowing of the coronary arteries is detected in approximately 90% of sudden deaths [2]. The degree of coronary artery damage plays an important role in the development of VA and SCD [8]. A large number of clinical studies show that both symptomatic and silent myocardial ischemia are an informative marker of the risk of SCD in patients with various forms of coronary artery disease [19,27]. Myocardial ischemia, electrical instability and left ventricular dysfunction constitute the so-called risk triangle for sudden death in patients with coronary artery disease [18].
The combination of two risk factors for SCD is especially unfavorable: frequent ventricular extrasystole and left ventricular dysfunction with a decrease in ejection fraction <40%. According to the GISSI-2 study, the risk of sudden arrhythmic death in this case increases 16 times [3].
One of the risk factors for SCD is the presence of severe left ventricular hypertrophy, in particular in patients with arterial hypertension [24] and hypertrophic cardiomyopathy [28].
The discussion about the precursors of VF has been going on in the literature for quite a long time, however, there is no certainty here either. Currently used risk factors for the occurrence of VA in patients with coronary artery disease have insufficient sensitivity and specificity. This prompts the search for new markers of myocardial electrical instability [26].
In addition to these, other risk factors for sudden death are known, in particular, a violation of the autonomic regulation of the heart with a predominance of sympathetic activity. The most important marker of this condition is a decrease in heart rate variability (HRV) [21], as well as an increase in the duration and dispersion of the QT interval [25]. Decreased rhythm variability and prolongation of the QT interval are considered additional indicators of myocardial electrical instability [18].
Regarding HRV, QT interval dispersion and late ventricular potentials (LVPs), I can add a few of my final conclusions from my defended dissertation work. The initial deterioration of HRV indices in patients in the post-infarction period is due to the fact that they are in an anxious-depressive state after suffering an acute MI. Depression occurs in 82% of patients in the post-infarction period [7]. Such patients develop a fear of death and anxiety for their health, they are deprived of the emotions of a joyful perception of the world around them and become withdrawn, as a result of which the activity of the sympathetic nervous system (SNS) begins to predominate over the parasympathetic nervous system (PSN). As the positive psycho-emotional state of patients is activated, they begin to emerge from depression, and the work of the PSN also stabilizes, which leads to fluctuations in sinus rhythm. It should be noted that the psycho-emotional state of patients can be positive and negative at different times of the day. At any moment, the positive psycho-emotional state of a patient who has suffered an MI can change to a negative and even stressful state, and this will lead to hyperactivity of the SNS, which, in combination with atherosclerotic changes in the coronary arteries, can lead to their spasm and the appearance of new necrotic foci in the myocardium .
Not all researchers classify psycho-emotional states as traditional risk factors for coronary heart disease, although prolonged spasm of even intact coronary arteries due to activation of the SNS is the main mechanism for the development of angina attacks and myocardial infarction. Often such a spasm is associated with a negative psycho-emotional state of the patient, and this suggests that IHD is, first of all, a cardio-neurological disease. Proof of this is a decrease in HRV in the majority of patients with episodes of ischemia according to the results of 24-hour ECG monitoring (CMECG), which means that such patients require additional psycho-neurological treatment. Many SMECG devices have a HRV analysis program, but specialists more often issue a general daily conclusion, although they can be fragmented into 5-minute intervals and correlated with ischemic episodes. This will provide information to specialists about a sharp decrease in the digital values of HRV before the development of an ischemic episode, and distinguish between patients with an unstable nervous system. Such a correlation of HRV can also be carried out with the onset of arrhythmia development. Perhaps, when specialists begin to decipher HRV based on SMECG data in more detail, the role of this research method will become more noticeable in the diagnosis and treatment of IHD.
In the post-infarction period, PPV improves slightly than the QT interval dispersion indicators. This is probably due to the fact that the presence of PPV is more associated with the death of the conduction pathways of the heart (branches of the bundle branches or the main trunks of the Purkinje fibers), which are completely blocked by the inhomogeneous necrotic zone and subsequent cicatricial changes in the myocardium, as a result of which the electrical impulse has to return and exit through other pathways to the myocardium. Either the conduction pathways of the heart are not completely blocked by cicatricial changes in the myocardium, and then the electrical impulse has to break through partially inhomogeneous zones.
Unlike PPV, the slowdown in the recovery processes of the QT interval is less associated with pathological changes in the conduction pathways of the heart, and perhaps there is no such connection at all in 50% of patients who have had a MI (especially in patients with non-Q-MI). In the acute stage of MI, a slowdown in the dispersion of the QT interval is often associated with the presence of necrosis and the reinfarction zone of the myocardium, which has a larger area of inhomogeneity by 20-40% than in the scar period, which subsequently leads to an improvement in repolarization processes. It is possible that in those isolated cases when PPV indicators improve in the post-infarction period, there may be a connection between rare cases of the body’s ability to produce stem cells, as a result of which there is a partial growth of new cardiac pathways (branch of the His bundle branch or Purkinje fibers) bypassing the scar zone, which leads to the restoration of the conductivity of electrical impulses and the elimination of PPV.
Having already written the article, I read a lot of literature, including the anatomy and physiology of the heart, but nowhere did I find any mention of the presence of an insulating membrane of the main PPS. It is written about the existence of a small number of P-cells and Purkinje cells (atypical, specialized), which have an electrically conductive function, the majority of the myocardium - 99% are cardiomyocytes (typical, working) with a contractile function, and between them are T-cells (transitional). It is logically clear that all these cells and cardiomyocytes of the myocardium conduct electrical impulses and we are talking about Purkinje fibers, where the conductive system is exposed and does not have STIO. The literature writes about the existence of STIO of the sinus and AV nodes, and therefore, there must be an insulating membrane between the main conducting pathways and contractile cardiomyocytes, otherwise it is not clear why the main PPS are needed at all!
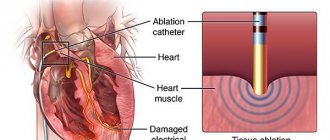
In conclusion, I note that at present, knowledge about the formation of the conduction system is far from complete, especially with regard to the formation of the conduction system. Progress in the study of additional pathways of impulse conduction is due only to ECG studies and is not evidence-based. To have a complete picture of all the features of the myocardium and the electrophysiology of the heart, you need to know that between the atria and ventricles there is a connective tissue framework that does not allow the ventricles to be excited along with the atria. In this frame there is a congenital opening defect (it is this defect that is cauterized during ablation), and not an additional conduction path (bundle of Kent), with an increase in pressure in the atrium or ventricle, and possibly in both of them, through this defect they begin periodically the ventricles become prematurely excited (WPW syndrome). In CLC syndrome, there is also no additional conduction pathway (James bundle), but there is a congenital periodic disturbance in the transformation of electrical impulses with accelerated conduction through the AV node. As a result of this, some electrical impulses pass through the AV node without transformation, and the PQ interval is shortened. Thus, it can be noted; 1. There are no additional conduction pathways between the atria and ventricles, and if they existed, then electrical impulses would pass through them constantly, from birth to death, since there are no valves in the conduction pathways, and these pre-excitation syndromes are intermittent. 2. The so-called additional conduction pathways of Kent, James and Mahaim are described as muscle bundles, but the entire myocardium is one large muscle, that is, many muscle bundles and why some of them became additional conduction pathways is not clear!
Literature
1. Buziashvili Y.I., Khananashvili E.M., Asymbekova E.U. et al. The relationship between myocardial viability and the presence of late ventricular potentials in patients who have suffered myocardial infarction. // Cardiology. - 2002. - No. 8. - P. 4-7.
2. Wichert A.M., Velishcheva L.S., Matova E.E. Geographical distribution and pathology of sudden death in the Soviet Union. In the book. Sudden death: Proceedings of the 1st Soviet-American Symposium. // Ed. A.M. Wicherta, B. Launa. - M.: Medicine. - 1980. - P.40-54.
3. Gilyarov M.Yu. Sulimov V.A. Treatment of cardiac arrhythmias in patients with circulatory failure. // Breast Cancer Cardiology. - 2010. - No. 22 (18). - pp. 1298-1301.
4. Grishaev S.L. Electrical instability of the myocardium in patients with coronary heart disease. // Russian medical journal. - 2003. - No. 2. - P. 13-18.
5. Murashko V.V., Strutynsky A.V. Electrocardiography: textbook. // 4th ed. - M.: MEDpress, 2000. - 312 p.
6. Orlov V.N. Guide to electrocardiography. // 4th era. ed.-M.: Medical Information Agency. - 2004. - 528 p.
7. Osadchy, K.K. Depression, anxiety and coronary heart disease: what does a cardiologist need to know? / K.K. Osadchiy // Cardiology. - 2009. - No. 5. - P. 70-77.
8. Savelyeva I.V. Stratification of patients with ventricular arrhythmias into sudden death groups. // Cardiology. - 1997. - No. 8. - P. 82-96.
9. Shalygin L.D., Lyadov K.V., Pyatkina T.V. Adequate antiarrhythmic chronotherapy for patients with ischemic heart disease. // 2001 conf. “Cardiology – XXI century”.
10. Bigger JT, Fleiss JL, Kjeiger R. et al. Therelationships among ventricular arrhythmias, left ventricular dysfunction and mortality in the 2 years after myocardial infarction. // Circulation. - 1984. - v.69. — R. 250.
11. Buxton AE, Kirk MM, Miehaud GT Current approaches to evaluation and management of patients with ventricular arrhythmias. // Med Health RI - 2001 Feb - 84(2). -R. 58-62.
12. Chen SW A wavelet-based heart rate variability analysis for the study of nonsustained ventricular tachycardia. // Trans Biomed Eng - 2002 Jul - No. 49(7). - R.736-742.
13. Elhendy A., Sozzi FB, van Domburg et al. Relation between exercise-induced ventricular arrhythmias and myocardial perfusion abnormalities in patients with intermediate pretest probability of coronary artery disease. // Eur J Nucl Med. — 2000 Mar — No. 27(3). - R. 327-332.
14. Gardner PI, Ursel PC, Fenoglio JJ et al. Electrophysiologic and anatomic basis for fractionated electrograms recorded from healed myocardial infarcts. // Circulation. - 1989. - No. 72. - R. 596-611.
15. Goldstein S., Bayes-de-Luna A., Gumdo-Soldevila J. Sudden cardiac death. // Armonk: Futura. - 1994. - 343 p.
16. Gottlieb LS, Weisfeldt M, Ouyang P et al. Silent ischemia as a marker for early unfavorable outcomes in patients with unstable angina. // New Engl. J. Med. - 1986. - v.314. — R. l214.
17. Kaasik A., Ristimae T., Soopold U. et al. The relationship between left ventricular mass and ventricular late potentials in patients with first myocardial infarction. // J Coronary Artery Disease. — 2001 Oct. — No. 4(1). R. 60.
18. Kleiger RE, Miller JP, Bigger JT et al.Decreased heart rate variability and its association with increased mortality after acute myocardial infarction. // Amer. J. CardioL. - 1987. - v.59. - R. 256 - 262.
19. Kulakowski P., Malik M. Ventricular signal averaged electrocardiography. Risk of Arrhythmia and Sudden Death ed. // London. - 2001. - R. 167-179.
20. Messerii FN Ventura HO Elizari DJ et al. Hypertension and sudden death, increased ventricular ectopic activity in left ventricular hypertrophy. // Amer. J. Med. - 1984. - v.77. - R. 18.
21. Morti V., Bayes-de-Luna A., Arriola J. et al. Value of dynamic QTc in arrhythmology. // New Trends Arrhyth. - 1988. - v.4. - R. 683.
22. Myeburg RJ, Spooner PM Opportunities for sudden death prevention: directions for new clinical and basic research. // Cardiovasc Res - 2001 May - No. 50(2). - R. 177-185.
23. Nademanee K, Intarachot V, Josephson M et al. Prognostic significance of silent myocardial ischemia in patients with unstable angina. // J. Amer. Coil. Cardiol. - 1987. - v.10. — R.1.
24. Nicod H., Polikar R., Petersoh KL Hypertrophic cardiomyopathy and sudden death. // new Engl. Med. - 1987. - v. 316. - P. 780.
25. Podrid Ph.J., Kowey PR Handbook of cardiac arrhythmia. // Baltimore, Williams & Wilkins. - 1996. - 459 p.
26. Priori SG, Barhanin J, NWHauer R, et al. Genetic and molecular basis of cardiac arrhythmias: impact on clinical management. // Circulation. — 1999 Feb 2. — No. 99(4). - R. 518-528.
27. Rocco MB, Nabel EG, Campbell S. et al. Prognostic significance of myocardial ischemia detected by ambulatory monitoring in patients with stable coronary artery disease.// Circulation. - 1988. - v.78. - R. 877.
28. Saeed M, Link MS, Mahapatra S et al. Analysis of intracardiac electrograms showing monomorphic ventricular tachycardia in patients with implantable cardioverter-defibrillators. // Am J Cardiol - 2000 Mar 1- No. 85(5). - R. 580-587.