Reticular (network) varicose veins are an enlargement of small intradermal and subcutaneous veins visible to the eye. The problem of reticular varicose veins is given considerable attention in modern phlebology. This is a “cosmetic” type of venous pathology, which is more often observed in women and is manifested by varicose dilation of small intradermal vessels and the appearance of telangiectasis on the lateral surface of the leg and less often along its inner part. Reticular varicose veins cause nothing but a cosmetic defect. Not dangerous, but not pleasing to the eye. The risk group consists of young women. After the first pregnancy and childbirth, a pathological process often develops in their intradermal vessels due to hormonal changes.
Causes
The causes of reticular varicose veins can be congenital. Sometimes it appears after long-term use of hormonal drugs. Visible affected vessels may appear after excessive physical activity, especially when walking in high heels. Reticular varicose veins of the lower extremities can also be a sign of chronic venous insufficiency and be accompanied by heaviness in the legs, swelling, and night cramps.
Reticular varicose veins are subcutaneous veins visible to the eye. They are larger than the capillaries on the vascular network, but smaller than varicose veins. The veins are approximately 1-3 mm in diameter, typically flat (do not protrude above the skin) and less twisted or convex than varicose veins, and often act as “feeder veins” for spider veins. They are usually blue or purple in color and are most often located on the legs, although they are sometimes found on other parts of the body, even on the face. Most often, reticular veins are a cosmetic problem rather than a health problem. This is because visible veins are small or moderate in size and do not cause medical symptoms or any complications in most patients. However, if their presence is accompanied by pain or discomfort, you should contact a specialist.
Varicose veins on the legs - symptoms and treatment
Taking into account modern treatment methods, the prognosis for varicose veins is favorable. Even in the most seemingly advanced cases, the elimination of varicose veins leads to a rapid improvement in the patient’s condition [8] [11].
However, when planning treatment, it is very important to assess its risks, since any intervention still carries potential adverse events. The direct responsibility of the doctor is to reduce their likelihood as much as possible. Before any manipulation, it is necessary to discuss with the patient all points regarding the intervention and obtain his signature on informed consent.
All adverse events can be divided into risks associated with surgery, including anesthesia, and risks on the part of the patient.
The risks of the operation may be small, for example, inflammation (phlebitis) in “welded” or sclerotic veins, accompanied by compaction in their projection and moderate pain. Areas of skin with reduced sensitivity and hyperpigmentation of the skin may appear. All these phenomena are temporary and, as a rule, pass quickly enough without any consequences [1].
Major complications include deep vein thrombosis, allergic and toxic reactions to anesthetic drugs. They are extremely rare, but for an individual patient who experiences such a complication, the case is 100 percent, even with statistics of 1 case per 10,000 operations.
Prevention of venous thrombosis is primarily based on calculating its risk using the so-called scoring system using the Caprini table. It contains various risk factors that have their own gradation. Taking into account each factor and obtaining a total score determines the degree of risk and, accordingly, its prevention. The main means of preventing venous thromboembolic complications are as follows:
- minimizing the trauma of the operation;
- early activation of the patient;
- compression jersey;
- pharmacological prevention, i.e., prescription of anticoagulants according to indications - blood thinning drugs (low molecular weight heparins or direct oral anticoagulants) [10].
Allergic and toxic reactions to the drug are, unfortunately, very difficult to predict. Testing for allergies to certain drugs does not prevent its occurrence and is not used in world practice. Therefore, it is extremely important to be prepared for the occurrence of these complications in any patient and to be able to provide immediate assistance. For this purpose, special equipment (first aid kits) with all necessary medications are always available in the operating room.
Risks from patients are usually associated with concomitant pathologies, for example, hypertension, coronary heart disease, epilepsy, etc. To prevent attacks of such diseases, a thorough medical history is taken and consultations with specialists are scheduled, who “give the go-ahead” for the operation.
As for the prevention of varicose veins, it simply does not exist, since the main cause of the pathology is still not clear, which could be influenced and thus prevent the occurrence of the disease. This is also associated with fairly frequent relapses of varicose veins after any type of intervention. However, given all the advantages of minimally invasive treatment, this is not a significant problem. Keeping your legs in order is quite simple, the main thing is to contact a phlebologist in time[3][5][6][10].
What causes reticular varicose veins?
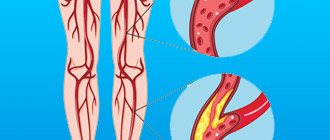
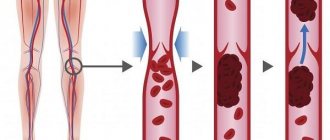
Vein dilatation occurs due to increased pressure in the skin vessels. The main causes of spider veins are the same as for spider veins and varicose veins: weak or damaged small venous valves. One-way valves in the veins prevent blood from flowing back. However, when the effectiveness of these valves and the elasticity of the vessel walls are impaired, this leads to backflow of blood and congestion of the reticular plexus. Blood returns to the intradermal veins (reflux) and causes the vessels on the surface of the skin to dilate, becoming visible.
Spider veins appear in the legs because the veins in the lower extremities must overcome gravity and withstand the most pressure to move blood back to the heart. A common cause of reticular varicose veins is a hereditary factor. If you have immediate family members who have spider veins or varicose veins, then there is a chance that you may also develop a similar problem.
Varicose veins are hereditary. Reticular varicose veins of the lower extremities can develop against the background of more serious venous lesions - varicose or post-thrombotic disease. Female hormones such as estrogen and progesterone can cause mesh formation. The most common uses of hormones are oral contraceptives (birth control pills), hormone replacement therapy, and fertility medications. Progesterone levels become very high during pregnancy. Progesterone relaxes the muscles in the walls of blood vessels, allowing them to stretch. For this reason, many women notice a large number of new visible blood vessels during pregnancy.
Experience of our specialists
Treatment of reticular varicose veins is the most painstaking work for a phlebologist. This procedure can only be entrusted to a very experienced specialist. The problem of treating reticular varicose veins of the lower extremities in our Center is dealt with by doctors Aleksey Viktorovich Beloglazov and Maxim Anatolyevich Karev. These are the most experienced aesthetic phlebologists in Moscow, who have successfully treated hundreds of women with cosmetic phlebological problems. In St. Petersburg, experienced phlebologist Astafieva Evgenia Valerievna deals with aesthetic phlebology; she uses the most modern method - transillumination sclerotherapy. The modern method of sclerotherapy is painless, cosmetic and safe. The principle of our phlebologists is to take on treatment and bring it to the best result.
Variants of intradermal varicose veins
Most often, reticular veins are visible as small blue vessels under the skin. They have small one-way valves, and when these valves stop working, the veins begin to dilate. Problematic vessels have poor blood flow and become twisted and distorted due to increased venous pressure, leading to the formation of red or purple spider veins. When dilated veins have a diameter of more than 3 mm and begin to bulge above the surface of the skin, they are called varicose veins. There are three types of varicose veins: linear (lines are formed on the surface of the skin), stellate (rays extend from a darker center, similar to a web or mesh) and tree-like (vessels have a branching appearance).
Symptoms
With cosmetic (aesthetic) varicose veins, patients' complaints are directed towards the presence of unaesthetic vascular networks, “worms”, “cobwebs”. In most cases, this causes psychological discomfort: women are embarrassed to undress on the beach, in the pool, or simply walk down the street in a short dress. In some cases, with the slightest blow, a hematoma immediately appears at the site of a superficial vessel, followed by the formation of a larger vascular network. In extreme cases, in the presence of reticular varicose veins, patients may feel a feeling of heat and baking at the end of the working day.
Absolute contraindications to sclerotherapy are:*
- Severe systemic diseases (for example, stage 3 hypertension)
- Thrombosis of deep and superficial veins
- Local or general infection
- In bedridden and sedentary patients
- Allergic diathesis
- Pregnancy and lactation
- Thrombophilic conditions (i.e., a violation of the properties of blood, accompanied by an increase in its coagulability)
- High obesity
- Impossibility of controlled intravascular injection (more common in obesity or “deep-lying” varicose veins)
* - based on the recommendations of the Meeting of Phlebology Experts in Moscow on June 16, 2000.
An example of sclerotherapy for spider veins is shown in the video below:
What is telangiectasia or spider veins?
Telangiectasia is a vascular formation, which is a persistent dilatation of skin vessels of small diameter (arterioles, venules, capillaries) of a non-inflammatory nature, morphologically manifested by spider veins or meshwork. The diameter of dilated vessels is 0.5-1.5 mm.
This is what spider veins on the legs look like
Surgery for the treatment of varicose veins
There are many methods of surgical treatment of varicose veins, the general essence of which boils down to the following: varicose veins are removed, incompetent perforating veins are blocked, which ultimately improves blood circulation in the limb. Surgical treatment of varicose veins is carried out in a hospital under general anesthesia or spinal anesthesia and requires a fairly long period of rehabilitation. Thanks to the advent of foam sclerotherapy (foam-form), the number of patients subject to surgical treatment is becoming smaller.
Learn about the differences and advantages of sclerotherapy and surgical treatment of varicose veins
Phlebotropic drugs
The action is designed to increase the tone of the venous wall, improve its properties (angioprotective effect), and improve the lymphatic drainage system of the limb. The most common drug currently used to treat varicose veins is Detralex.
Venoruton, troxevasin, ginkor-fort, aescusan, etc. are also used.
Compression jersey
Compression hosiery plays an important role in the treatment of varicose veins. The therapeutic effect of elastic compression is determined by the following mechanisms:
- Reducing the pathological capacity of altered veins due to their compression;
- Improving the functional properties of incompetent venous valves;
- Acceleration of venous blood flow due to narrowing of altered veins;
- An increase in the reabsorption of tissue fluid, resulting in a decrease in edema
- Improving the rheological properties of blood, which is the prevention of thrombosis;
Compression knitwear comes in the form of golf, stockings, and tights. It differs in the degree of “compression” according to functional classes (preventive, 1st, 2nd, 3rd, 4th). Currently, there are many manufacturers (Sigvaris, Medi, etc.), however, purchasing knitwear costs individual measurements and is not the cheapest. The degree of compression and type (stockings, golf, tights) are selected by the attending physician individually.
Therapeutic treatment
Vein sclerotherapy
- Cost: 6,500 rub.
- Duration: 20-60 minutes
- Hospitalization: No hospitalization required
More details
The selection of therapeutic treatment methods is carried out individually, taking into account the results of diagnostic studies. The most effective are:
- Laser sclerotherapy is a painless procedure that allows you to successfully combat the disease in the initial and middle stages of development. Requires three procedures with an interval of one month;
- Foam sclerotherapy involves the introduction of sclerosing substances into the vessels that block it. It is carried out in the presence of medium and large veins, lasts from five minutes to one hour depending on the size of the lesion;
- Microphlebectomy provides a good cosmetic effect and allows you to return to your normal lifestyle immediately after the procedure. It involves puncturing a vein with a special hook, pulling it out and ligating it.
All of the above treatment methods require wearing stockings with a compression effect during the rehabilitation period. This approach allows you to minimize the load on the veins of the legs, stimulates venous outflow and eliminates blood stagnation. It is important that the patient wears compression stockings exactly as scheduled, as this will affect the results of treatment.
Physiotherapy
Recommended for almost all forms and stages of varicose veins. Below is an example set of exercises:
| Initial position | Exercises | Number of repetitions |
| Lying on your back, the foot end of the couch is raised 20-25 cm + arms along the body, legs apart | Simultaneous flexion and extension of the feet and fingers | 10-12 |
| The same + legs straightened | Alternate flexion and extension of the legs at the knee joints | 3-6 times with each leg |
| Same | Bend your left leg, pull it to your chest, straighten it up, hold it and slowly lower it. Same with the right foot. | Same |
| Same + legs apart | Toes and knees in and out | 8-10 |
| The same + hands to shoulders | Circular movements in the shoulder joints | 4-5 times each way |
| The same + legs bent, hands on stomach | Tilts of bent legs to the right and left | 6-8 |
| The same + legs straightened | Alternate flexion and extension of the feet with reinforcement - “pressing the pedals” | 6-12 |
| Same + hands behind head | Bicycle leg movement | 6-8 movements 2-3 times |
| The same + legs bent, arms along the body | Alternately raise your legs up with a delay at the top - movements of the toes and active circular movements of the foot | Repeat 2-3 times |
| Lying on your left side, the foot end of the couch is lowered to a horizontal level, your left hand under your cheek, your right hand on your thigh, your legs are bent | Raise your right arm and leg up | 4-5 |
| Lying on your left side, hold onto the couch with your right hand | Swinging the right leg back and forth | 6-8 |
| The same Repeat the last 3 exercises lying on your right side | Flexion and extension of the feet | 8-12 |
| Standing facing the wall and holding onto the bar | Rise onto your toes, roll onto your heels and back onto your toes. | 5-6 |
Correction of work and rest regime for varicose veins
Basic recommendations on lifestyle, work and rest for patients suffering from varicose veins are as follows:
Harmful:
- stand or sit for a long time
- visiting a bathhouse, sauna
- prolonged exposure to the sun
- football, basketball, tennis, alpine skiing, volleyball, martial arts
- lifting weights
- tight underwear, corsets
- use of hormonal contraceptives
- overweight
- salt, spicy seasonings, fried foods, excess fluid intake, strong coffee, smoking
Healthy:
- walk, incl. climb stairs
- contrast shower on feet
- swimming
- skiing, cycling (in combination with elastic compression)
- vegetables, fruits, herbs and other foods rich in vitamin C
Prevention
One of the features of reticular varicose veins is that the development of the disease (primary or after a course of treatment) can be prevented. To do this you need:
- do light physical exercises daily, putting moderate stress on the lower limbs;
- when working for long periods of time sitting or standing, take short breaks and take a walk every hour;
- give up high heels and give preference to shoes with a wide last;
- control body weight, establish proper nutrition, give up bad habits.
To summarize, we note that reticular varicose veins, although not a critically dangerous disease, requires timely and professional treatment. An integrated approach and care for your feet will save you from possible complications and the development of more serious diseases.
There are several classifications of varicose veins of the lower extremities
In Russia, the classification proposed in 2000 at a meeting of leading phlebologists in Moscow is most often used.
Stage 1 - intradermal, subcutaneous and segmental varicose veins without pathological veno-venous discharge (in other words, when there are small varicose veins, but the valves of large saphenous and deep veins retain their function and allow blood to pass in the right direction, i.e. there is no pathological discharge of blood) .
Stage 2 – segmental varicose veins with reflux along the superficial or perforating veins (i.e. there are small saphenous varicose veins, the valves of the main saphenous veins or perforating veins (veins connecting the superficial veins with the deep ones) are incompetent).
Stage 3 – widespread varicose veins with reflux along the superficial and perforating veins.
Stage 4 – in addition to all the changes described above, insufficiency of the deep vein valves is also added.
Abroad, the CEAP classification, proposed by experts of the international conciliation group in 1994, is mainly used. This classification is gaining increasing popularity in Russia. For the work of a clinician, the clinical (C) section of this classification is most appropriate. According to the CEAP classification, there are 6 C-classes (stages) of the disease.
CLASS 1 – HEAVY LEGS SYNDROME, VASCULAR “STARS”
CLASS 2 – PRESENCE OF SUBSCUTANEOUS VARICOSE VEINS WITH TRANSIENT EDEMA.
3 CLASS – PERSISTENT EDEMA.
CLASS 4 – TROPHIC DISORDERS (ITCHING, PIGMENTATION, DERMATITIS, ECZEMA)
CLASS 5 – HEALED TROPHIC ULCER
CLASS 6 – OPEN TROPHIC ULCER.
The remaining classes of the CEAP classification (E - etiological, A - anatomical, P - pathophysiological) do not have much practical significance and are used more in scientific research.