- What is atherosclerosis of the lower extremity vessels?
- Symptoms of the disease
- Risk factors
- Stages of development of atherosclerosis of the lower extremities
- Diagnostics
- Treatment
- Conservative treatment
- Surgical techniques
- Possible consequences and prevention
- Popular questions
Obliterating atherosclerosis (OA) of the arteries of the lower extremities
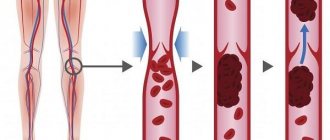
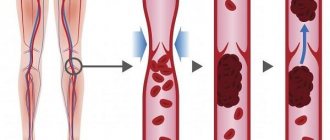
is a chronic vascular disease, which is based on lipid metabolism disorders, leading to the formation of atherosclerotic plaques, thickening of arterial walls and a decrease in the vascular lumen. As a result, ischemia develops - insufficient oxygen supply to cells and tissues.
Most often the popliteal, femoral and tibial arteries are involved in the pathological process.
OA of the arteries of the lower extremities is in first place among diseases of the peripheral arteries of atherosclerotic origin. According to literature data, obliterating arterial diseases account for about 16% of all vascular diseases Source: Podrezenko E.S. The influence of risk factors on the development of obliterating atherosclerosis of the vessels of the lower extremities / E.S. Podrezenko, S.S. Dunaevskaya // Health is the basis of human potential: problems and ways to solve them. - 2012. - pp. 576-578. .
Symptoms of atherosclerosis of leg vessels
The development of the disease occurs gradually and in the first stages there may be nothing to show for it. Subsequently, the patient develops pain in the lower extremities, especially with prolonged walking, and a feeling of numbness in the feet. A decrease in temperature is felt on the legs, pallor and cyanosis are visible, and cramps occur. Over time, a person develops intermittent claudication and trophic changes occur in the form of delamination of nails and the formation of ulcers on the fingers and heels.
- with atherosclerosis, the patient may feel and observe the following:
- muscle pain in the legs, in the later stages even the feet hurt, and the pain cannot be relieved with painkillers;
- limited mobility of the affected leg;
- pain along the affected artery - first during physical activity, then at rest;
- intermittent claudication - after walking some distance, a person is forced to stand up and give his legs a rest, and then he moves on until the next attack of weakness;
- tingling, numbness in the affected area;
- thickening of nails;
- loss or slow growth of hair on the legs;
- paleness when raising the legs and sharp redness when lowering them;
- rapid freezing of feet;
- sores on the skin;
- purple fingers;
- absence of pulsation in the affected artery;
- areas of darkening on the skin are signs of the onset of gangrene in advanced stages;
- coldness of the skin of the leg;
- reduction in the mass and volume of the muscles of the thighs and legs.
At the beginning of the disease, as a rule, one limb suffers, then the process becomes symmetrical - this is a signal that the arteries are affected on both sides. An objective examination reveals the absence of pulsation in the popliteal fossa, thigh and ankle.
Difference between stenosing and non-stenosing atherosclerosis
Atherosclerosis is a chronic vascular disease that develops with age, and all people are susceptible to it. At the initial stage, the plaques in the vessels are small, but if they do not block the vessel by more than half, this condition is called non-stenotic atherosclerosis. In this case, there are simply no signs of atherosclerosis, and the person feels great. As the cholesterol plaque grows, the vascular lumen becomes blocked—arterial stenosis occurs. In this case, organs deprived of the usual amount of oxygen and nutrients suffer from ischemia. This explains why the diagnosis of “stenotic atherosclerosis” occurs mainly in older and elderly people.
Risk factors
The development of OA is based on the following most significant risk factors, the degree of influence of which can be different Sources: 1. Kuznetsov M.R. Basic principles of diagnosis and treatment of obliterating atherosclerosis of the arteries of the lower extremities / M.R. Kuznetsov // General medicine. - 2008. - No. 1. - P. 3-8. 2. Podrezenko E.S. The influence of risk factors on the development of obliterating atherosclerosis of the vessels of the lower extremities / E.S. Podrezenko, S.S. Dunaevskaya // Health is the basis of human potential: problems and ways to solve them. - 2012. - pp. 576-578. 3. Fattakhov V.V. Obliterating atherosclerosis of the lower extremities in the practice of a polyclinic surgeon / V.V. Fattakhov // Practical medicine. - 2010. - No. 2 (41). — P. 126-130. :
- male gender (men get sick 10 times more often);
- age (over 40 years);
- poor nutrition;
- overweight (obesity);
- smoking tobacco;
- hypokinesia (insufficient motor activity);
- hypofunction of the thyroid and gonads;
- heredity;
- some concomitant diseases (diabetes mellitus, coronary heart disease, heart rhythm disorders, lipid and carbohydrate metabolism, hypertension);
- exposure to adverse environmental factors.
Causes and factors for the development of pathology
The most common cause of the disease is atherosclerosis. It is a long-term pathological process during which the vessel wall becomes rigid and cholesterol plaques are deposited in it, which are sources of local inflammation.
These formations narrow the lumen of the vessel, blocking the access of oxygenated blood to the tissues. They are the culprits of thrombosis, which threatens not only the affected limb, but also all organs of the body.
Other causes of obliterating atherosclerosis:
- Diabetes. High blood sugar damages the arterial wall, promoting the formation of blood clots. Such patients often have impaired lipid metabolism and increased blood pressure.
- Inflammation of blood vessels. This condition is called arteritis, or vasculitis. The cause is the body's autoimmune reactions.
- Infections such as salmonellosis and syphilis.
- Structural defects (vascular pathologies that arose during prenatal development).
Risk factors that increase the likelihood of developing the disease:
- several cases of death from myocardial infarction or stroke in the family;
- age over 50 years;
- excess weight;
- inactive lifestyle;
- smoking;
- diabetes;
- arterial hypertension;
- lipid metabolism disorders;
Stages of development of atherosclerosis of the lower extremities
The most detailed is the modified classification of chronic arterial insufficiency of the lower extremities (CANF), which takes into account in detail the phenomena of critical limb ischemia, which is necessary when determining treatment tactics.
| Stage 1 | Muscle pain only during heavy physical activity (when walking over a distance of more than 1 km). Initial signs of stenosis appear - the skin turns pale, there is a feeling of goosebumps, it seems that the legs are always cold, fatigue quickly sets in when walking, excessive sweating is observed |
| Stage 2A | Feeling of fatigue and stiffness in the calf muscles, intermittent claudication after 200-1000 m |
| Stage 2B | Intermittent claudication in less than 200 m |
| Stage 3A | Intermittent claudication after a few steps or pain at rest when it is possible to keep the lower limb in a horizontal position for more than 2 hours |
| Stage 3B | Pain at rest, ischemic edema, inability to keep the lower limb in a horizontal position for 2 hours |
| Stage 4A | Gangrene of the fingers or part of the foot with the prospect of maintaining the supporting function of the limb |
| Stage 4B | Extensive necrotic changes in the limb without the possibility of maintaining its supporting function |
Recovery and rehabilitation of the patient
The prognosis for a patient’s life is largely determined by preventive measures after radical intervention: medical check-up (screening), regular medications, and physical activity contribute to the speedy restoration of lower limb functions.
Dosed walking: what is the duration and intensity?
All patients require a special rehabilitation program with physical therapy. The most effective method is considered to be measured walking (on a treadmill - treadmill).
Basic principles of purpose:
initial duration - 35 minutes, gradually increasing to 60 minutes;- exercise 2-3 times a week;
- the intensity is determined individually at the load level, which causes lameness within 3-4 minutes;
- with a gradual improvement in the quality of walking - increase the intensity due to the speed rather than the duration of the workout.
It is recommended to start classes while staying in a sanatorium under the supervision of a doctor. If you experience shortness of breath or chest pain, consult a specialist.
Diagnostics
There is a standard diagnostic program for this disease:
- Ultrasound of vessels of the lower extremities (duplex and Doppler scanning);
- coagulogram (determination of the blood coagulation system);
- determination of cholesterol and LDL levels in the blood;
- leg arteriography;
- establishment of pulsation in peripheral arteries;
- MR, MSCT angiography.
If prescribed by a doctor, MRI and CT scans with contrast and rheovasography can be performed.
To make a timely diagnosis of atherosclerosis of the vessels of the lower extremities, consultation with a vascular surgeon or phlebologist and a number of diagnostic measures are necessary.
Due to the systemic nature of the atherosclerotic process, patients with OA of the lower extremities often experience combined damage to various arterial basins, therefore, in such patients, an integral part of instrumental diagnosis is the study of extracranial and coronary arteries. Identification of pathology in them may require a change in treatment tactics or the order of surgical interventions Source: Kuznetsov M.R. Basic principles of diagnosis and treatment of obliterating atherosclerosis of the arteries of the lower extremities / M.R. Kuznetsov // General medicine. - 2008. - No. 1. - P. 3-8. .
What it is
The pathology is associated with the development of a degenerative process in the peripheral arteries supplying the lower extremities.
This is one of the most common types of atherosclerosis - deposits of cholesterol and calcium salts on the walls of blood vessels and the formation of numerous plaques that sharply impede blood flow. Narrowing of the lumen of the arteries and poor circulation in the lower extremities leads to severe pain when walking and numbness of the feet. This syndrome is called intermittent claudication. As the pathology progresses, the pain becomes constant, and trophic ulcers and necrotic areas appear on the skin in the foot area.
The main problem in the treatment of obliterating atherosclerosis is associated with late seeking medical help, when pathological changes in blood vessels are irreversible.
Obliterating atherosclerosis often begins at a young age, but occurs without any symptoms. With age, clinical manifestations gradually become more pronounced, and if in people aged 50 years the pathology is diagnosed in only 1.1% of the population, then by the age of 70 this figure increases to 5.2%.
In older people, the disease usually occurs against the background of other chronic pathologies and damage to several arterial basins by atherosclerotic plaques. The disease is especially severe in patients with diabetes.
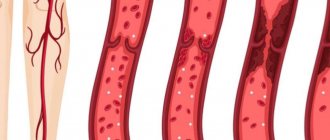
The pathological process in obliterating atherosclerosis affects the inner layer of blood vessels, consisting of a layer of endothelial cells - the intima. Around the fatty deposits on the vessel wall, connective tissue begins to grow and fibrous plaques form, to which platelets “stick.” Next, calcium salts begin to deposit on the affected tissues, creating a serious obstacle to blood flow.
The pathology is life-threatening to the patient: if you do not consult a doctor in a timely manner and if it lasts for a long time, the risk of high limb amputation increases. Every fourth patient dies after amputation, and half of the patients die in the first year after diagnosis, even if amputation was not performed. Narrowing of the arteries and prolonged stagnation of blood in the vessels of the lower extremities threatens the formation of blood clots, the development of gangrene and sepsis.
Treatment of atherosclerosis of the vessels of the lower extremities
The approach to treatment is determined depending on the stage of the disease and is primarily about choosing the right regimen. It is necessary to adhere to a diet limiting fried and fatty foods, eliminating smoking and alcohol, as well as combating excess weight. The patient should follow a walking and physical activity regimen, choose comfortable and spacious shoes, and treat even the smallest injuries on the skin of the lower extremities. Treatment of concomitant chronic diseases is mandatory.
Medicinal methods include anticoagulants, antiplatelet drugs, agents that improve blood microcirculation, vasodilators, and physiotherapeutic procedures.
In severe cases, surgical treatment may be necessary.
General recommendations:
- normalize weight;
- follow a diet with low cholesterol;
- give up alcohol and smoking;
- wear shoes that fit;
- do not overcool your feet;
- even minor injuries should be carefully treated and treated;
- trim nails carefully without damaging soft tissues;
- engage in moderate physical activity - walking, swimming, cycling or exercising on an exercise bike.
Diagnostic measures
The presence of a specific pathology, as well as its exact cause, can only be determined during a face-to-face consultation with a specialist. During it, the doctor will ask several general questions regarding lifestyle and chronic diseases, study the medical history in detail, conduct some functional tests, and clarify the presence of similar pathologies in close relatives. As part of the examination, the doctor will ask you about the frequency and intensity of your symptoms, monitor your clinical picture, and identify the suspected etiology of the disease.
If suspicions are partially confirmed, you will be prescribed simple tests:
Rheovasography (RVG) is a non-invasive functional method for assessing pulse blood supply to the extremities, as well as the tone, elasticity and patency of peripheral vessels using a specific device;
Measurement of the brachial-ankle index - a one-time determination of the level of blood pressure in the area of the shoulders and ankles (normally it is the same);
Biochemical blood test (cholesterol content), and other tests to detect cardiac dysfunction.
For a more in-depth study of the course of the disease, the following measures are taken:
1. Duplex scanning of arteries and veins;
2. Angiography using a contrast agent;
3. Magnetic resonance angiography;
4. Multislice computed tomography of the lower extremities;
5. Functional tests.
Treating atherosclerosis
- Shishkin A.A.
- Volkov A.M.
- Kabirov A.V.
- Baranov V.S.
Shishkin Andrey Andreevich
Candidate of Medical Sciences. Surgeon, proctologist, phlebologist at SM-Clinic. Proficient in all modern methods of conservative and surgical treatment of diseases of the veins of the lower extremities (including sclerotherapy, EVLT - endovasal laser coagulation, traditional phlebectomy)
Read moreVolkov Anton Maksimovich
Phlebologist, surgeon at SM-Clinic. Performs operations with a modern proprietary method of treating varicose veins using a laser (modified endovenous laser coagulation. M-EVLC).
Surgical treatment of varicose veins of any complexity (phlebectomy, miniphlebectomy) More detailsKabirov Alexander Vitalievich
Cardiovascular surgeon at SM-Clinic. Candidate of Medical Sciences Proficient in all modern methods of conservative and surgical treatment of diseases of the veins of the lower extremities (including sclerotherapy, EVLT - endovasal laser coagulation, traditional phlebectomy)
More detailsBaranov Vladimir Sergeevich
Cardiovascular surgeon at SM-Clinic. Candidate of Medical Sciences Treats lower varicose veins using non-surgical and surgical methods (aesthetic sclerotherapy, ECHO sclerotherapy, stem sclerotherapy, phlebectomy, miniphlebectomy, EVLT).
More details
Conservative treatment
The patient may be prescribed various medications:
- prevent the formation of blood clots, prevent stroke and heart attack;
- increasing physical activity, improving blood flow in the lower extremities;
- antiplatelet drugs that lower blood cholesterol levels;
- anticoagulants, which prevent blood clotting in blood vessels and prevent blood clots;
- antispasmodics to relieve pain and spasms;
- antimicrobial ointments that need to be used to treat trophic ulcers;
- medications that promote better tissue nutrition;
- vasodilators;
- vitamins.
Also, as part of conservative therapy, physiotherapy is performed - electrophoresis with novocaine, darsonvalization, hyperbaric oxygenation.
Surgical techniques
Surgery is a last resort and is usually prescribed for severe ischemia and very severe complications. Nowadays, different types of surgical interventions are performed. Some involve a day hospital, some require a long-term hospital stay under observation. Patient rehabilitation plans and post-operative care vary. Our doctors advise patients in detail on all aspects related to surgical intervention and carefully monitor their health in the pre- and postoperative period.
Surgical treatment of atherosclerosis of the lower extremities:
- bypass surgery - an additional “bypass” path for blood flow is created around the area of narrowing of the artery;
- stenting - a special tubular spacer is placed in the affected vessel, which ensures the required diameter of the artery;
- balloon angioplasty - similar to stenting, only a balloon is inserted into the vessel cavity rather than a spacer, which expands its lumen;
- autodermoplasty - if trophic ulcers are poorly treated conservatively, they are operated on and covered with the patient’s own skin;
- endarterectomy - removal of the affected part of the artery in which the atherosclerotic plaque is located;
- prosthetics – replacement of the affected vessel with the patient’s own vein, taken from another place, or with a synthetic prosthesis;
- amputation - prescribed in severe cases when gangrene occurs, after which prosthetics are performed.
In 75-85% of cases, after surgery, blood circulation is completely restored for an average of 5-8 years.
Indications for surgery:
- an aneurysm that may rupture;
- chronic ischemia of critical stage;
- hemodynamically significant carotid artery stenosis or plaque accompanied by symptoms of cerebral ischemia;
- decompensation of blood circulation in the leg due to embolism, trauma, thrombosis.
Contraindications to surgical treatment:
- wet gangrene with sepsis;
- severe disruption of vital organs - renal and liver failure, circulatory disorders in the brain, myocardial infarction, heart failure, etc.
Classification and course of the disease
An atherosclerotic plaque consists of cholesterol deposits and is covered with a fibrous layer of tissue. The core gradually grows, filling with contents and blocking the lumen of medium and large arteries, up to complete occlusion. If fat breaks into the bloodstream, rapid deposition of platelets and fibrin occurs on the plaque bed. This is how a blood clot forms.
Emboli have a different origin, being particles of a tumor or warty masses on infected heart valves. Sometimes they form if there are barriers to the physiological flow of blood: aortic aneurysm, congenital and acquired heart defects.
When thrombosis, embolism or injury occurs, the disease begins to manifest itself acutely. The location of circulatory arrest and the presence of additional vessels (collaterals) determine the severity of symptoms and the development of complications.
There are 4 stages of the disease:
- I. Pain increases with heavy loads and during long walking (more than 1000 meters).
- Stage II:
- A: pain begins when walking from 250 to 1000 m;
- B: when walking from 50 to 250 m.
- Stage of critical ischemia. Pain syndrome occurs with complete calm and during sleep.
- Stage of dystrophic disorders. Necrosis is found on the heels and toes, which tends to develop into gangrene .
Possible risks associated with the disease
The disease is insidious in that it is impossible to predict its course and symptoms. Approximately 20% of patients over 65 years of age, having severe plaques, do not feel any discomfort. The seriousness of the progressive course of OA ANC is also due to the fact that after the appearance of the first symptoms, 10-40% of patients develop gangrene within 3-5 years, which leads to amputation of a limb or death Source: Kazantsev A.V. A new approach to surgical tactics for obliterating atherosclerosis of the arteries of the lower extremities / A.V. Kazantsev, E.A. Korymasov // Saratov Medical Scientific Journal. - 2010. - T. 6. - No. 4. - P. 850-856. .
Atherosclerosis can be complicated by arterial thrombosis. This complication, if not immediately sought by a doctor, leads to loss of a limb or embolism of other arteries. If the clot detaches and enters the coronary artery, a myocardial infarction may develop, and if it migrates to the carotid artery, a stroke may occur.
Prevention methods
For prevention purposes, you need to start controlling the levels of lipids, sugar and cholesterol in the blood as early as possible. Even with a slight increase in numbers relative to the norm, you should consult a doctor. It is also recommended to regularly do ultrasound of the lower extremities - once every 1-2 years.
It is important to watch your diet, because the reason for the increase in “bad” cholesterol in the blood is the saturated fats that we consume in food. These are products of animal origin - fatty meat, lard, butter. There is a lot of cholesterol in eggs, or rather in the yolks. All these products should be consumed in the smallest possible quantities.
| Name of service (price list incomplete) | Price, rub.) | In installments* |
| Appointment (examination, consultation) with a cardiovascular surgeon, primary, therapeutic and diagnostic, outpatient | 1 750 | — |
| Program “Risk of atherosclerosis and ischemic heart disease, predisposition to dyslipidemia” | 19 000 | — |
* You can read more about the conditions here - Treatment on credit or in installments.