What is hyperechogenicity in the fetal heart?
A hyperechoic focus of the fetal heart implies the presence of a compaction in the structure of the heart muscle.
As a result, ultrasonic waves are reflected to a greater extent from the myocardial area and produce a bright spot on the screen. The inclusion, as a rule, has a diameter of 2-3 millimeters. Most often it is found in women over 35 years of age at 18-22 weeks of pregnancy. The phenomenon is most typical for representatives of Asian countries. On the European continent, this phenomenon occurs much less frequently (in 7-10% of cases). Usually the lump disappears by the end of the third trimester, but often remains until childbirth.
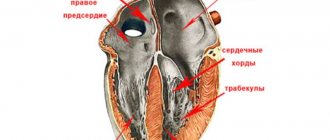
Most often, a hyperechoic inclusion is found in the left ventricle of the fetal heart, however, it can also be visualized in other parts of the organ. The presence of increased echogenicity in the right parts is considered more dangerous.
This phenomenon can be considered pathological only in cases where it accompanies other signs of congenital diseases. It is also important to remember that this is just a diagnostic sign, which is not an independent pathology and does not carry any negative consequences in the future.
Carrying out echocardioscopy
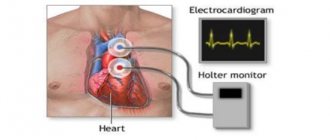
If GEF is detected in a child and there are certain indications, the patient is referred for fetal echocardioscopy.
Abnormal cardiac image abnormal heart rhythm palpitation defect defect other mucus instrument increased nodular translucency abnormal urinary flow abnormal amniotic fluid volume. Congenital heart defect Diabetes preeclampsia Phenylketonuria Systemic lymphadenopathy. Increased transventricular abnormalities, cardiac arrhythmias, abnormal arteries of the heart, other abnormalities in the abdomen. Miscarriage Miscarriage during pregnancy Several pregnancies. . According to various sources, hypergenic lesions occur in the range of ± 2-5% in all healthy fats in the second trimester of pregnancy.
Indications for echocardioscopy:
- first pregnancy in women over 35 years of age;
- diabetes;
- infectious disease of the expectant mother;
- identified pathologies in the structure of the heart;
- the child is developmentally delayed;
- relatives of a pregnant woman suffer from heart defects;
- Markers of genetic diseases have been discovered.
Echocardioscopy is performed until the 28th week of pregnancy, after which the method becomes uninformative due to the large size of the fetus and the small amount of amniotic fluid.
Many publications and web pages report that hyperechoic flashes are more common in men with abnormal chromosomes. During each test, the doctor accurately assesses fetal development, including the structure and function of the heart. Ultrasound illustrates the amount of cardiac cavity, valve function, and proper blood flow and contractility of the heart.
Only an experienced specialist can do this, who can accurately assess the structure and functioning of the child’s heart. After about 30 weeks, the light tissue is better developed, the pelvic fins are more calcified, the distance from the heart is greater - all of these factors cause the image of the heart to become less noticeable.
The study is used to assess the size of the valves and cavities of the heart, its contractility and the level of blood filling.
Causes
The source of hyperechoic inclusion of the fetal heart may be the deposition of calcium salts in the papillary muscles of the left ventricle. During this period, significant activation of mineral metabolism and intensive formation of the skeletal system occur. Over time, the salt is absorbed into the blood and the seal disappears.
In some cases, a similar symptom is caused by the presence of an additional chord. This is a connective tissue thread that runs from the heart valves to the papillary (papillary) muscles. Most often, each muscle corresponds to one thread, but in this case several of them are formed.
As blood passes through the chordae, turbulence will occur, which can produce a heart murmur heard on auscultation. This should be remembered, because in the future, due to the presence of this phenomenon, the pediatrician may make an incorrect diagnosis. Despite the fact that this phenomenon is considered an abnormality of the heart, this development option is accepted as normal.
Detection of an additional chord does not require further examination and treatment. As a rule, they grow together before birth or in the first years of life.
Previously, it was believed that LVEF was a clear sign of Down syndrome or other chromosomal diseases. But in recent years, many scientific works have appeared, thanks to which we now know that this is true only in the presence of additional symptoms. The detection of this sign alone is not a cause for concern and no further examination is required.
Normal indicators during echocardioscopy
During the examination, all cavities of the heart are measured. Normally, these indicators should be within the limits:
- length of the right ventricle - 0.5-1.75 cm;
- width of the right ventricle - 0.4-1.1 cm;
- length of the left ventricle - 0.9-1.8 cm;
- width of the left ventricle - 0.44-0.89 cm;
- ratio of the width of the left ventricle to the right - 0.45-0.9 cm;
- aortic mouth - 0.3-0.52 cm;
- pulmonary artery mouth - 0.3-0.5 cm;
- mitral orifice - 0.35-0.6 cm;
- tricuspid foramen - 0.3-0.63 cm;
- number of heart contractions - 140-160 beats/minute.
Gastrointestinal disorders. Skeletal dysplasia Kidney breeds. Rhythm disturbances and coarctation of the pulmonary aorta. Echo-morphology and chromosomal diseases. There is no nasal hypoplasia. Systematic morphological ultrasound examination. Standard abbreviations for fetal biometric assessment.
Sectional plane through the integration of the portal system with the umbilical vein. The diaphysis does not include the cartilaginous reflex. The distal epiphyseal. Standard abbreviations for assessing fetal appliances. Location and connection with the cervix. Factors influencing indicators of malformation development Assessment methodology - organization. Patient- and fetal-specific technical factors. Abnormal factors. Factors, level of ultrasound training and experience.
The size of the fetal heart has its own indicators and differs significantly from the size of an adult, since all organs correspond to the size of the body. Heart pathology is always detected during such an examination, so you should not worry about the unprofessionalism of the uzist if the diagnosis is not confirmed or the doctor says that this does not pose a threat to the child.
Echocardiographic diagnosis of primary cardiac tumors in the fetus. Echocardiographic diagnosis of primary fetal heart tumors. Pediatric cardio. National Center for Medical Genetics. Associate Professor of the Department of Pediatrics. Six cardiac tumors were identified, representing 0.3% of the cases examined. Five were consistent with rhabdomyomas, and one was consistent with right atrial myxoma. Most have blocked inlet or outlet tracts. Arrhythmia was observed in one case.
Key words: prenatal diagnosis, cardiac tumors, tuberous sclerosis, rhabdomyomas, genetic counseling. Five of these were rhabdomyosarcomas and also atrium fibroids. Large blockage of inlet and outlet passages. In the case there was arrhythmia.
Action tactics
In most cases, if a hyperechoic inclusion is detected, additional research is indicated. In this case, they can assign:
- repeat ultrasound to clarify the diagnosis;
- echocardioscopy (performed only until the 25th week);
- blood chemistry;
- karyotyping.
Invasive diagnostic procedures are used quite rarely:
- amniocentesis (taking a sample of amniotic fluid through the abdominal wall);
- placentocentesis (biopsy of placental cells);
- fetoscopy (examination of the fetus using a video probe).
First of all, of course, genetic causes of hyperechoic inclusion should be excluded. To do this, the diagnostician searches for other small markers of chromosomal pathologies. These include congenital heart defects, thickening of the cervical fold, developmental disorders of the gastrointestinal tract and skeletal system. They are usually detected during ultrasound examination. If they are detected, consultation with a geneticist is necessary.
If no additional signs are found, the fetus can be considered completely healthy. However, a follow-up echocardiogram is recommended in the first months after birth. This procedure will make sure that there are no pathological changes.
Description of diagnosis
A hyperechoic focus (HEF), shown on an ultrasound machine during examination of the fetal heart, is usually an incidental finding. Diagnosis of the main organ is included in the list of mandatory tasks for every pregnant woman; it is this area that deserves special attention from doctors. The patient attends all procedures as planned, and at a certain time the doctor talks about such inclusion when examining the child’s organ.
All parents can be reassured by saying that a hyperechoic focus in the fetal heart is not a dangerous pathology. This feature does not have a negative impact on the functioning of the organ, which is confirmed by the study of a similar condition in a baby. Usually the disorder is detected at 18-22 weeks, this period is considered suitable for a second screening using ultrasound. Further, the deviation is observed unchanged and does not disappear until childbirth. Statistical data show that an echogenic focus most often appears in the left ventricle of the fetus; relatively rarely, pathology is found in the right ventricle, as well as in the area of other cardiac chambers. On average, approximately 7%-8% of all pregnant women may experience this problem.
When performing an ultrasound, the doctor notices a white spot measuring about 2-3 mm, round in shape, located in the area of the left, right ventricle or the cavity of the organ chambers. Another name for such a deviation, which is often used by diagnosticians, is qolf ball or golf ball. This comparison is indeed appropriate, since the round ball on the heart, which bounces during each contraction of the organ, resembles a ball.
A similar picture on the monitor of an ultrasound machine usually occurs as a result of the appearance of a dense formation consisting of bone tissue, so many doctors are amazed to see it in this particular place. No one knows how such a seal appears on the heart and where it disappears after childbirth.
What the GEF shows:
- The chorda accessory, which are fibers passing from the ventricles and attached to the valves.
- Salt deposits (usually calcium salts).
- Pathological process of a chromosomal nature.
- Another type of anomaly that does not pose a danger to the activity of the heart muscle.
The accessory chord will not go anywhere after childbirth, but it does not interfere with the functioning of the organ. It should be borne in mind that in this state, when the heart beats, it can make noises that will be audible to the doctor when listening. The reason may lie in any of these factors, but there is no need to identify it.
conclusions
Thus, a hyperechoic inclusion detected by ultrasound is not an independent diagnosis. According to the system for assessing markers of chromosomal abnormalities, he is awarded only one point, which cannot be a cause for concern.
Most often, GEF occurs as a result of physiological processes or benign anomalies of cardiac development (the appearance of a false chord). However, if no other anatomical or functional abnormalities are found, no further examination or treatment is required. Monitoring during a routine ultrasound in the third trimester of pregnancy will be sufficient.
First ultrasound
Doctors recommend doing the first ultrasound at 18 to 20 weeks. If there are abnormalities in the development of the fetus, they will be quickly detected. There are also indicators, in the presence of which, experts recommend a planned study:
- There are people in the family with heart defects. Especially if it is from the mother or from a brother or sister who was born earlier;
- The pregnant woman has diabetes mellitus, she had rubella, her blood pressure is noticeably elevated, etc.
- The expectant mother was taking medications that can pathologically affect the development of the heart and can cause a defect;
- An ultrasound of the fetal heart, which must be done routinely at 20 weeks, revealed an arrhythmia in the fetus;
- The woman underwent an IVF fertilization procedure.
The heart begins to work at the end of the 3rd week in the fetus. 2 more will pass and the instruments are already registering this rhythm. Contractions are not always clearly audible. To detect the baby’s heartbeat, the sensor is placed on the pregnant woman’s stomach, but only 50% of studies are successful until the 7th week.
A specialist can obtain a truly reliable result only at the end of the 8th week. In other cases, it is possible to determine whether the blood flow is good, but it is impossible to obtain accurate data on the condition of the heart. If the fetal heart beats at too low a rate, it continues to be monitored with repeated ultrasounds. If everything is as bad in the future, the question may arise about the advisability of terminating the pregnancy. Of course, if the mother is categorically against it for religious and other reasons, no one can force her.
From 6 to 8 weeks, it is considered excellent if the baby’s heart beats 110-130 beats per minute. From the 9th or 10th week the rate increases to 200 beats per 1 minute. In addition to the fetal heart rate, the doctor notes how the heart and circulatory systems are formed, are there any pathologies? The most informative is considered to be an ultrasound, which is going to be done from 18 to 28 weeks. At this stage, the anatomy of the organ is already clearly visible.
The technique of making a four-chamber cut has proven itself to be excellent. There you can see 2 atria, 2 ventricles, and the partitions between them are clearly visible. The cusps of the tricuspid and mitral valves are visible. A valve is also noticeable, closing and opening at the oval-shaped hole.
When a specialist evaluates a four-chamber slice with ultrasound, he should ask himself the following questions:
— Is the fetal heart in the correct position?
— Is it the size it should be at these times? When the heart is 1/3 in the chest, this is normal. if more, it means cardiomegaly. It happens when there are some congenital defects.
— Is the axis of the heart located correctly? If not, we can conclude that there are defects in the main arteries.
— The ventricles and atria should be approximately the same size, otherwise this signals the initial stage of some kind of disease. For example, stenosis in the pulmonary artery or Ebstein's anomaly, or something else.
— Are there any defects in the interventricular septa?
— Are the atrioventricular valves in a normal position?
— Are there any abnormalities observed in the myocardium or endocardium, or maybe in the pericardium?
90% of ultrasounds done in the 2nd trimester will show what the four-chamber structure of the organ is now. If everything is within normal limits. then standard routine examinations are then prescribed.
Diagnosis of the problem
If GEF is detected, the specialist refers the pregnant woman to amniocentesis and cordocentesis. Additionally, 3D fetal ultrasound, echo, cardiotocography and Doppler ultrasound are performed.
The most effective diagnostic methods:
Thanks to the use of new echocardiographic methods, we can evaluate the heart from different projections. Doppler examination allows you to evaluate the functions of individual parts of the circulatory system. After the interview, parents are interviewed, during which we explain the nature of the problem, we offer additional tests, such as a karyotype or “map” of the child’s chromosomes. Once all results are received, we will provide parents with full information about the potential and results of the treatment. In some cases, we will arrange a visit to the center that will care for the baby after birth.
- Blood test to detect abnormal chromosomes.
- Fetoscopy allows you to identify the pathological development of a child as a result of genetic disorders. The method is an examination of the amniotic space using a tube inserted through the uterine wall of a pregnant woman. The use of fetoscopy is justified if other diagnostic methods have already been used and have not yielded results. Fetoscopy is considered a dangerous method and is therefore used in extreme cases. There is a possible risk of premature birth.
- Placentocentesis (biopsy) is used to obtain the material required to study the cellular composition of the placenta. The method allows you to study the genes of the fetus and confirm or refute the presence of genetic diseases.
- Amniocentesis is a method that allows you to examine amniotic fluid through a puncture in the abdominal wall of a pregnant woman. Provides biochemical, immune and hormonal indicators to assess the risk of genetic disorders.
More about echocardioscopy
An ultrasound of the fetal heart is prescribed to a woman if there are the following indications:
- age over 35 years;
- diabetes mellitus of any type;
- infectious diseases suffered in early pregnancy;
- routine ultrasound revealed pathology of the fetal heart muscle;
- the child in the womb lags behind in terms of development;
- the pregnant woman or one of her close relatives has a heart defect.
The opportunity to perform an echocardioscopy procedure appears from the 18th week of pregnancy, when you can listen to the baby’s heartbeat using ultrasound. If echocardioscopy was not performed before 28 weeks, then its information content is minimal due to the large amount of amniotic fluid and the large size of the fetus.
The procedure is designed to evaluate the functioning of the heart muscle, valves, cavity sizes, their filling and contractility. The data obtained is then compared with the norm, according to the woman’s gestational age:
- width of the right ventricle – 0.4-1.10 cm;
- left ventricular width – 0.4-0.9 cm;
- length of the left ventricle – 0.9-1.15 cm;
- length of the right ventricle – 0.7-1.75 cm;
- size of the aortic orifice – 0.3-0.5 cm;
- diameter of the tricuspid foramen – 0.3-0.6 cm;
- the mouth of the pulmonary artery – 0.2-0.5 cm;
- Heart rate varies from 140 to 160 beats per minute.
Fetal heartbeat on ultrasound: what are the nuances?
The cardiac muscle of the fetus begins to form at the beginning of the fourth week of pregnancy and at this stage it resembles a hollow tube.
In the middle of the fifth week, the heart begins to work for the first time, that is, its first contractions “start.”
By the ninth week, the muscle already consists of four chambers and resembles a full-fledged organ of any adult (includes the atria and ventricles).
It is important to perform fetal ultrasound correctly. Thus, the first fetal heartbeat can be listened to using this method, but only with a transvaginal type sensor, already in the fifth or sixth week of pregnancy (this depends on the rate of fetal development)
The use of a transabdominal type sensor is possible a week later.
At this time, the specialist records the number of fetal heartbeats, and their absence may be evidence of a “frozen” pregnancy. In such a situation, a woman needs to undergo a repeat ultrasound scan after five to seven days. This will help confirm or refute the presented diagnosis.
Greatest danger
In rare cases, a hyperechoic focus may persist after birth. In such a situation, blood pressure in the left atrium increases, due to which an insufficient amount of physiological fluid enters the right atrium. Among the consequences of this pathology, oxygen starvation of internal organs is noted. If the diagnosis is not made in a timely manner, even the death of the fetus from hypoxia—oxygen starvation—is possible.
A child born with this pathology may experience the following symptoms during the first years of life:
- Increased fatigue, which is expressed in drowsiness and reluctance to play for a long time.
- Apathy.
- Attacks of acute pain in the heart area, which arise due to disturbances in its functioning.
- Shortness of breath, especially during light physical exertion, such as climbing stairs or active games.
- Cardiopalmus. This symptom can be either constant or periodic.
- Swelling of the limbs, which is most noticeable in the evening, as well as in the morning if the child drank water at night.
- Paleness of the skin, sometimes cyanosis.
- Cool hands even in hot weather.
In addition, attacks of tachycardia and rapid breathing are sometimes observed. In such cases, it is necessary to register the child with a cardiologist. He will prescribe appropriate treatment that will help relieve symptoms in a sick child. By the age of 4, the child will either “outgrow” the disease on his own, or may require medication or surgery.