General information
Terminal states of a person are borderline states between life and death. The terminal condition is characterized by severe disorders of important systems (cardiovascular and respiratory) of the body, which requires emergency resuscitation. Terminal conditions include: severe shock , extreme coma , pre-agony , agony , clinical death .
All these conditions differ in the degree of impairment of vital organs and the brain. Today we will touch on various types of comas that can occur in everyday life (for example, coma due to diabetes mellitus, stroke, liver and kidney diseases) and you need to navigate them, not get confused and correctly provide first aid to a person, since delay significantly aggravates the condition. Coma is a profound depression of the central nervous system with impaired consciousness that borders between life and death.
In coma, reflexes and reactions to stimuli are reduced or absent. The patient’s cardiac activity, breathing and metabolic processes are preserved, but their parameters change significantly, and this affects the condition of the whole organism. Depending on the disease, coma occurs instantly or develops over several hours.
Types of diabetic coma
Increased attention to the prevention of the development of diabetic comas is due to the high level of complications of these life-threatening conditions. The mortality rate for diabetic ketoacidosis (DKA) in European countries is 2-7%, in the Russian Federation 7-19% [1].
The incidence of DKA in people living with type 1 diabetes mellitus (DM) is 10-100 cases per 1000 cases. About a third of them end up in hospitals in a state of diabetic coma [2]. At the same time, competent glucose-lowering therapy can significantly reduce the likelihood of developing comatose states and delay the development of other serious complications of diabetes [1].
There are 4 types of comas that develop in diabetes:
- Diabetic ketoacidotic. In the medical literature it is also referred to as hyperglycemic hyperketonemic.
- Diabetic non-ketoacidotic hyperosmolar. It is also hyperosmolar non-acidotic.
- Lactic acidosis (lactic acidosis).
- Hypoglycemic coma [2, 3, 7].
Pathogenesis
The pathophysiology of metabolic coma, which we are considering today, is a disruption of metabolic processes in the brain. Metabolic coma occurs when the delivery of necessary substances and oxygen to the brain is stopped (for example, with hypoxia , ischemia , a sharp decrease in blood sugar) or with damage to neuronal membranes (with intoxication - drug, uremic, alcoholic, liver diseases and epilepsy ). In this case, brain damage develops focal or diffuse. Coma due to liver or kidney failure is accompanied by significant metabolic disturbances in neurons. The toxic effect in this case is multifactorial and leads to a decrease in energy reserves in cells, changes in membrane potential, disorders of neurotransmitter transmission, and even organic changes. In hepatic coma, an increase in ammonia concentration in brain tissue disrupts the function of the Na+, K+ and ATPase pump and energy metabolism.
Hypoglycemia leads to intracellular accumulation of lactate, calcium, and fatty acids, and this causes cell death. A shift in the acid-base state occurs ( metabolic acidosis ). There are also various imbalances of electrolytes: sodium, calcium, potassium, and hyperammonemia . The most significant changes in hypoglycemia are changes in potassium (hypo- and hyperkalemia), as well as sodium ( hyponatremia ).
Thus, the pathogenesis of comatose states includes the following links:
- Hypoxia and disruption of energy supply. Moreover, the disorder in the provision of oxygen to tissues is the most important pathogenetic link. Brain neurons become vulnerable during hypoxia. Stopping blood circulation in the brain for 8-10 seconds already disrupts the supply of energy to neurons - glucose reserves are depleted and ATP energy in the cell is completely consumed.
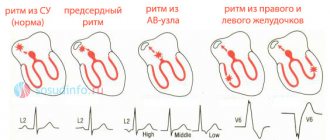
- Disruption of the energy supply not only to brain cells, but also to all tissues causes dysfunction of the heart ( arrhythmia , cardiac contractility decreases, as well as arterial hypotension ) and respiratory organs (ventilation in the alveoli decreases), which leads to cardiopulmonary failure, and hypoxia is further aggravated .
- Intoxication. Any coma is characterized by the accumulation of toxic substances that enter from the outside (exogenous comas) or are formed in the body (with any comas). Toxic substances and metabolic products of toxic substances have a negative effect on the cells of the central nervous system, heart, liver, endocrine glands, and kidneys. Intoxication aggravates the developing dysfunction of the kidneys and liver.
- Imbalance of water and electrolytes. An important link is the violation of the relationship between ions in the cell and the intercellular fluid. When membranes are damaged and the activity of Na+, K+ - ATPases decreases, cells lose K+, and [H+] and [Na+] increase inside the cell. The level of [Cl-] in the blood decreases and [H+] increases.
- As the severity of the coma increases, its specific features decrease and general features become more apparent.
Ketoacidotic
Hyperglycemic hyperketonemic coma is an acute decompensation of diabetes, which develops as a result of severe insulin deficiency. At the same time, there is a lot of glucose in the blood, but in the absence of insulin it does not enter the cells, so fat begins to be used as an energy source instead of carbohydrates.
Active breakdown and inclusion of free fatty acids in metabolism leads to the formation of ketone bodies. Their synthesis increases to 1000 mmol per day, which significantly exceeds the ability of the kidneys to excrete ketones in the urine [7].
Changes in blood and urine tests in diabetic ketoacidosis in adults are presented in table [1].
| Laboratory indicators | Values |
| Blood plasma glucose | >13 mmol/l to 18-20 mmol/l [3] |
| Plasma ketone bodies | >5 mmol/l |
| Ketonuria | ≥++ |
| pH | ˂7,3 |
Classification
Comatose states can be divided into two groups: primary (or cerebral) and secondary (so-called metabolic). In this regard, the following types of comatose states are distinguished:
- Associated with damage to the central nervous system ( stroke , traumatic brain injury , brain tumors , epilepsy ).
- Occurring when gas exchange is disrupted (hypoxic, respiratory).
- Associated with impaired hormone production (hypothyroid, diabetic, thyrotoxic, hypocorticoid, hypoglycemic, hypopituitary).
- Toxigenic (associated with the action of endogenous and exogenous toxins - hepatic, pancreatic, uremic, alcoholic).
Associated with loss of electrolytes and water (hyponatremic, chlorhydropenic with vomiting, alimentary-dystrophic).
If we separately consider comas with diseases of internal organs, we can distinguish:
- Pancreatic.
- Uremic.
- Hepatic.
- Coma in diabetes mellitus .
The stages of coma are divided into:
- Mild degree. Manifested by lethargy, lethargy, confusion .
- Moderate severity. The patient is in a stupor: does not respond to light, sounds, pain. The pressure drops, the heart rate accelerates. Chaotic movements in the legs and arms are periodically observed, and spontaneous bowel movements are observed.
- Deep coma. Shallow breathing, no swallowing, pupils dilated, blood pressure reduced.
- Terminal stage. Reflexes are completely absent, the pupils do not react, the pressure is critically reduced. The patient is connected to a ventilator and receives parenteral nutrition.
Any coma is a lack of consciousness and a state of wakefulness. The patient lies with his eyes closed, he is not aware of his surroundings, and any stimulation does not cause activity. This is due to the fact that there is diffuse damage to the cortex and white matter of both hemispheres of the brain. Damage to one hemisphere does not lead to coma.
To differentiate coma from fainting, it is generally accepted that the coma lasts more than an hour. In rare cases, it lasts more than a month.
The most common are comas due to diabetes , which are its complications and require immediate treatment. The most common is diabetic coma (synonymous with ketoacidotic), which develops with insulin deficiency, decreased glucose utilization and an increase in its level in the blood (28-30 mmol/l). Develops in patients with severe diabetes mellitus. Provoking factors are:
- improper administration of insulin ;
- increased need for insulin;
- infections, injuries, operations;
- myocardial infarction;
- cerebrovascular accidents;
- stress;
- taking drugs.
Hypoglycemic coma occurs when sugar levels drop to 2 mmol/l. In diabetic patients, this type of coma is caused by a large dose of insulin and lack of food intake, severe physical activity or alcohol intake. Hypoglycemia can also be caused by sulfonylurea drugs ( Glimeperide , Amaryl , Glyme ), but this is less common than with an overdose of insulin. Some diabetic patients experience a syndrome of atypical hypoglycemia—coma develops without prior activation of the sympathoadrenal system. Hypoglycemic conditions are also observed in people who do not have diabetes.
In endocrinology, hypothyroid coma - a severe complication of hypothyroidism , which has not been treated for a long time, so decompensation of the condition has developed. It primarily develops in older people who have not received treatment. Provoking factors for this condition are operations, injuries, serious illnesses, hypothermia, and taking sedatives. Patients in a state of hypothyroid coma die from cardiac and respiratory failure in 40% of cases, even with timely resuscitation measures.
Uremic coma is associated with progressive renal failure, which causes intoxication with nitrogenous wastes and disturbances in water and electrolyte balance. This condition can develop with glomerulonephritis , diabetic nephrosclerosis , a mechanical obstruction to the outflow of urine, or exposure to nephrotic poisons. In addition to kidney diseases, this type of coma develops with shock, massive blood loss, dehydration, which results in renal failure and uremia . There is a gradual increase in symptoms. In precoma weakness , headache drowsiness , slowness of movements, nausea, itching of the skin , and the smell of ammonia in the exhaled air appear
The stuporous state gradually increases and during coma there is no consciousness, swelling , puffiness of the face , vomiting , diarrhea , and no urine appear. Blood pressure is elevated, tachycardia and arrhythmia , shallow breathing.
Another comatose state is hypoxic coma . This is a depression of the central nervous system, which is associated with a deterioration in cellular respiration due to insufficient oxygen supply to the cell. This type of coma develops faster than other types and requires urgent restoration of respiratory function. It has several options:
- Hypoxemic - insufficient supply of oxygen from the outside.
- Asthmatic - considered as a complication of bronchial asthma .
- Anemic - occurs with decompensated anemia.
- Respiratory - develops with respiratory failure.
Epileptic coma occurs after status epilepticus, when frequent seizures occur over a short period of time. The patient is unconscious, the face is pale and cyanotic, the pupils are dilated and do not react well to light. Breathing is wheezing and frequent, blood pressure is low, pulse is weak. Involuntary urination and loss of feces. As the coma deepens, breathing becomes intermittent, the pulse becomes thready, and the bluishness of the skin increases. A characteristic symptom that allows you to distinguish coma from other types is biting the tongue and the presence of bloody foam from the mouth.
Hyperosmolar non-acidotic
Non-ketoacidotic hyperosmolar coma also develops due to acute decompensation of diabetes. It is based on a sharp decrease in insulin levels and loss of fluid from the body. In this case, there is no excessive formation of ketone bodies and acidosis [7].
| Laboratory indicators | Values |
| Blood plasma glucose | >30 mmol/l |
| Blood osmolarity | 400-500 mOsm/l [4] |
In a general blood test, an increase in hemoglobin and hematocrit levels is noted due to a decrease in plasma volume. There is no acetone in the urine [3].
Causes
The reasons for this condition are varied and the following can be distinguished:
- Traumatic factors (brain injury, exposure to electric current).
- Thermal effects (this can be overheating and hypothermia).
- Exposure to neurotoxins ( ethylene glycol , alcohol substitutes , drugs in toxic doses, barbiturates and sedatives ).
- Hypoxia.
- Infectious factors (exposure to neurotropic viruses, toxins of botulism, malaria, typhus).
- Exposure to large doses of radiation.
- Pathological conditions ( stroke , brain tumor , cerebral edema , abscess ).
- Blood pathology ( hemolysis of red blood cells , anemia ).
- Respiratory failure.
- Liver failure.
- Kidney failure.
Hyperglycemic coma is provoked by:
- Incorrect administration of insulin (reducing the dose and number of injections, unauthorized withdrawal of insulin).
- Infections.
- Injuries and surgeries.
- Acute cardiovascular diseases.
- Psycho-emotional stress.
- Taking drugs.
- Long-term use of glucocorticoids and diuretics.
- Pregnancy.
Hypoglycemic coma is provoked by:
- Violation of the diet with skipping meals.
- Insulin overdose (faulty syringe pen, error in dose calculation, malfunction of the glucometer).
- Drinking alcohol.
- Changing insulin medications.
- Excessive loads.
- Impaired kidney and liver function.
Symptoms of coma
Clinical manifestations depend on the stage of coma. The initial stage is called precoma and includes a state of stupor, stupor (or stupor). All of them, unlike coma, are distinguished by the preservation of reactions and the patient can be brought out of this state by a painful or sound stimulus. Common conditions for all types of coma are:
- Stunning is a slight depression of consciousness. The patient's movements and speech are somewhat slow, and his face is unexpressive. The patient loses the ability to attentively perceive speech and experiences moderate drowsiness . The pauses between questions and answers lengthen. However, the patient is oriented to the individual, the situation, assesses the situation and follows all commands. During the period of stunning, partial amnesia may be observed (the patient cannot reproduce some events). Deep stupor is characterized by increasing drowsiness, lethargy, and slow speech. Communication with the patient is possible, but it is necessary to repeat questions many times or attract the patient’s attention by patting. The patient answers in monosyllables. With such limited contact, it is established that the patient is oriented in the person and situation, but disoriented in time. The patient's movements are sharply slowed down, and he can only carry out simple commands. The response to pain persists, and control over urination and bowel movements is weakened. With deep deafness, partial amnesia .
- Sopor. This deep depression of consciousness and communication with the patient is impossible - he is in a dream. The patient is awakened by intense external stimuli, to which he opens his eyes. The patient's face is hyperemic and there is an increase in heart rate to the voice of someone close to him. In this state, he can localize pain, and without irritation he is motionless. During the period of stupor, complete amnesia is noted. apnea may occur . There are no reflexes except the pharyngeal ones.
- Stupor develops with mental illness ( schizophrenia ), and stupor develops with somatic illnesses, infections or injuries. This condition is also characterized by pathological drowsiness, the patient opens his eyes only to sound. He is capable of simple movements, swallows food and water, and can change body position. The patient's tendon reflexes are weakened and skin reflexes are increased. Thus, stupor and stupor are characterized by inhibition and difficulty in contact. But with stupor, hallucinations and delusions , and with stunning, the patient is completely indifferent and lacks any experiences.
Coma is a state of complete absence of reflexes, characterized by very low blood pressure and body temperature, dilated pupils and rare breathing. A comatose state is characterized by the fact that the patient cannot be awakened and does not respond to stimuli. In comas that have developed against the background of diseases of the internal organs, there are characteristic symptoms that suggest its type.
Symptoms of hypoglycemic coma
Signs of hypoglycemia (sugar less than 2.5 mmol/l) develop in a short time and are associated with activation of the sympathoadrenal system , so the patient experiences increased sweating, hand tremors, palpitations, hunger, pale skin, nausea and anxiety. With a further decrease in blood sugar, the brain suffers as neuroglycopenia . It manifests itself as headache, disorientation, confusion, difficulty speaking, movement disorders (paresis, paralysis), convulsions, behavioral disorders, and amnesia. If the patient does not receive help at this stage, he falls into a coma.
Symptoms of hyperglycemic coma
Characteristic signs of hyperglycemic coma are a gradual increase in all symptoms of diabetes mellitus (thirst, dry mouth, excessive fluid intake, excessive urination) and eventually coma . A diabetic coma can take several days to develop. At an early stage, in addition to the characteristic complaints for decompensated diabetes mellitus, there is a dysfunction of the central nervous system - headache , apathy , adynamia and drowsiness or increased excitability .
As the coma deepens, dysfunction of the nervous system progresses. Nausea, vomiting, acute abdominal pain, shortness of breath , rapid heartbeat , smell of acetone from the mouth, and decreased reflexes appear. Typical symptoms of ketoacidotic coma are frequent deep breathing (called Kussmaul breathing) and the smell of acetone. When examining the patient, a pronounced loss of fluid is noted - dry skin, mucous membranes and decreased turgor.
Hypothyroid coma
This condition is characterized by a gradual increase in all symptoms of hypothyroidism. These are drowsiness, a decrease in temperature to 34C, a slow pulse, cold extremities, swelling of the face and the whole body. The main symptom of this coma is a decrease in temperature. Coma is accompanied by increasing changes in the central nervous system: lethargy, disorientation, suppression of all reflexes. CNS depression causes an even greater decrease in heart rate and blood pressure, as well as hypoglycemia. The cause of death of a patient in this condition is pronounced changes in the cardiovascular system.
Hepatic coma
Hepatic coma is considered stage IV of hepatic encephalopathy (pathology of the central nervous system), developing in chronic liver diseases or fulminant acute hepatitis . If the patient has suffered one episode of hepatic encephalopathy, then there is a high probability of relapse in the presence of provoking factors. Coma is preceded by precoma - stage III encephalopathy, which is characterized by drowsiness, confusion, disorientation, amnesia, slurred speech, attacks of rage, irritability and disinhibition, and inappropriate behavior. Disturbances in sleep and wakefulness are typical - patients are excessively sleepy during the day and do not sleep at night.
Hepatic coma is manifested by loss of consciousness and a complete lack of response to any irritants. In acute liver failure, coma occurs with psychomotor agitation, and then lethargy and drowsiness develop. Some patients with prolonged coma develop stereotypic movements (sucking, chewing or grasping). And in the terminal stage, the pupils dilate, the reaction to light disappears, general clonic convulsions and respiratory arrest appear.
Treatment
Prevention
If certain conditions are met, a coma due to diabetes mellitus may not threaten the patient with diabetes. These rules are quite simple:
- Follow your diet.
- Monitor your glucose levels.
- Follow your insulin therapy schedule.
- Do not use expired insulin.
- Avoid stress.
- Avoid excessive physical activity.
- Treat infectious diseases in a timely manner.
- Give up bad habits - smoking, drinking alcohol.
- If warning signs appear, seek emergency help.
Parents whose children have insulin-dependent diabetes should carefully monitor their diet and take insulin injections on time. Gradually, children need to be taught to independently follow doctor’s orders.
Urgent Care
If a diabetic clearly shows signs of a precomatose state associated with hyperglycemia, the following steps must be taken:
- Provide the patient with comfortable conditions (put him to bed, eliminate irritating factors);
- Inject short-acting insulin under the skin every 2 to 3 hours with mandatory concomitant monitoring of sugar levels;
- Limit his intake of carbohydrates;
- Give him magnesium and potassium supplements;
- Drink mineral water (alkaline) often.
If the condition does not return to normal or worsens, you must immediately seek medical help and call an ambulance.
If the patient has lost consciousness and signs of a diabetic coma are detected, you need to provide him with all possible first aid:
- Place the patient on his side to prevent vomit from entering the respiratory tract;
- Remove dentures from the oral cavity (if they are present);
- Watch your tongue so that it doesn’t sink;
- Measure your sugar level;
- Inject insulin (inject);
- Call an ambulance;
- Monitor your pulse and breathing;
- Describe in detail the background of the attack to the arriving medical team.
When providing emergency care, adhere to the following principles:
- Do not leave the patient alone;
- Do not forbid him to inject insulin into himself (if he is in adequate condition);
- Do not neglect to call an ambulance, even if the patient’s condition has been stabilized.
If the patient falls into a coma, he will definitely need hospital treatment. The length of his stay in the hospital will depend on the severity of the condition; coma with diabetes can lead to serious consequences.
Timely initiation of treatment in a medical facility will preserve the patient’s health. Treatment includes several mandatory steps:
- Fighting dehydration;
- Combating insulin deficiency;
- Correction of electrolyte imbalance;
- Correction of PH shift (metabolic acidosis);
- Treatment of associated disorders.
The treatment regimen is as follows:
- The patient is given insulin in small doses intravenously until signs of coma disappear. In this case, every 2–3 hours, blood is taken for analysis (to control sugar) and urine (to control sugar and acetone).
- To prevent an overdose of insulin, a dose of glucose is administered an hour after the injection; such manipulation contributes to the “burnout” of ketone bodies. Glucose injections have to be given up to 5 times a day.
- Drip administration of saline solution with soda will help fight acidosis and maintain vascular tone. For the same purpose, an intravenous injection of sodium chloride is given.
- The patient is applied heating pads to the limbs and given an oxygen cushion to speed up the oxidation-reduction processes in the body.
- To maintain cardiac activity, the patient is injected with caffeine and camphor, vitamins B1, B2 and ascorbic acid are prescribed.
At first, rapid insulin is administered continuously in small doses, after sugar has been reduced to 16 mmol/l, long-acting drugs are added, and at the first opportunity the patient is transferred to his usual diabetes treatment regimen. After eliminating hyperglycemia, glucose is administered to the patient in small quantities to meet energy needs. As soon as he begins to feed on his own, the drips are stopped.
Similar tactics are followed in the treatment of dehydration: first, saline and potassium chloride are injected into the bloodstream in large quantities, and then simply monitor whether the patient drinks enough water. Intoxication with acetone decreases as soon as urine excretion resumes.
Blood acidity usually recovers on its own as the blood composition is corrected. Sometimes it is necessary to reduce the acidity forcibly, then for this purpose droppers with sodium bicarbonate are used.
Are you suffering from high blood pressure? Did you know that hypertension leads to heart attacks and strokes? Normalize your blood pressure with... Read the opinion and review about the method here
Diet
Diet 9th table
- Efficacy: therapeutic effect after 14 days
- Timing: constantly
- Cost of products: 1400 - 1500 rubles per week
Diet for low blood sugar
- Efficacy: stabilization of blood sugar levels
- Dates: no data
- Cost of food: 1930 - 2100 rubles per week
In each specific case, for various diseases, dietary nutrition is indicated. For diabetes mellitus - Table No. 9 , for kidney pathology Table No. 7 , and for liver diseases - Table No. 5 . In hepatic encephalopathy, correction of nitrogen metabolism is crucial. 75% of patients with hepatic encephalopathy have protein and energy deficiency, which is accompanied by loss of muscle and energy reserves. Long-term restriction of protein in the diet is harmful for such patients, since the need for it in this condition is lower than in healthy people. Weight loss and muscle breakdown increase hepatic encephalopathy, so it is necessary to provide the body with sufficient protein and energy and achieve a positive nitrogen balance. In this regard, for normal weight, a daily protein intake of 1.2-1.5 g/kg is recommended, and the calorie content of the diet should be maintained at 2400 kcal.
It is recommended to eat evenly throughout the day and have a snack before bed. You need to limit your protein intake during the first days of the onset of encephalopathy, and then return to your normal protein intake. To reduce the amount of protein, it is replaced with vegetable or dairy or a complex of branched chain amino acids - BCAA in capsules.
Prevention
If there is an endocrinological pathology, in this case diabetes mellitus, the patient needs to carefully monitor his condition and its changes. People suffering from diabetes are usually well aware of changes in their condition, regularly measure their sugar levels at home and immediately take action. Patients know that after an insulin they need to eat, they keep a diabetic diary and follow a diet. Persons who are not treated or do not know about the presence of diabetes mellitus can bring themselves into a coma. Severe stress, alcohol exposure, or severe infectious diseases can provoke a sharp deterioration in their condition, even to the point of coma.
First aid
Correction of the patient's condition is carried out in a medical institution. People with moderate ketoacidosis are hospitalized in the therapeutic/endocrinology department, and in a state of precoma and coma - in the intensive care unit [4].
At home you can:
- conduct a rapid glycemic analysis if you have a glucometer;
- call an ambulance.
A person with ketoacidosis can be given 20 units intramuscularly. short-acting insulin (RAI) [4]. With moderate hypoglycemia, the patient needs to take easily digestible carbohydrates (sugar dissolved in tea, water, a piece of bread) [3].
In the emergency department, a urine test for ketone bodies is additionally performed and infusion therapy begins with the introduction of a 0.9% NaCl solution at a rate of 1 l/h [4].
Consequences and complications
Complications of hyperglycemic coma are:
- Severe acidosis .
- Hypokalemia.
- Hypocalcemia.
- Infection.
- Brain swelling . This is a rare complication that occurs more often in children and develops 4-12 hours after treatment. The reason is a rapid decrease in blood glucose or osmolality, as well as the presence of hypoxia of the central nervous system. To avoid a rapid decrease in osmolarity, first use 0.9% sodium chloride , and then 0.45% sodium chloride . And to prevent a rapid decrease in blood sugar, first perform rehydration (replenish the loss of the liquid part of the blood), and after 2 hours begin administering insulin.
- Shock.
- Pulmonary edema.
- Arterial thrombosis.
Complications of severe hypoglycemia include:
- Cardiovascular complications ( angina pectoris , myocardial infarction , stroke , atrial fibrillation, paroxysms of ventricular tachycardia , myocardial ischemia ).
- Neuropsychic ( convulsions , paresis , paralysis, decortication , behavioral disorders, intellectual disorders, psychoses ).
With uremic coma, the following may develop:
- Bloody vomiting.
- Brain edema.
- Uremic peritonitis .
- Hemorrhagic stroke.
With hepatic coma the following are possible:
- Brain swelling
- Bleeding.
- Kidney failure.
- Respiratory failure.
Forecast
The prognosis for a comatose state depends on the cause, as well as the degree of depression of consciousness and the duration of its depression. In case of precoma or the presence of stage I coma, a favorable prognosis is noted. In the case of coma II and III degrees, the prognosis is questionable, but there is hope for recovery. If we consider a IV degree coma, it most often ends in death. A deep coma lasting more than 24 hours has a poor outcome. If reflexes are absent for less than 6 hours, the prognosis is relatively favorable.
Favorable prognostic factors are:
- Early return of speech.
- Spontaneous eye movements.
- Preserved muscle tone at rest.
- Ability to execute commands.
The prognosis is unfavorable if patients, after circulatory arrest, experience:
- Myoclonic status epilepticus .
- Lack of pupil reaction for 24-72 hours.
- Absence of corneal reflexes.
- No response to pain within 72 hours.
In uremic coma, all reflexes and motor reactions may be lost, but recovery after treatment is complete. If hypothyroid coma , death occurs in 60-90%.
If a patient develops a hepatic coma against the background of chronic liver pathology, then every fifth person does not come out of it and death occurs after 1-3 days. How long do people live in a hepatic coma after they come out of it? This period depends on many factors, but most often the life span does not exceed several months, provided that the patient is constantly supported by liver function. Life extension is possible through organ transplantation - patients live from 5 to 10 years. Coma with fulminant hepatitis ends in death in 85% of patients. Patients with liver failure live for 3 months.
List of sources
- Efimov A. S., Komissarenko I. V., Skrobonskaya N.A. Emergency endocrinology. – M.: Medicine, 1982, – 208 p.
- Balabolkin M.I., Lukyanchikov V.S. Clinic and therapy of critical conditions in endocrinology. – Kyiv: Health, 1982, – 152 p.
- Kurek, V.V. Guide to emergency conditions in children / V.V. Kurek, A.E. Kulagin. 2nd ed. Moscow: Med. lit., 2012, - 464 p.
- Sumin, S. A. Anesthesiology, resuscitation, intensive care: textbook. for students of institutions of higher professional education / S. A. Sumin, I. I. Dolgina. Moscow: Medical Information Agency, 2015, 496 p.
- Krylov, V.V. Neuroreanimatology. Practical guide / V. V. Krylov, S. S. Petrikov. Moscow: GEOTAR-Media, 2010, - 176 p.
Resuscitation actions
Indications for resuscitation measures are:
- lack of breathing or pulse;
- heart failure;
- blue discoloration of the skin surface;
- absence of any reaction of the pupils when light hits them.
If you have these symptoms, you should not wait for the ambulance to arrive.
The patient's relatives should begin to act independently according to the following recommendations:
- Place the patient on a hard surface.
- Open access to the chest, freeing it from clothing.
- Tilt the patient's head back and place one hand on his forehead, and with the other push the lower jaw forward to ensure airway patency.
- Remove food debris from the mouth (if necessary).
When performing artificial respiration, it is necessary to firmly touch your lips with the patient’s mouth, having first placed a napkin or a piece of clean cloth on it. Then you need to take deep exhalations, closing the patient’s nose in advance. The effectiveness of the actions taken is determined by the raising of the chest at this moment. The number of breaths per minute can be up to 18 times.
To perform indirect cardiac massage, the hands should be placed on the lower third of the patient’s sternum, located on the left side of him. The basis of the procedure is energetic pushes made towards the spine. At this moment, the surface of the sternum should shift by a distance of 5 cm in adults and 2 cm in children. You need to perform about 60 presses per minute. When combining such actions with artificial respiration, each breath should alternate with 5 compressions on the chest area.
The described steps should be repeated until the doctors arrive.
Video lesson on resuscitation measures:
- In case of ketoacidosis coma, it is necessary to administer insulin (first in a stream manner, and then in a drip method with dilution in a glucose solution to prevent hypoglycemia). Additionally, sodium bicarbonate, glycosides and other agents are used to maintain heart function.
- In case of hyperosmolar coma, infusion drugs are prescribed to replenish fluid in the body, and insulin is administered intravenously by drip.
- Lactic acidosis is eliminated by using the antiseptic Methylene Blue, Trisamine, sodium bicarbonate solution, and insulin.
The actions of specialists depend on the type of coma and are performed in a hospital setting.