Diabetes mellitus type 2.
It is a chronic disease of the endocrine system, which develops due to a lack of insulin and dysfunction of pancreatic cells. It manifests itself as excessive urination, increased thirst, itchy skin, increased appetite, fever, and muscle weakness. The diagnosis should be confirmed by laboratory tests, namely through a blood test for glucose concentration and the level of glycosylated hemoglobin. Treatment mainly uses a low-carbon diet, increased physical activity and hypoglycemic drugs.
Information about the disease.
In fact, “diabetes mellitus” from Greek means loss of sugar. Thus, the term reflects the main symptom of the disease (lack of sugar) - glucose is not retained in the body and is excreted in the urine. Type 2 diabetes mellitus (non-insulin-dependent) develops against the background of tissue insensitivity to the action of insulin, as well as a subsequent decrease in cell function. Diabetes mellitus type 2 (DM2) is different from diabetes mellitus type 1 (DM1). In diabetes 1, the lack of insulin is primary; in diabetes 2, the lack of the hormone is a consequence of a prolonged lack of insulin. Statistics are very diverse and depend on ethnic characteristics and living standards. In Russia, the prevalence is about 7%, and covers 90% of all forms of diabetes. The group most susceptible to the disease is people over 40-45 years of age.
What is this?
Diabetes mellitus (DM) type 2 is a chronic disease with a persistent increase in blood glucose levels due to a decrease in the sensitivity of body cells to the hormone insulin. In healthy people, insulin binds to cell receptors and helps glucose enter the cells. If cell membranes for some reason become deformed or there are fewer insulin receptors on them, the cells stop “recognizing” the hormone, and insulin resistance forms. As a result, sugar, instead of supplying the body with energy, accumulates in the blood, and this greatly harms the blood vessels, heart and brain.
How many people have diabetes?
The number of people with diabetes is growing from year to year (Fig. 1). According to the International Diabetes Federation, there are about 463 million adult patients in the world. Moreover, in 2014 there were 422 million, and in 1980 - 4 times less - 108 million. Type 2 diabetes makes up about 90% of all cases of this disease.
Figure 1. Projected number of diagnosed cases of type 2 diabetes among adults in different countries. Source: Statista
Causes of type 2 diabetes mellitus.
The disease develops due to a combination of hereditary predisposition and external factors affecting the body throughout life. By adulthood, negative exogenous influences reduce the sensitivity of cells to insulin, as a result of which they cease to receive sufficient amounts of glucose. The main causes of type 2 diabetes:
- • Obesity. Fat tissue reduces the ability of cells to properly perceive insulin. Excess weight is one of the key risk factors for developing the disease. Obesity is present in 80-90% of patients;
- • Poor nutrition. The main cause of obesity is overeating. An increased calorie intake leads to the development of type 2 diabetes. In addition, excessive consumption of large amounts of sugar provokes surges in insulin secretion, which also provokes the development of the disease;
- • Physical inactivity. Lack of physical activity has a bad effect on the functioning of most organs of the body, and also helps to slow down metabolic processes. Physical inactivity is accompanied by low consumption of glucose by muscles, so it accumulates in the blood;
- • Endocrine diseases. Often, the disease occurs against the background of disruption of the endocrine system. Cases have been reported against the background of pancreatic tumors, pancreatitis, hypo- or hyperfunction of the thyroid gland;
- • Infectious diseases. In people with hereditary pathology, the initial appearance of diabetes mellitus can be triggered by an infectious disease - herpes, influenza and hepatitis.
Recommendations
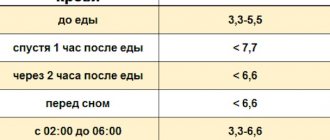
Even in the absence of an established diagnosis of diabetes, it is recommended to monitor blood sugar once a year - this is the simplest and most accessible method of early diagnosis of the disease. There is no specific prevention of diabetes, so it is recommended to maintain a healthy lifestyle: rational exercise and proper nutrition.
In the case when this diagnosis is confirmed, constant contact between the patient and the doctor is necessary. Only under this condition is it possible to prevent the destructive effects of diabetes on the body.
Mechanism of disease development.
The basis of the disease is a violation of carbohydrate metabolism due to increased cell resistance to insulin. The ability of tissues to accept and utilize glucose decreases, and a state of hyperglycemia (increased plasma sugar levels) develops. In addition, alternative ways of obtaining energy from amino acids and fatty acids are activated. To compensate for the glucose balance, the body begins to remove it through the kidneys (in the urine). A high concentration of sugar in body fluids causes an increase in osmotic pressure, causing copious and frequent urination. During this process, more fluid and salts are removed from the body, leading to dehydration and electrolyte imbalance. All this provokes the main symptoms of the disease - thirst, dry skin, weakness and arrhythmia.
Classification of the disease:
- • Lightweight. Treatment requires dietary adjustments, as well as a small dosage of a hypoglycemic drug. Low risk of complications;
- • Medium shape. To stabilize the disorders, constant intake of hypoglycemic agents is necessary. There is a possibility of initial stages of vascular complications;
- • Severe form. Patients require a course of tableted hypoglycemic drugs and insulin. Serious diabetic complications arise - angiopathy of small and large vessels, neuropathy, encephalopathy.
Prevention
If there is a history of type 2 diabetes in your family, you are over 40 years old, you are burdened with extra pounds, you lead a sedentary lifestyle and you have high blood pressure, you should take action to prevent this disease.
Its main methods are:
- Proper nutrition. It should be based on complex carbohydrates and foods rich in fiber. About 60% of your diet should be complex carbohydrates, 20% fats (50-70% of which are vegetable oils), 20% proteins. Give preference to poultry, lean fish, vegetables, and unsweetened juices.
- Eliminate canned food, sweets and fatty foods. Steam;
- Quitting alcohol and tobacco. Both increase the risk of developing carbohydrate metabolism disorders;
- Daily physical activity: at least half an hour of sports or walking in the fresh air;
- Stress management and regular medical examinations. People at risk need to have their blood tested for sugar once every six months.
10 unexpected circumstances that increase blood sugar levels
Sometimes blood sugar can rise due to unobvious reasons. Blood glucose levels can be affected by:
- Sunburn – pain causes stress, and stress increases blood sugar levels.
- Artificial sweeteners - Some studies show that these may raise blood sugar levels.
- Coffee - even without sweetener. Some people's blood sugar levels are very sensitive to caffeine.
- Lack of sleep – Even one sleepless night can reduce the effectiveness of insulin in the body.
- Skipping breakfast – Skipping your morning meal can raise your blood sugar levels both after lunch and after dinner.
- Time of day – It is more difficult to control your blood sugar levels late in the day than during the day.
- Dawn - People experience a surge in hormones early in the morning, whether they have diabetes or not. For people with diabetes, their blood sugar levels may spike at dawn.
- Dehydration – less water in the body means higher concentrations of sugar in the blood.
- Nasal spray - Some of these contain chemicals that cause your liver to release more sugar into your blood.
- Gum disease – This complication of diabetes can cause high blood sugar levels.
People with diabetes should also avoid situations that could cause their blood sugar levels to drop sharply. For example, extreme heat can cause blood vessels to dilate, which speeds up the absorption of insulin and can lead to low blood sugar.
Symptoms of the disease.
Type 2 diabetes develops quite slowly. At the initial stage, the symptoms are practically invisible. The first symptom that appears is increased thirst. The mouth feels dry, and patients drink about 3-5 liters per day. With this volume, the amount of urine and frequency of urination increases. Due to the increased sugar content in the urine and frequent urination, itching and redness of the groin area occurs. Over time, itching occurs in the abdomen, armpits, knees and elbows. Since glucose does not reach the tissues in full, appetite increases (after 1-2 hours after eating, the patient feels hungry). Despite the high caloric content of the diet, the patient does not gain weight, since glucose is not absorbed, but is lost in urine.
Additional symptoms include increased fatigue, chronic feeling of tiredness, daytime sleepiness, weakness. The skin becomes drier, rashes and fungal formations appear. Bruises easily appear on the body, and wounds and abrasions take a very long time to heal. Women experience genital candidiasis, and men experience urethral infections. Some patients report tingling in their fingers and numbness in their feet. After eating, a feeling of nausea and even vomiting is also noticeable. Headaches and dizziness are common.
T2DM
Type 2 diabetes mellitus (T2DM) most often affects people over 40 years of age. This form of diabetes is characterized by relative insulin deficiency. For a long time, the disease may not manifest itself at all; symptoms appear gradually, so people often seek help late. Over time, the patient may need insulin therapy. Type 2 diabetes mellitus is treated mainly on an outpatient basis.
The risk of developing T2DM is higher in the following groups of people:
- age over 45 years;
- overweight (body mass index more than 25 kg/m²);
- high blood pressure (arterial hypertension, above 140/90 mm Hg);
- genetic predisposition (close relatives suffer from T2DM);
- low physical activity;
- elevated blood triglyceride levels (≥ 2.82 mmol/L) and decreased HDL cholesterol levels ≤0.9 mmol/L.
For people who are at risk, doctors recommend doing a blood test at least once a year and monitoring their glucose levels.
Symptoms of T2DM
Type 2 diabetes mellitus does not have specific symptoms that can clearly identify the disease, but the appearance of several symptoms of the disease at the same time may be a sign of the development of T2DM. Check if you have three or more symptoms from the list below, this is a reason to see a doctor:
- you feel dry in your mouth and constantly thirsty;
- you have excessive urination, including at night;
- your skin and mucous membranes are itchy;
- you quickly get tired and feel weak;
- your wounds and skin damage are healing slowly;
- pustules appear on the skin;
- you have lost a lot of weight and suddenly for no apparent reason.
What to do if you suspect you have T2DM?
If you feel unwell and experience symptoms of diabetes, the first thing you should do is consult a doctor. An examination performed by a therapist or general practitioner will help identify T2DM. To register at the clinic, you will need a passport and compulsory medical insurance policy. The doctor will decide on the need for further examination based on the results of the examination.
The following tests help identify T2DM:
- general blood analysis;
- general urine analysis;
- biochemical blood test with blood glucose testing;
- biochemical blood test to assess lipid metabolism disorders;
- determination of the level of glycated hemoglobin in the blood;
- oral glucose tolerance test.
All of the above tests can be done at the clinic at the site of attachment. The results will be ready 1-2 days after submission. The diagnosis may be as follows:
- diabetes mellitus has not been confirmed, but there are factors for its development;
- prediabetes was detected;
- type 2 diabetes mellitus was diagnosed.
Serious complications.
The development of type 2 diabetes mellitus may be accompanied by the development of chronic and acute complications. The most dangerous complications can lead to death - hyperglycemic coma, hypoglycemic coma, lactic acid coma. Chronic complications develop gradually and include diabetic microangiopathies and macroangiopathies - manifested by thrombosis and vascular atherosclerosis. Disturbances in the functioning of internal organs, joint pain and mental disorders (depression, emotional instability) are often noticeable.
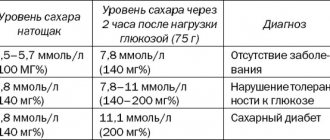
Blood sugar levels: norms and violations
| Analysis | Men | Women | ||
| norm | pathology | norm | pathology | |
| Glycated hemoglobin % (up to 30 years) | 4,5-5,5 | over 5.5 | 4-5 | over 5 |
| Glycated hemoglobin % (from 30 to 50 years) | 5,5-6,5 | over 6.5 | 5-7 | over 7 |
| Blood from a finger on an empty stomach, mmol/l | 3,3–5,5 | over 5.5 | 3,3–5,5 | over 5.5 |
| Analysis after taking 75 grams of glucose, mmol/l | less than 7.8 | over 7.8 | less than 7.8 | over 7.8 |
| Analysis for adiponectin, mg/ml | more than 10 | less than 10 | more than 10 | less than 10 |
How to diagnose type 2 diabetes?
The problem of identifying diabetes mellitus is manifested in the absence of obvious symptoms in the initial stages of the disease. Patients with a hereditary predisposition to the disease, or over 40 years of age with suspected diabetes, are recommended to undergo a blood plasma test for sugar levels. Laboratory tests will be the most informative and will detect not only the initial stage of diabetes mellitus, but also the state of prediabetes - decreased susceptibility to glucose. The examination is carried out by an endocrinologist.
To the Endocrinologist
Diagnosis begins with asking the patient about his well-being, symptoms of the disease are identified, and existing risk factors are analyzed. Once results from the laboratory are received, the diagnosis can be confirmed. There are several specific tests to detect type 2 diabetes:
- • Fasting glucose. The material is collected after 8-12 hours of fasting. Glucose levels above 7 mmol/l (venous blood) are a criterion for the disease;
- • Glucose test. To diagnose diabetes at an early stage, glucose concentrations are examined after eating a meal high in carbohydrates. With this test, a reading above 11.1 mmol/l is diabetes, a reading of 7.8-11.0 mmol/l is prediabetes;
- • Glycated hemoglobin. The analysis allows you to estimate the average glucose concentration in the body over the past 3 months. An indicator of 6.5% or more indicates diabetes, 6-6.4% indicates prediabetes.
Diff. diagnosis involves distinguishing between type 1 diabetes and type 2 diabetes. The clinical differences between these diseases are the slow increase in symptoms and the older age of the patients (although recently there have been cases of the disease in people aged 20-25 years).
Diabetes mellitus is a disease that develops as a result of a relative or absolute deficiency of insulin or a disruption of its interaction with the receptor, resulting in hyperglycemia. It is characterized by a chronic course and a violation of all types of metabolism: carbohydrate, fat, protein, mineral and water-salt.
Risk factors for developing diabetes:
- Presence of diabetes in 1st degree relatives (parents, brothers, sisters)
- Impaired fasting glucose or glucose tolerance at previous examination
- Other clinical conditions that are associated with impaired glucose tolerance
- Presence of cardiovascular diseases
- Low physical activity
- In women - polycystic ovary syndrome, birth of a child weighing more than 4 kg, gestational diabetes
- BP > 140/90 or therapy for hypertension
- HDL cholesterol < 0.9 mM/l and/or triglycerides > 2.82 mM/l
- Testing for prediabetes and diabetes in asymptomatic adults is indicated if they are overweight (BMI greater than 25 kg/m2) and have one or more risk factors for diabetes. If there are no additional risk factors, the test should be performed starting at age 45 at intervals of 3 years.
There are two main types of diabetes mellitus:
- Type 1 diabetes mellitus (insulin-dependent, IDDM) occurs in 10-15% of all diabetic patients. Hyperglycemia develops as a result of insulin deficiency caused by autoimmune destruction of insulin-producing β-cells of the pancreas. The peak incidence was observed at the ages of 3-5 and 11-14 years.
- Type 2 diabetes mellitus (non-insulin dependent, NIDDM) is much more common (80-85% of cases). Hyperglycemia is caused by insulin resistance. The risk of morbidity is observed after 50 years of life.
Main differences between both forms of diabetes
| IDDM ( type 1) | index | NIDDM ( type 2) |
| Up to 30 years old | Patient's age | After 50 years |
| Shortage | Body mass | 80-90% obesity |
| Acute | Onset of the disease | Gradual |
| Spring-winter period | Seasonality of the disease | Absent |
| Labile | Course of diabetes | Stable |
| Tendency to ketoacidosis | Ketoacidosis | Not developing |
| High hyperglycemia | Blood analysis | Moderate hyperglycemia |
| Reduced | Insulin and C-peptide in the blood | Normal, often elevated |
| Detected in 80-90% in the first weeks of the disease | Autoantibodies to the islets of Langerhans Autoantibodies to insulin Autoantibodies to glutamic acid decarboxylase | None |
| HLA DR3-B8, DR4-B15, C2-1, C4, A3, Dw4, DQw8 | Immunogenetics | No different from healthy ones |
In addition to type 1 and type 2 diabetes, there are other specific types of diabetes. Diabetes mellitus in such patients is a consequence of a certain primary disease (genetic or acquired), and this form of diabetes is often called secondary diabetes mellitus. The main causes are the following diseases:
- Genetic defects in β-cells or insulin action;
- Acromegaly (gigantism): GH interferes with the uptake of glucose into fat and muscle tissue by suppressing the action of insulin;
- Pheochromocytoma: the action of catecholamines is aimed at mobilizing glucose from the depot and suppressing the effects of insulin;
- Itsenko-Cushing syndrome: excessive secretion of cortisol inhibits glucose uptake in many tissues;
- Chronic pancreatitis or surgery on the pancreas causes tissue damage to the pancreas (including β-cells);
- Toxic effects on the pancreas of drugs and chemicals.
A normal pregnancy is accompanied by numerous hormonal changes that predispose to the development of hyperglycemia and, accordingly, to the development of diabetes. Up to 14% of pregnant women suffer from transient diabetes.
DIAGNOSIS OF DIABETES MELLITUS The task of a laboratory examination if diabetes is suspected is to identify or confirm the presence of absolute or relative insulin deficiency in the patient. The main biochemical signs of insulin deficiency are: fasting hyperglycemia or an abnormal increase in glucose levels after meals, glycosuria and ketonuria. In the absence of symptoms, laboratory results alone provide an accurate diagnosis. The WHO Expert Committee recommends screening for the presence of diabetes in the following categories of citizens: 1) All patients over the age of 45 years (if the test result is negative, it is repeated every three years). 2) Younger patients with:
- Obesity;
- Hereditary burden of diabetes;
- High-risk ethnic/racial background;
- History of gestational diabetes mellitus;
- The birth of a child weighing more than 4.5 kg;
- Arterial hypertension;
- Previously identified impaired glucose tolerance or high fasting glycemia;
Blood glucose testing Testing the concentration of glucose in the blood is the most common method for diagnosing diabetes. Glucose is evenly distributed between plasma and blood cells, with some excess of its concentration in plasma. The glucose content in arterial blood is higher than in venous blood, which is explained by the continuous use of glucose by the cells of tissues and organs. This explains the advantage of studying glucose in plasma or serum of venous blood over its determination in capillary blood for diagnosing diabetes. Venous blood additionally reflects such an important point as the use of glucose by cells of tissues and organs. Therefore, for the diagnosis of diabetes, it is preferable to determine glucose in venous blood.
Reference values for blood glucose concentrations
| Age | Glucose concentration in blood plasma, mmol/l | mg/dl |
| newborns | 2,8 — 4,4 | 50 — 115 |
| children | 3,9 — 5,8 | 70 — 105 |
| adults | 3,9 — 6,1 | 70 — 110 |
Glycosylated hemoglobin Glycosylated hemoglobin is formed as a result of a non-enzymatic reaction between hemoglobin A contained in red blood cells and serum glucose. The degree of glycosylation of hemoglobin depends on the concentration of glucose in the blood and on the duration of contact of glucose with hemoglobin (the lifespan of a red blood cell). Red blood cells circulating in the blood have different ages, therefore, to average the level of glucose associated with it, we focus on the half-life of red blood cells (60 days). There are at least three variants of glycosylated hemoglobins: HbA1a, HbA1b, HbA1c, but only the latter variant quantitatively predominates and gives a closer correlation with the severity of diabetes mellitus. The results of the study of glycosylated hemoglobin are assessed as follows:
- 4-6% indicate good compensation of diabetes in the last 1-2 months,
- 6.2-7.5% – satisfactory level,
- above 7.5% – unsatisfactory.
Unlike glucose, the level of glycosylated hemoglobin does not depend on physical activity, food intake, medications, or the patient’s emotions.
Relationship between blood glucose concentrations and glycosylated hemoglobin levels
| Glycosylated hemoglobin level | Blood glucose concentration | |
| mmol/l | mg/dl | |
| 4,0 | 2,6 | 50 |
| 5,0 | 4,7 | 80 |
| 6,0 | 6,3 | 115 |
| 7,0 | 8,2 | 150 |
| 8,0 | 10,0 | 180 |
| 9,0 | 11,9 | 215 |
| 10,0 | 13,7 | 250 |
| 11,0 | 15,6 | 280 |
| 12,0 | 17,4 | 315 |
| 13,0 | 19,3 | 350 |
| 14,0 | 21,1 | 380 |
Glucose tolerance test The most informative method for diagnosing diabetes is considered to be the dynamics of changes in the level of glucose in the blood of patients in response to a sugar load - the glucose tolerance test (glucose tolerance test). A glucose tolerance test should be performed in patients if the fasting plasma glucose level is from 6.1 to 7.0 nmol/l, as well as in persons with identified risk factors for the development of diabetes (diabetes mellitus in close relatives, birth of a large fetus, impaired tolerance history of glucose deficiency, obesity, hypertension). To carry out the test, the patient must receive a diet containing at least 125 g of carbohydrates for 3 days (all hospital food tables meet this requirement). The test is carried out in the morning after 10-14 hours of fasting. An initial blood sample is taken on an empty stomach, then the patient takes 75 g of glucose dissolved in 200 ml of water, and the child takes 1.75 g of glucose per 1 kg of weight, but not more than 75 g. The blood is taken again after 120 minutes and the samples are examined for glucose content (interpretation of test results, see below).
Examination of urine for glucosuria In healthy people, glucose entering the primary urine is almost completely reabsorbed in the renal tubules and is not determined in urine by conventional methods. When the glucose concentration increases above the renal threshold (8.88-9.99 mmol/l), glucose begins to enter the urine and glucosuria occurs. Glucose can be detected in the urine in two cases: with a significant increase in glycemia and with a decrease in the renal threshold for glucose - renal diabetes. In patients with diabetes mellitus, glucosuria is studied to assess the effectiveness of treatment and as an additional criterion for compensation of diabetes:
- In type 1 diabetes mellitus, urinary loss of 20-30 g of glucose per day is allowed.
- The criterion for compensation of type 2 diabetes mellitus is the achievement of aglucosuria.
Determination of glucose in urine is not usually used to diagnose diabetes mellitus. Moreover, with age, the renal threshold for glucose increases and in older people can be above 16.6 mmol/l before glucosuria appears.
Autoantibodies Currently, IDDM is considered an autoimmune disease with destruction of β-cells of the pancreatic islets. Inducers of the autoimmune process in type 1 diabetes mellitus include Coxsackie B viruses, mumps, encephalomyelitis, rubella, etc. The detection of autoantibodies to islet cell antigens has the greatest prognostic significance in the development of type 1 diabetes mellitus. They appear 1-8 years before the clinical manifestation of diabetes. Their identification allows the clinician to diagnose prediabetes, select a diet and carry out immunocorrective therapy. Carrying out such therapy plays an extremely important role, since clinical symptoms of insulin deficiency in the form of hyperglycemia and associated complaints appear when 80-90% of insulin-producing β-cells are affected, and the possibilities of immunocorrective therapy during this period are limited. The high level of autoantibodies in the preclinical period and at the beginning of the clinical period gradually decreases over several years, until complete disappearance. The use of immunosuppressants in the treatment of type 1 diabetes also leads to a decrease in the level of autoantibodies.
Antibodies to insulin Antibodies to insulin belong to the IgG class. Antibody levels can be elevated in 35-40% of patients with newly diagnosed type 1 diabetes (i.e. not treated with insulin) and in almost 100% of children within 5 years from the time of onset of IDDM. The appearance of autoantibodies to insulin is based on hyperinsulinemia, which occurs in the initial stage of the disease, and the reaction of the immune system. Therefore, the determination of autoantibodies can be used to diagnose the initial stages of diabetes, its debut, erased and atypical forms (sensitivity - 40-95%, specificity - 99%). After 15 years from the onset of diabetes, autoantibodies to insulin are found in only 20% of patients. Long-term insulin therapy usually causes an increase in the number of circulating antibodies to the administered insulin drug. Autoantibodies are the cause of insulin resistance. However, there is not always a direct relationship between the level of antibodies and the degree of insulin resistance. Autoantibodies can also be detected in patients treated with oral antidiabetic drugs (in particular bucarban, glibenclamide). Determination of the level of autoantibodies can be used to assess the risk of developing diabetes over 5 years in first-degree relatives. In the presence of autoantibodies more than 20 units. The risk increases almost 8 times and is 37%; when autoantibodies to islet cell antigens and insulin are combined, it reaches 50%. The main antigen representing the main target for autoantibodies associated with the development of IDDM is glutamic acid decarboxylase, a β-cell membrane enzyme. Antibodies to glutamic acid decarboxylase (anti-GAD) are a very informative marker for diagnosing prediabetes, as well as identifying individuals at high risk of developing IDDM (sensitivity - 70%, specificity - 99%). Elevated levels of anti-GAD can be detected in patients 7-14 years before clinical manifestations of the disease. Over time, the level of anti-GAD decreases, and after years, antibodies are detected in only 20% of patients. Anti-GAD is found in 60-80% of patients with type 1 diabetes; their detection in patients with type 2 diabetes indicates the involvement of autoimmune mechanisms in the pathogenesis of the disease and serves as an indication for immunocorrective therapy.
Criteria for diagnosing diabetes mellitus Diabetes mellitus can be diagnosed if one of the following criteria is present:
- Clinical symptoms of diabetes (polyuria, polydipsia, unexplained weight loss) and an incidentally detected increase in plasma glucose concentration ≥11.1 mmol/l (≥200 mg%).
- Fasting plasma glucose level (no food intake for at least 8 hours) – ≥ 7.1 mmol/l (≥ 126 mg%).
- 2 hours after an oral glucose load (75 g glucose) – ≥ 11.1 mmol/l (≥ 200 mg%).
Diagnostic criteria for diabetes mellitus and other categories of hyperglycemia
| Category | Glucose concentration, mmol/l | |||
| Whole blood | Plasma | |||
| venous | capillary | venous | capillary | |
| Diabetes mellitus: on an empty stomach and/or 120 minutes after taking glucose | >6,1 >10,0 | >6,1 >11,1 | >7,0 >11,1 | >7,0 >12,2 |
| Impaired glucose tolerance: on an empty stomach and 120 minutes after ingestion of glucose | <6,1 6,7 — 10,0 | <6,1 7,8 — 11,1 | <7,0 7,8 — 11,1 | <7,0 8,9 — 12,2 |
| Impaired fasting glucose: fasting 120 min after glucose intake | 5,6 — 6,1 <6,7 | 5,6 — 6,1 <7,8 | 6,1 — 7,0 <7,8 | 6,1 — 7,0 <8,9 |
WHO recommends using only venous plasma test results to make a diagnosis of diabetes mellitus
- normal fasting plasma glucose levels are up to 6.1 mmol/l (<110 mg%);
- fasting plasma glucose levels from 6.1 mmol/l (≥110 mg%) to <7.0 mmol/l (<128 mg%) are defined as impaired fasting glucose;
- fasting plasma glucose level > 7 mmol/l (> 128 mg%) is regarded as a preliminary diagnosis of diabetes mellitus, which must be confirmed according to the above criteria.
When conducting a glucose tolerance test, the following indicators are important:
- Normal glucose tolerance is characterized by a plasma glucose level 2 hours after a glucose load of <7.8 mmol/L (<140 mg%);
- An increase in plasma glucose concentration 2 hours after a glucose load ≥ 7.8 mmol/L (≥ 140 mg%), but below 11.1 mmol/L (<200 mg%) indicates impaired glucose tolerance;
- A plasma glucose level 2 hours after an oral glucose load > 11.1 mmol/l (> 200 mg%) indicates a preliminary diagnosis of diabetes mellitus, which must be confirmed according to the criteria given above.
To evaluate the results of the glucose tolerance test, 2 indicators are calculated: hyperglycemic and hypoglycemic coefficients:
- Hyperglycemic – the ratio of glucose content after 30 or 60 minutes (the largest value is taken) to its level on an empty stomach. Normally, this coefficient should not be higher than 1.7.
- Hypoglycemic – the ratio of glucose levels after 2 hours to its fasting level. Normally, this coefficient should be less than 1.3.
If the patient does not have impaired glucose tolerance, but the value of both or one of the coefficients exceeds normal values, the glucose load curve is interpreted as “doubtful”. Such a patient should be advised to abstain from carbohydrate abuse and repeat the test after 1 year.
Recommended laboratory tests to establish the diagnosis of DIABETES MELLITUS
First level tests Blood
- The amount of glucose in venous blood
- Amount of glucose after exercise (vein)
- Glycosylated hemoglobin
- Fructosamine
Urine
- Amount of glucose
- Acetone in urine
Second level tests (differential diagnosis of diabetes)
- Blood insulin level
- Blood C-peptide level (fasting)
- Autoantibodies to cells of the islets of Langerhans
- Autoantibodies to insulin
- Autoantibodies to glutamic acid decarboxylase
- Immunogenetic typing (HLA)
- DR3-B8
- DR4-B15
- B15
- DR4
- Dw4
Third level tests (diagnosis of diabetes complications) Hypoglycemic coma
- Blood insulin level
- Blood glucose level
Diabetic nephropathy (tests at least once every 4-6 months)
- Microalbuminuria
- Protein in urine (proteinuria)
- Study of 24-hour urine protein (rate of increase in proteinuria)
- Rehberg test (creatinine clearance)
- Hypercreatininemia
- Hypoalbuminemia
- Apolipoprotein A1
- Apolipoprotein B (Apo B)
- Triglycerides
- Cholesterol
- HDL cholesterol
- LDL cholesterol
Diabetic macroangiopathy
- Hyperglycemia
- Hyperinsulinemia
- Total cholesterol (increased levels)
- Triglycerides (increased levels)
- High density lipoproteins
- Accelerated thrombus formation (see “diagnosis of thrombophilia”)
- Microalbuminuria
- Proteinuria
Plan for laboratory examination of a patient diagnosed with DIABETES MELLITUS
Laboratory tests at the first visit and at annual follow-up Blood
- The amount of glucose in plasma
- Amount of glucose after exercise
- Glycosylated hemoglobin
- Fructosamine
- Apolipoprotein A1
- Apolipoprotein B (Apo B)
- Triglycerides
- Cholesterol
- HDL cholesterol
- LDL cholesterol
- Creatinine
- Electrolytes (K/Na/Cl)
- Blood insulin level
- Blood C-peptide level
Urine
- Glucosuria
- Acetone in urine
- Microalbuminuria
- Ketonuria
- Bacteriuria
- Urine sediment
Laboratory tests at follow-up visit (every 3 months) Blood
- The amount of glucose in plasma
- Amount of glucose after meals
- Glycosylated hemoglobin
- Triglycerides
- Cholesterol
- HDL cholesterol
- LDL cholesterol
Urine
- Glucosuria
- Proteinuria
Assessing the effectiveness of diabetes treatment (diabetes compensation criteria)
| Laboratory indicators | Criteria for compensation of diabetes mellitus | ||
| DIABETES MELLITUS, TYPE 1 | optimal | satisfactorily | unsatisfactory |
| Glycemic profile | |||
| Fasting glycemia, mmol/l | 4,0 — 5,0 | 5,1 — 6,5 | >6,5 |
| Glycemia after meals (peak), mmol/l | 4,0 — 7,5 | 7,6 — 9,0 | >9,0 |
| Glycemia before bedtime, mmol/l | 4,0 — 5,0 | 6,0 — 7,5 | >7,5 |
| Glycosylated hemoglobin,% | <6,1 | 6,2 — 7,5 | >7,5 |
| Lipid profile | low risk | moderate risk | high risk |
| Total cholesterol, mmol/l | <4,8 | 4,8 — 6,0 | >6,0 |
| LDL-C, mmol/l | <3,0 | 3,0 — 4,0 | >4,0 |
| HDL-C, mmol/l | >1,2 | 1,0 — 1,2 | <1,0 |
| Triglycerides, mmol/l | <1,7 | 1,7 — 2,2 | >2,2 |
| DIABETES MELLITUS, TYPE 2 | optimal | satisfactorily | unsatisfactory |
| Glycemic profile | |||
| Fasting blood glucose (capillary blood), mmol/l | <5,5 | >5,5 | >6,0 |
| Glycemia after meals (peak, capillary blood), mmol/l | <7,5 | >7,5 | >9,0 |
| Fasting glycemia (venous blood plasma), mmol/l | <6,0 | >6,0 | >7,0 |
| Glycosylated hemoglobin,% | <6,5 | >6,5 | >7,5 |
| Lipid profile | low risk | moderate risk | high risk |
| Total cholesterol, mmol/l | <4,8 | 4,8 — 6,0 | >6,0 |
| LDL-C, mmol/l | <3,0 | 3,0 — 4,0 | >4,0 |
| HDL-C, mmol/l | >1,2 | 1,0 — 1,2 | <1,0 |
| Triglycerides, mmol/l | <1,7 | 1,7 — 2,2 | >2,2 |
Types of blood glucose curves during the glucose tolerance test. Changes in glucose concentration during hyperinsulinism (1); in healthy individuals (2); with thyrotoxicosis (3); with mild form (4) and severe form (5) of diabetes mellitus.
Laboratory diagnosis of complications of diabetes mellitus Diabetic nephropathy (DN) is currently the leading cause of high morbidity and mortality in patients with diabetes. The frequency of its development ranges from 40 to 50% in patients with insulin-dependent diabetes (IDDM) and from 15 to 30% in patients with non-insulin-dependent diabetes (NIDDM). The danger of this complication is that developing quite slowly and gradually, DN goes unnoticed for a long time, since clinically it does not cause a feeling of discomfort in the patient. And only at a pronounced (often terminal) stage of kidney pathology does the patient develop complaints related to intoxication of the body with nitrogenous wastes; however, at this stage it is not always possible to radically help the patient. Therefore, the main task of a general practitioner, endocrinologist or nephrologist is to timely diagnose DN and carry out adequate pathogenetic therapy as early as possible. In the pathogenesis of DN, changes that develop in the structure of the glomerular basement membrane and capillaries are important, which leads to disruption of hemodynamic parameters of renal function. They manifest themselves in an increase in glomerular filtration rate during the period of manifestation and the first years of diabetes. Due to relaxation of the afferent and narrowing of the efferent arterioles, intraglomerular pressure increases, which has a damaging effect on the surface of endothelial cells, both through increased mechanical stress and through an increase in the permeability of the basement membranes of the glomerular capillaries for lipids and various protein components of the plasma. Disruption of the normal structure of the glomerular barrier contributes to the proliferation of mesothelial cells with the deposition of lipids and proteins, thickening of the basement membrane, increased formation of the extracellular matrix and sclerosis of the renal tissue. As sclerotic changes progress, glomerular occlusion and renal tubular atrophy develop. Hyperfiltration (more than 140 ml/min/1.73 m2), observed in the initial stages of DN, is replaced by hypofiltration, which is accompanied by an increase in creatinine and urea in the blood serum and the appearance of clinical symptoms of renal failure. DN in the first years after the manifestation of diabetes occurs latently. This period lasts about 10-15 years, and only then does proteinuria, clinical signs of renal failure appear, and at the end of the disease - symptoms of uremia, combined with anemia, acidosis, and arterial hypertension.
Classification of stages of development of diabetic nephropathy (according to Mogensen S. E.)
| Stage of diabetic nephropathy | Clinical and laboratory characteristics | Development timeframe |
| Hyperfunction of the kidneys | increased GFR (> 140 ml/min); PC increase; kidney hypertrophy; normoalbuminuria (<30 mg/day). | In debut |
| Stage of initial structural changes in kidney tissue | thickening of the basement membranes and capillaries of the glomeruli; expansion of the mesangium; high GFR remains; normoalbuminuria. | After 2 - 5 years |
| Beginning nephropathy | microalbuminuria (from 30 to 300 mg/day); GFR is high or normal; unstable increase in blood pressure; | In 5 - 15 years |
| Severe nephropathy | proteinuria (more than 500 mg/day); GFR is normal or moderately reduced; arterial hypertension. | In 10 - 25 years |
| Uremia | decreased GFR < 10 ml/min; arterial hypertension; symptoms of intoxication. | After 20 or more years or after 5 - 7 years from the onset of proteinuria |
Algorithm for screening and management of diabetic nephropathy (from the moment of diagnosis)
| Test | Frequency | Acceptable Next steps | |
| Microalbuminuria | 1 time per year | < 20 mg/l | 20 mg/l Rule out other diseases (infections, heart failure) Determine daily albumin excretion |
| Rate of daily albumin excretion | 1 time per year | <15 µg/min | 15 – 200 mcg/min – if blood pressure is elevated, start treatment > 200 mcg/min – determine serum creatinine |
| Serum creatinine | Age norm | <120 – control once every 6 months 120 – 200 – control once every 3 months 200 – 450 – management together with a nephrologist >450 – management by a nephrologist | |
Prevention and treatment of type 2 diabetes
Endocrinology uses a systematic approach to therapy. In the initial stages of the disease, the greatest attention is paid to consultations and changes in the patient’s lifestyle (attempts to control sugar). If such treatment does not help, then a decision is made to use drug treatment. The complex of treatment procedures includes:
- • Diet. The main principle of the diet is to reduce foods high in carbohydrates and fats. The most dangerous are products with refined sugar (confectionery, candy, chocolate, lemonade). The diet should consist of vegetables, milk, meat, eggs and grains. The diet should be fractional (5-6 times a day), portions should be small;
- • Physical exercise. If the patient does not yet have severe complications, then sports activities are indicated for him. The duration and intensity of training is selected individually. Patients are usually recommended to exercise walking, swimming and walking;
- • Drug treatment. Several groups of drugs are used. To reduce insulin resistance of cells, the absorption of glucose in the gastrointestinal tract and its production in the liver, the use of biguanides and thiazolidinediones is allowed. If the use of these drugs is not enough, drugs that enhance insulin activity are prescribed.
Timely diagnosis, an experienced endocrinologist and correctly prescribed treatment (including diet) are the key to successful treatment of the disease. Our multidisciplinary Sante Clinic employs experienced endocrinologists (PhD) who will help you maintain your health with diabetes mellitus type 1 and 2. Without queues, long waits “by appointment” and postponed appointments - we are waiting for you at Sante Clinic!
To the Endocrinologist
Treatment
In type 2 diabetes, insulin is used only in advanced cases. It can be administered in short courses during hospital treatment, but this does not mean that at home you will also be tied to injections. Proper nutrition and physical activity are extremely important for diabetes.
Is there a cure for type 2 diabetes?
The situation is potentially reversible at the stage of metabolic syndrome and prediabetes - a borderline state between normal and pathological, when you can return glucose levels to normal levels if you lose weight, exercise and start eating right. But if diabetes has already developed, then this diagnosis will stay with you forever.
Drug treatment
Commonly prescribed medications for type 2 diabetes include:
- metformin (reduces glucose production in the liver, increases cell sensitivity to insulin),
- sulfonylureas and meglitinides (help the pancreas secrete more insulin),
- Thiazolidinediones (help insulin work, but have side effects - risk of weight gain, heart failure and liver disease).
In later stages of diabetes, regular insulin injections may be required. The insulin dose may increase over time. Read more about insulin therapy in the article “Type 1 Diabetes.”
Diet
“Patients with diabetes are advised to exclude watermelons - they are too sweet, which means they contribute to an increase in blood glucose levels,” explains Professor Leonid Yulievich Morgunov, “but if you love them so much that you cannot refuse them, please eat, but in small quantities. Those who receive insulin should adjust their dose upward if they allow themselves to enjoy watermelon or grapes, or eat a heavier meal. Patients are taught the ability to calculate the dose of insulin depending on the amount and nature of food eaten at Diabetes Schools. This is a very important skill! In fact, we are trying to artificially recreate the natural mode of insulin production by the pancreas. We prescribe the patient long-acting insulin, which ensures the basic level of this hormone in the body, and “pin up” short-acting insulin during meals, when a healthy person has a peak release of insulin into the blood by the pancreas.”
"What can I eat?" is the first question that people with diabetes ask when they are diagnosed.
Experts believe that such patients do not need a diet, but a healthy eating system individually selected by a nutritionist. The main thing is not to exceed the daily calorie intake and the amount of carbohydrates, especially fast ones (sugar, pastries, white bread, sweets and sweet fruits). The Diabetes School will help you create an individual nutrition program, which you must attend annually. Information about classes at such a school can be obtained from the district clinic or endocrinology clinic.
If a diabetic is not overweight, his caloric intake should not differ from the norm. True, there is one nuance: a person who is not burdened with illnesses usually does not think about what components his food consists of, but for a diabetic patient this information is vital. Knowing exactly the nutrient content of foods is necessary to control their consumption throughout the day.
The Diabetes Plate Method is widely used as a basic nutrition guide and provides a clear, visual approach to calorie management (Figure 2).
Figure 4. Diabetic plate method (diameter 22-23 cm). Source: ifong/Depositphotos
Important! For diabetic patients who are not overweight, a physiological diet containing 60% carbohydrates, 24% fats and 16% proteins of the total daily calorie intake is recommended.
Diabetes is often accompanied by obesity, so the main goal of nutritional therapy for many patients with type 2 diabetes is to adjust their weight. A reduced-calorie diet helps normalize carbohydrate and fat metabolism. At the same time, blood sugar levels decrease and the need for medications may disappear.
Important! The main rule of a diet for diabetes: daily caloric intake must correspond to energy expenditure. It may be a little less, but in no case should it exceed them, this will lead to obesity and aggravate the course of the disease.
Physiotherapy
Regular physical activity is an important part of diabetes treatment and prevention. Don’t go to extremes: don’t give up, but don’t bring yourself to the point of fainting with exhausting workouts. Talk to your doctor or gym trainer about what cardio and strength exercises are appropriate for your weight, joint condition, age and lifestyle.
Physical activity helps you lose weight and normalize carbohydrate metabolism, reversing developing diabetes at its very beginning. If the disease has already progressed far enough and required a switch to insulin therapy, then its combination with physical activity allows for better control of glycemic levels.
Important! You will have to abstain from training if your glycemia is above 15 mmol/l until this figure normalizes. Ask your doctor to choose an individual set of exercises, use every opportunity to move more.
What types of physical activity do you prefer?
In the initial stages of diabetes (fasting sugar 6.7–7.8 mmol/l), breathing and regular exercises, walking at a comfortable pace for a distance of at least two, but not more than ten kilometers, are useful. You can exercise with dumbbells and weight machines, but the weight should be light. Do you like skiing and skating? Great! In winter, diversify your physical activity with them. And don't forget about swimming - this is the best sport for diabetics.
With an advanced form of diabetes (7.8–14 mmol/l), the exercise program remains the same - walking and gymnastics for all muscle groups. Do relaxation exercises more often and avoid fatigue!
Carefully monitor the parameters of your body during independent physical exercise:
- use a glucometer to measure your sugar level before and after training (Fig. 3) and record the dynamics of changes in a special diary;
- if you are switched to insulin therapy, inject insulin before starting exercise;
- monitor your heart rate (not higher than 120 beats per minute);
- record at what minute of exercise fatigue occurred: this is a reason to end the workout.
Figure 5. Glucometer for determining the amount of glucose in the blood. Source: Amanda Mills/USCDCP/Pixnio
Folk remedies. Are they effective?
To a certain extent, herbal medicine helps normalize glucose levels. For example, green tea reduces cravings for sweets and has a slight hypoglycemic effect. Infusions of rose hips, bean pods, dandelion root, blueberry leaves, blueberries, strawberries and blackberries (as well as their berries themselves), mulberry (mulberry) and walnuts, galega herb (goat's rue), lungwort, and nettle have a similar effect. dioecious, St. John's wort, common chicory, bird's eye buckwheat, elecampane, common vetch, horsetail, adonis. Although herbs alone cannot cure diabetes, they can be used as an addition to the main treatment prescribed by your doctor.
The myth of Jerusalem artichoke
Among patients with diabetes, there is a widespread belief that Jerusalem artichoke fruits reduce blood glucose levels (Fig. 3). It happened because this plant contains a substance called “inulin”. Sounds almost like “insulin”! However, phonetic similarity does not mean a similar effect, since inulin is a polysaccharide, not a hormone. Therefore, a diabetic patient can eat Jerusalem artichoke, but one cannot expect a sugar-lowering effect from the earthen pear.