Published: 08/13/2021 10:52:00 Updated: 08/13/2021
Hypoglycemia refers to a decrease in blood glucose levels to critical values. This is a dangerous condition that leads to disruption of the brain’s internal organs, and in a severe stage – to irreparable consequences or death due to hypoglycemic coma.
The symptoms of this condition are varied and depend on the cause of the pathology and the characteristics of the individual patient. Timely diagnosis and control of sugar concentrations make it possible to prevent serious complications and maintain the usual way of life.
Causes of hypoglycemia
A decrease in blood sugar levels is not a disease, but a condition that occurs due to a number of disorders of carbohydrate metabolism in the body.
Glucose, as a source of energy, determines the functioning of internal organs and the condition of a person as a whole. The brain is especially sensitive to a drop in sugar concentration. It works more intensively than all other organs, consumes an increased amount of “fuel”, is not able to store it and therefore is completely dependent on the continuous supply of glucose through the bloodstream.
In the body of a healthy person, excess glucose from carbohydrates received from food is stored in the liver in the form of glycogen - a molecule consisting of many interconnected glucose molecules, which, if necessary, is broken down and absorbed into the blood. This ensures the smooth functioning of organs. Thus, any liver pathology can lead to hypoglycemia.
In addition, hormones significantly influence glucose metabolism:
- pancreas: insulin (responsible for the accumulation of glucose in the form of glycogen and reducing its level in the blood) and glucagon (stimulates the breakdown of glycogen, which causes an increase in sugar levels);
- adrenal glands: adrenaline, cortisol, growth hormone (increases sugar);
- thyroid gland: thyroxine and triiodothyronine (increase sugar).
Hypoglycemia is most often observed in diabetes mellitus.
On the one hand, the patient takes glucose-lowering medications. On the other hand, glucose from the liver enters the blood slowly. This leads to the fact that at some point the sugar concentration may drop to critically low values. This condition also occurs as a result of diseases of the gastrointestinal tract with impaired absorption of glucose, renal failure (increased excretion of sugar in the urine), cancer of the pancreas and some congenital pathologies.
Hypoglycemia resulting from disease is called pathological. In contrast, physiological hypoglycemia develops in healthy people during fasting, dehydration, emotional stress or excessive physical activity, taking certain drugs and alcohol.
In women, hypoglycemia is sometimes observed during pregnancy due to the fact that part of the mother's glucose is spent on fetal development. Hypoglycemia in children develops in the first hours or days after birth and can be temporary or permanent. Risk factors include prematurity, maternal diabetes, birth asphyxia, and congenital pancreatic anomalies.
Type 2 diabetes – what is it?
The content of the article
The most common form of diabetes is type 2 diabetes, also called adult-onset diabetes or non-insulin-dependent diabetes. The dominant symptoms of this disease are abnormal blood glucose levels accompanied by insulin resistance.
With insulin resistance, the body produces a lot of this hormone, but the tissues are less sensitive to its effects.
Genetic predisposition, as well as modifiable factors, that is, those that we influence, are responsible for the development of the disease. Although the tendency to develop the disease is hereditary, diabetes can be caused by an unhealthy lifestyle.
Abdominal obesity contributes to the development of insulin resistance, as well as:
- increased levels of triglycerides and cholesterol;
- hypertension;
- low physical activity;
- age (the risk of developing the disease increases with age);
- chronic sleep disorders;
- past gestational diabetes;
- smoking and drinking alcohol.
Low physical activity
Genetic factors and a family history of type 2 diabetes increase the risk of developing this disease. The Diabetes Association recommends that people at risk should be screened annually for diabetes. Healthy people over 45 years of age should do this once every three years.
Symptoms and types of hypoglycemia
Hypoglycemia is characterized by various symptoms, the nature and severity of which depend on the individual patient and the cause of the pathology.
The main signs of this condition include obsessive hunger, increased sweating, nausea and vomiting, weakness, tremors in the limbs, rapid heartbeat, decreased concentration, drowsiness, visual disturbances (blurred vision, double vision and “gnats” in the eyes), panic and anxiety, paleness of the face.
There are three types of hypoglycemia based on severity:
- Mild (a person is able to independently help himself by consuming sweet drinks and sugar-containing foods).
- Moderate severity (the person remains conscious, but needs the help of third parties to normalize blood sugar levels).
- Severe (a hypoglycemic coma occurs, the person is unconscious and needs urgent hospitalization).
Complications of diabetes
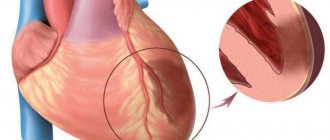
Diabetes mellitus leads to decreased immunity. As a result, the patient more often suffers from various diseases, the recovery process is delayed, and the diseases often become chronic. The healing of various wounds (cuts, abrasions) is worse. Nervous tissue and blood vessels suffer. The development of atherosclerosis is stimulated, the vessels of the eyes and kidneys are affected, and the blood supply to the skin is disrupted. The combination of disorders of various systems leads to a complex of complications called diabetic foot syndrome. The foot, due to its peripheral position, turns out to be the most vulnerable - pathological changes caused by diabetes can lead here to inflammatory processes, ulcers, and tissue necrosis. In advanced cases, amputation may be required.
ketoacidosis , are dangerous
– accumulation of products of intermediate metabolism of fats (acetone) in the blood. Ketoacidosis is characteristic of type 1 diabetes.
Diagnosis of hypoglycemia
The signs of this condition are quite characteristic, and the primary diagnosis is most likely made after a conversation with the patient and his examination.
The only difficulty is finding out the true cause of this pathology. Therefore, a wide range of laboratory and instrumental examination methods are used for diagnosis. First of all, if hypoglycemia is suspected, a blood test is performed to check the sugar level, which in this condition drops below 3.5 mmol/l. This test may produce biased results because many factors, including time of day, affect sugar concentrations.
The determination of glycosylated hemoglobin (HBA1c) is of great diagnostic importance. This is a stable combination of hemoglobin A with glucose in red blood cells: the more glucose in the blood, the higher the level of HBA1c. Throughout the life of a red blood cell (120 days), this compound continues to circulate in the blood, and determining the concentration of HBA1c allows us to reveal the true concentration of glucose over the last two to three months.
In order to establish the cause of hypoglycemia, a blood test is performed for hormones (in particular, the thyroid gland and adrenal glands), the presence of excess alcohol and medications, a urine test, a biopsy of the liver and pancreas to confirm insufficient production of enzymes, ultrasound, MRI and CT scan of internal organs.
The first signs of type 2 diabetes
Although doctors have been saying for years that preventive screenings are a chance for early detection of the disease or prediabetes, patients rarely follow these recommendations. For this reason, the disease is often diagnosed at a late stage.
This is also because the symptoms of type 2 diabetes are quite varied and at the same time not very specific. The disease can develop undetected for many years. Therefore, it is worth carefully monitoring your health and quickly responding to suspicious symptoms.
Treatment of hypoglycemia
First of all, when signs of this condition appear, it is necessary to provide the body with glucose.
Conscious patients should be given quickly digestible carbohydrates: sweet drinks (fruit juice, compote, tea, sweetened water) and sweets (sweets, marmalade, honey, pure sugar). In cases of moderate severity, a glucose/dextrose solution is administered intravenously and/or subcutaneously, glucagon is administered subcutaneously or intramuscularly.
For hypoglycemic coma, droppers with saline, insulin and electrolytes are used.
First of all, medical care for hypoglycemia is aimed at treating the underlying disease that caused the pathology.
Weight change
In type 1 diabetes, patients experience noticeable weight loss. The opposite situation occurs in people with type 2 diabetes. High concentrations of insulin increase appetite and stimulate the body to store fat, which adds pounds. And this happens despite no changes in diet.
Prevention of hypoglycemia
Simple and effective recommendations allow the patient to control their condition and live a full life:
- strictly adhere to the diet (healthy diet without long breaks between meals), as well as sleep, exercise, and taking prescribed hypoglycemic and other medications;
- Constantly monitor sugar levels (measurement with a glucometer at home, repeated tests for glycosylated hemoglobin every 3 months);
- learn to clearly identify signs of low glucose levels, always carry sweet bars with you and notify loved ones about first aid measures in case of an attack.
Author:
Pugonina Tatyana Alekseevna, Therapist
Chronic fatigue and drowsiness
Constantly high levels of glucose, which the body cannot use for work, manifests itself in fatigue and excessive sleepiness. These symptoms may get worse, especially after eating.
When the body receives a large dose of carbohydrates from food, it takes time to balance it with the right amount of insulin. As a result, the patient struggles with so-called hyperglycemia after eating, which decreases after a while.
Constant fatigue can cause mood swings, which over time begin to interfere with daily activities.
Prices
| Name of service (price list incomplete) | Price |
| Appointment (examination, consultation) with a pediatric endocrinologist, primary, therapeutic and diagnostic, outpatient | 1750 rub. |
| Consultation (interpretation) with analyzes from third parties | 2250 rub. |
| Prescription of treatment regimen (for up to 1 month) | 1800 rub. |
| Prescription of treatment regimen (for a period of 1 month) | 2700 rub. |
| Consultation with a candidate of medical sciences | 2500 rub. |
Increased blood sugar detected for the first time: what to do?
1. Don't panic. Stress raises your blood sugar and makes it difficult to make smart decisions.
2. Remember who ordered the analysis and why.
- If the study is prescribed by a doctor, a specialist will evaluate the result and decide on further actions.
- If for some reason you assigned this study to yourself, then most likely there were some reasons for this. Nothing happens by chance. You may be worried about dry mouth, changes in body weight, or maybe new food cravings. Often the idea of controlling sugar is prompted by information that one of your relatives has been diagnosed with diabetes. Sometimes close relatives insist on analysis because they notice your changes: unpleasant body odor, sticky drops of urine in the restroom. If this is the case, then it's time for you to see a doctor.
3. Decide how urgently you need to seek medical help.
- If the excess of the norm is tenths, then it would not be amiss to repeat the analysis after preliminary preparation and/or examine glycosylated hemoglobin.
- If blood sugar is 11.0 or higher, then a consultation with a therapist should be scheduled immediately. Why not immediately see an endocrinologist, you ask. My answer is that consultation with a therapist is more accessible, and it will prepare you for an effective visit to a specialist. If the doctor deems it necessary, he will receive a preliminary consultation with an endocrinologist and prescribe treatment.
- If sugar is above 7.0, but less than 11.0, then there are several days to understand the situation. However, there is no reason to delay solving the problem. The faster the answers are given, the less stress and the greater the chance of adequate help.
4. Follow the recommendations of a specialist, and do not google a solution on the Internet or look for advice on social networks.
- Firstly, each person is individual, template recommendations can be harmful and lead to diagnostic error.
- Secondly, what works for someone else may not work for you.
- Thirdly, it is necessary to share the responsibility of making decisions for your health with someone who spent 8 years learning to take it upon himself and carry it through the thorns of the medical specialty.
5. Trust a professional.
- Tell about yourself, your problems and complaints, your concerns.
- Together with your doctor, draw up a plan to overcome the situation.
- Be honest about what you are willing to do and what is unacceptable to you, including for financial reasons.
- Ask questions, clarify answers.
6. Win. Defeat the disease, solve problems, move towards your goals.
Be healthy!
about the author
- Ivlieva Evgenia Sergeevna
- Endocrinologist of the first category
- All publications by the author