Where do platelets in the blood come from?
Platelets are made in the bone marrow, as are red blood cells and most white blood cells (leukocytes).
They are formed from very large bone marrow cells called megakaryocytes. As megakaryocytes develop, they undergo a fragmentation process that results in the release of more than 1000 platelets per megakaryocyte. The dominant hormone that controls the development of megakaryocytes is thrombopoietin. The lifespan of one blood plate is about 7-12 days, after which they disintegrate in the spleen or liver. The main role of platelets in the human body is to stop bleeding and hemostasis. When the integrity of the vessel is violated, they are activated. At the same time, they acquire a spherical shape, and processes (pseudopodia) appear on their surface. Next, the platelets come into contact with the damaged inner lining of the blood vessel (endothelium). With the help of these processes, they attach to the site of traumatization of the vessel and are fastened together, forming a blood clot. In this way, platelets prevent blood loss.
Figure 1. Blood clotting. Image: pvproductions/Depositphotos
Additionally, platelets prevent infectious agents from entering the bloodstream by releasing lysozyme and B-lysine. They also take part in the delivery of nutrients to the endothelium. By releasing growth factors, these blood cells help repair the vascular wall. There is evidence that platelets take an active part in the functioning of the immune system.
How does platelet activation occur?
Normally, platelets move along the vascular wall, as if inspecting it. When the integrity of the vessel is damaged, collagen protein enters the blood, with which the platelet interacts using a special receptor. In this case, a whole cascade of reactions occurs inside the platelet, due to which a number of substances are released, and the cell itself changes shape. At the same time, blood platelets begin to attach to the site of injury and connect with each other, forming a primary thrombus¹.
Blood test for platelets
The level of platelets in the blood is measured as part of a complete clinical blood test (CBC).
In Russian public hospitals and clinics, on paper forms the platelet level is labeled with the corresponding word - platelets. In automated analyzers of foreign origin, the most common designation is PLT, short for platelets.
The unit of measurement for platelets is the number of cells per volume of blood. The most commonly used multiplier is 109/L (10 to the 9th power per liter of blood), for example 200x109/L.
Indications for analysis
A general blood test, which includes determining platelet levels, is performed on all patients who seek help from a medical facility, undergo a preventive examination, or are preparing for surgery.
Platelet levels may also be measured in other cases:
- Unexplained bleeding and formation of subcutaneous hematomas.
- Bleeding gums, frequent nosebleeds.
- Heavy, prolonged menstruation.
- Suspicion of a malignant tumor in the body.
- Cardiovascular diseases.
- Some pathologies of the gastrointestinal tract that may be complicated by bleeding, for example, gastric and duodenal ulcers.
- Kidney diseases, such as glomerulonephritis.
- Suspicion of diseases of the blood system, including leukemia.
Preparing for analysis
Platelet levels are measured in the same capillary blood that is collected for the CBC. Accordingly, preparation for the analysis is based on the general rules for a clinical (general) blood test. This includes the following requirements and recommendations:
- Refusal to eat before donating blood. Blood for OAC is collected on an empty stomach, usually in the first half of the day. To obtain reliable results, at least 8 hours must pass between the last meal and blood sampling. In emergency cases, OAC can be performed 4 hours after a light snack with an apple, tea or unsweetened porridge without milk and sugar.
- Minimizing physical and emotional stress. If possible, immediately before the procedure, it is better to rest quietly for 10-15 minutes near the office or in the lobby of the medical facility.
- Avoid drinking alcohol the day before donating blood and tobacco products – 1-2 hours.
- If possible, blood sampling should be carried out 10-14 days after stopping medication. If this is not possible, you must notify the laboratory technician who will evaluate the analysis results.
What drugs can affect platelet levels in the blood?
A number of medications for various applications can affect blood platelet counts. Most often these include:
- Antibiotics.
- Antiallergic drugs (antihistamines).
- Some nonsteroidal anti-inflammatory drugs (NSAIDs) that are used to suppress inflammation and relieve pain: acetylsalicylic acid, ibuprofen.
- Medicines used to treat hypertension, including calcium channel blockers (verapamil).
- Medicines to lower blood cholesterol levels (statins).
- Medicines that prevent intravascular coagulation and blood clots (anticoagulants).
- Antidepressants and other drugs used to treat mental disorders.
- Potency improving agents (sildelafil).
Blood platelet levels
The exact indicators of normal platelet levels in the blood for children and adults vary depending on the equipment and reagents used in the laboratory.
As a rule, the normal value for the patient is indicated next to the results obtained. In most cases, the normal range of platelets in the blood for adult men and women is considered to be from 150 to 400 × 109/l¹. Table 1. Average normal values of platelets in the blood, taking into account the patient’s age
| Age | Reference values |
| Less than 10 days | 99-421×109/l |
| 10 days – 1 month | 150-400×109/l |
| 1-6 months | 180-400×109/l |
| 6 months – 1 year | 160-390×109/l |
| 1-5 years | 150-400×109/l |
| 5-10 years | 180-450×109/l |
| 10-15 years | 150-450×109/l |
| More than 15 years | 150-400×109/l |
General (clinical) blood test: interpretation and norm
A complete blood count provides essential information about the types and numbers of blood cells, especially red blood cells, white blood cells and platelets. Using a general blood test, the treating doctor can detect the nature of symptoms such as weakness, fatigue, and bruising. A complete blood count is used to diagnose anemia, infection and many other disorders.
A general (clinical) blood test includes the following indicators:
- Absolute white blood cell count ( WBC ). White blood cells protect the body from infection. If an infection develops, these cells attack and destroy bacteria, viruses, or other pathogenic organisms. White blood cells are larger in size than red blood cells, but their number is less. When a person gets sick, the number of white blood cells increases very quickly. Sometimes white blood cell counts are used to detect infection or to evaluate the effectiveness of cancer treatment.
- Determination of the ratio of different types of white blood cells (leukogram). The main types of leukocytes are neutrophils, lymphocytes, monocytes, eosinophils and basophils. Counting immature neutrophils, also called band neutrophils, is part of this test. The number of each cell type can provide important information about the health of the immune system. Too high or too low the number of one type of cell may indicate an infection, an allergy or toxic reaction to a drug or chemical, or various diseases such as leukemia.
- Absolute red blood cell count ( RBC ). Red blood cells carry oxygen from the lungs to the rest of the body. They also carry carbon dioxide back to the lungs for exhalation. When the level of red blood cells is low (anemia), the body does not receive enough oxygen. When levels are high (polycythemia), there is a risk of red blood cell clots that can block tiny blood vessels (capillaries), also making it difficult to carry oxygen.
- Hematocrit ( HCT , precipitated red blood cell volume, PCV ). This test measures the volume of blood per red blood cells. For example, a hematocrit value of 38 means that 38% of the blood is red blood cells. Hematocrit and hemoglobin are the two main tests for detecting anemia or polycythemia.
- Hemoglobin ( Hgb ). Hemoglobin molecules are found in red blood cells; they carry oxygen and give the blood its red color. A hemoglobin test measures the level of hemoglobin in the blood and shows how the body copes with transporting oxygen.
- Erythrocyte index. There are three red blood cell indices: mean erythrocyte volume (MCV), mean erythrocyte hemoglobin content (MCH) and mean erythrocyte hemoglobin concentration (MCHC). All of them are calculated using special equipment, and the numbers are derived from other indicators of a general blood test. MCV reflects the size of red blood cells, MCH is the average hemoglobin content in an individual red blood cell, MCHC is the hemoglobin concentration in an individual red blood cell. These indices are used in diagnosing various types of anemia. The red blood cell distribution width (RDW) index is also calculated, which reflects the difference in size and shape between cells.
- Absolute platelet count. Platelets are the smallest type of blood cell. They play an important role in the blood clotting process. If bleeding occurs, the platelets are activated and bind together, forming a plug that prevents bleeding. If the number of red blood cells is insufficient, there is a risk of uncontrolled bleeding. If there is an excess amount, there is a risk of thrombus formation in a blood vessel. In addition, platelets can be involved in the formation of sclerotic plaques on artery walls (atherosclerosis).
- Mean platelet volume ( MPV ). This indicator reflects the average value of the measured platelet volume. MPV is used in conjunction with platelet count to diagnose certain diseases. If the platelet count is normal, the MPV may be low or high.
Your doctor may also order a blood smear microscopy at the same time as your complete blood count, but this is not part of your routine blood test. For this test, a drop of blood is placed on a plate and diluted with dye. The plate is examined under a microscope, noting the number, size and shape of red blood cells, white blood cells and platelets. Differences in the shape or size of blood cells can indicate various diseases, such as leukemia, malaria or sickle cell disease.
A clinical blood test is carried out for the following purposes:
- Finding the cause of symptoms such as fatigue, weakness, fever, bruising, or weight loss
- Diagnosis of anemia
- Establishing the amount of blood lost during bleeding
- Diagnosis of polycythemia
- Diagnosis of infections
- Diagnosis of blood diseases, such as leukemia
- Monitoring the body's response to drug treatment and radiation therapy.
- Monitoring the blood cell response to abnormal bleeding.
- Screening of indicators before surgery.
- Tracking high or low levels is used to detect various diseases, such as high eosinophil levels that may indicate allergies or asthma.
A complete blood count is performed as part of a routine medical examination. A complete blood count provides valuable information about the overall condition of the body and health.
Preparing for the examination
No special preparation required.
How is the examination carried out?
- The shoulder is tightened with an elastic tourniquet to stop the blood flow. The veins under the tourniquet become larger, making it easier to insert the needle.
- The puncture site is cleaned with alcohol.
- The needle is inserted into the vein. Sometimes more than one injection is required.
- A blood collection tube is attached to the needle.
- When enough blood has been collected, the tourniquet is removed.
- After the needle is removed, a cotton swab is applied to the injection site.
- The area should be pressed and a bandage applied.
If a baby's blood is being tested, a heel prick is done instead of drawing blood from a vein.
Feelings during the procedure
A blood sample is taken from a vein in the arm. The forearm is wrapped with an elastic band, so there may be a feeling of tightness. You may not feel any pain from the needle, but sometimes there will be a slight burning sensation or pain.
Complications
When taking blood from a vein, the chance of complications occurring is very small.
- There may be a slight bruise. By pressing the tampon to the puncture site for a few minutes, you can reduce the chance of its occurrence.
- In rare cases, the vein may become swollen, this is called phlebitis. The problem can be treated with several warm compresses.
- Continuous bleeding may occur in patients with blood disorders. Taking medications such as aspirin, warfarin (such as Coumadin), and other blood thinners increases the chance of bleeding. Tell your doctor before taking a sample if you have problems with blood clotting or are taking blood-thinning medications.
results
A complete blood count provides important information about the types of blood cells - red blood cells, white blood cells, platelets - and their numbers. A complete blood count helps determine the cause of various symptoms such as weakness, nausea, bruising and is used in the diagnosis of various diseases - anemia, infections and many others.
Normal results
IMPORTANT! The normal values, or range of normal values, given here are average values. These vary depending on the laboratory, so where you are being tested will have different readings. The laboratory report should contain information about the reference range used. In addition, overall health and other factors are taken into account when analyzing the results. Therefore, a value that does not fit into the range presented here may be normal for you personally.
The normal range depends on your age, gender, type of blood sample, and how high above sea level the area where you live is. The doctor can use all the indicators of the general blood test when checking the condition of the body. For example, the number of red blood cells, hemoglobin, hematocrit are the main indicators in diagnosing anemia, but erythrocyte indices and smear microscopy also help detect this disease and can show the possibility of its occurrence.
To assess the number and size of leukocytes, the doctor takes into account the results of counting the number of cells and the ratio of their types. To see if there are too many or few cells of a certain type, the doctor compares their number and percentage. There is a norm for each type of leukocyte.
Indicators may change during pregnancy. During each trimester, your doctor should report changes in your normal range.
| Absolute white blood cell count ( WBC ) | |
| Men and non-pregnant women: | 5,000–10,000 WBC per cubic mm (mm3) or 5.0–10.0 x 109 WBC per 1 liter (L) |
| The ratio of different types of leukocytes | |
| Neutrophils: | 50%–62% |
| Band neutrophils: | 3%–6% |
| Lymphocytes: | 25%–40% |
| Monocytes: | 3%–7% |
| Eosinophils: | 0%–3% |
| Basophils: | 0%–1% |
| Absolute red blood cell count ( RBC ) | |
| Men: | 4.5–5.5 million RBC per µl or 4.5–5.5 x 1012/l |
| Women: | 4.0–5.0 million RBC per µL or 4.0–5.0 x 1012/L |
| Children: | 3.8–6.0 million RBC per µL or 3.8–6.0 x 1012/L |
| Newborns: | 4.1–6.1 million RBC per µL or 4.1–6.1 x 1012/L |
| Hematocrit (HCT) | |
| Men: | 42%–52% or 0.42–0.52 of the total volume |
| Women: | 36%–48% or 0.36–0.48 of total volume |
| Children: | 29%–59% or 0.29–0.59 of the total volume |
| Newborns: | 44%–64% or 0.44–0.64 of total volume |
| Hemoglobin (Hgb) | |
| Men: | 14–17.4 grams per deciliter (g/dL) or 140–174 grams per liter (g/L) |
| Women: | 12–16 g/dl or 120–160 g/l |
| Children: | 9.5–20.5 g/dl or 95–205 g/l |
| Newborns: | 14.5–24.5 g/dl or 145–245 g/l |
Typically, a normal hemoglobin level is one third of the hematocrit level.
| Red blood cell indices | |
| Mean erythrocyte volume ( MCV ) - Adults: | 84–96 femtoliters (fl) |
| Mean erythrocyte hemoglobin content ( MCH ) - Adults: | 28–34 picograms (pg) per cell |
| Mean erythrocyte hemoglobin concentration ( MCHC ) - Adults: | 32–36 grams per deciliter (g/dL) |
| Red blood cell distribution width by volume ( RDW ) | |
| Norm: | 11.5%–14.5% |
| Absolute platelet count | |
| Adults: | 140,000–400,000 platelets per mm3 or 140–400 x 109/L |
| Children: | 150,000–450,000 platelets per mm3 or 150–450 x 109/L |
| Mean platelet volume (MPV) | |
| Adults: | 7.4–10.4 µm3 or 7.4–10.4 fl |
| Children: | 7.4–10.4 µm3 or 7.4–10.4 fl |
| Blood smear microscopy | |
| Norm: | Normal indicators of the number, shape, color and size of blood cells. |
High performance
Absolute red blood cell count (RBC)
- Conditions and habits that cause high red blood cell counts include smoking, exposure to carbon monoxide, long-term lung disease, kidney disease, some cancers and heart disease, alcoholism, liver disease, a rare bone marrow disease (polycythemia vera), or rare problems related to with hemoglobin, which are associated with the transfer of oxygen.
- Diseases related to the water component of the body can also cause high red blood cell counts. These include dehydration, diarrhea, vomiting, increased sweating, and taking diuretics. Lack of fluid in the body causes red blood cell counts to appear high. This is sometimes called pseudopolycythemia.
Absolute white blood cell count (WBC)
- Causes of high white blood cell counts include infection, inflammation, tissue damage (for example, due to a heart attack), kidney failure, lupus, tuberculosis, rheumatoid arthritis, malnutrition, leukemia, and cancer.
- Taking costosteroids and certain medications, underactive adrenal glands, problems with the thyroid gland, and removal of the spleen can also cause an increase in white blood cell levels.
Absolute platelet count
- High platelet levels can occur due to bleeding, iron deficiency, cancer and bone marrow problems.
Low performance
Absolute red blood cell count (RBC)
- With anemia, the level of red blood cells decreases. Anemia can be caused by heavy menstrual bleeding, stomach ulcers, colorectal cancer, inflammatory bowel disease, tumors, Addison's disease, thalassemia, lead poisoning, sickle cell disease, or a reaction to certain chemicals and medications. One reason for low red blood cell counts may be removal of the spleen.
- Not getting enough folic acid or vitamin B12 can also cause anemia, such as pernicious anemia, which causes problems absorbing vitamin B12.
- Red blood cell indices and smear microscopy can help find the cause of anemia.
Absolute white blood cell count (WBC)
- Low white blood cell counts may be caused by chemotherapy and reaction to drug treatment, aplastic anemia, viral infections, malaria, alcoholism, AIDS, lupus, Cushing's syndrome.
- An enlarged spleen can reduce white blood cell counts.
Absolute platelet count
- Low platelet levels can be caused by pregnancy, immunopathological thrombocytopenic purpura and other diseases that affect the process of generating platelets or destroy them.
- An enlarged spleen can reduce platelet counts.
What can affect the results of the examination?
Reasons why the analysis is not possible or the results will be incorrect:
- When drawing blood, your arm was tied with an elastic tourniquet for a long time.
- Taking drugs that cause low platelet counts, such as certain antibiotics, steroids, thiazide diuretics, chemotherapy drugs, quinidine, meprobamate.
- Very high levels of white blood cells or fats (triglycerides) can cause falsely high hemoglobin levels.
- With an enlarged spleen, the level of platelets (thrombopenia) or white blood cells may be reduced; this condition can also cause some types of cancer.
- During pregnancy, the level of red blood cells is often reduced, and less often, the level of white blood cells is increased.
On a note:
- The absolute white blood cell count can reach up to 2000 WBC per microliter due to exercise, stress or smoking.
- Children tend to have higher levels of white blood cells than adults.
- Often, a red blood cell count test includes:
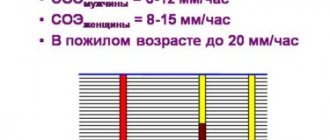
- Erythrocyte sedimentation rate (ESR). The ESR test measures how quickly red blood cells settle to the bottom of a tube. During inflammatory processes occurring in the body (for example, in the presence of infection or cancer), red blood cells settle more slowly than under normal conditions. Using ESR analysis, inflammatory diseases can be diagnosed if the blood test results are normal.
- Analysis of reticulocyte content. This is an analysis of the number of young red blood cells in a blood sample. As a rule, the content of reticulocytes is lower compared to the content of mature red blood cells. However, recent bleeding or destruction of mature red blood cells may cause increased reticulocyte production. This test is done to detect certain types of anemia and screen for the body's response to treatment.
- Hematocrit measurements may vary depending on the assay method and equipment used.
Causes of elevated platelets
An increased number of platelets in the blood (over 400×109/l) is called thrombocytosis. This condition may be a normal reaction of the body to physical activity (reactive thrombocytosis) or one of the signs of the disease. The most common causes of thrombocytosis are:
- Malignant tumors of the bone marrow and other organs.
- Polycythemia vera.
- Iron-deficiency anemia.
- Bleeding and severe blood loss.
- Internal organ injuries.
- Acute and chronic infectious diseases, including tuberculosis.
- Kidney failure.
- Splenectomy.
- Autoimmune pathologies, including rheumatoid arthritis and systemic lupus erythematosus.
- Inflammatory diseases of the gastrointestinal tract.
- Hereditary tendency to thrombocytosis.
In some cases, a consistently high platelet level is normal. In such cases, they speak of primary or essential thrombocytosis. The exact cause of this phenomenon is unknown².
Figure 2. Symptoms of thrombocytosis and thrombocytopenia. Image: mikrostoker/Depositphotos
Basic functions of platelets
In appearance, platelets are round or oval red plates with a smooth surface. They are formed in the bone marrow. They mature in approximately 8 days. These components constantly circulate in the bloodstream.
The main function of platelets is to ensure blood clotting. In addition, the ability of these blood components to stop bleeding is important. This is ensured by the fact that individual platelets can stick together and stick to sites of vascular damage. The process is automatically started by the human body when there is a risk of bleeding.
An important question is how long platelets live. Their viability time lasts approximately 10 days. Depending on the age of the red plates, their size changes: from 2 to 5 microns in diameter.
The process of platelet renewal in the blood occurs constantly. Therefore, an important factor to ensure the maintenance of blood condition is the balance between the formation of red plates and their death. Otherwise, there may be a tendency to blood clots or increased bleeding.
Causes of low platelets
A decrease in blood platelet levels is called thrombocytopenia. As a rule, it is an alarming symptom and requires therapeutic measures. The main causes of thrombocytopenia:
- Severe liver diseases: cirrhosis, hepatitis.
- Thrombocytopenic purpura or Werlhof's disease. A variant of hemorrhagic diathesis, in which the platelet level decreases.
- Hemolytic-uremic syndrome or Gasser's disease. A disease in which, in addition to a decrease in platelet levels, red blood cells disintegrate and acute renal failure occurs.
- Chemotherapy for malignant tumors.
- Taking certain medications: clotrimazole, heparin.
- Malaria.
- Alcohol abuse.
- Bone marrow pathologies, leukemia.
- Thyroid diseases: thyrotoxicosis, hypothyroidism.
- Splenomegaly (enlarged spleen).
- Disseminated intravascular coagulation syndrome.
Also, a decrease in platelet levels below 150-400×109/l is possible during pregnancy. However, this condition is considered a physiological norm.
Platelet donation
The most common donation option is whole blood donation. However, donation of platelets only is also practiced. Blood is taken from one arm and placed into a special machine. In it, platelets are separated from other blood components, which are returned to the donor's vascular bed through the other arm. This cycle is repeated several times. In this way, one donor can contribute the amount of platelets that would normally be obtained from five whole blood tests. In total, this procedure can help save three people³.
Consequences of abnormal platelet levels
Since the main role of platelets in the body is to participate in blood clotting, with a sharp change in their level, changes in this process are observed.
Consequences of thrombocytosis
When the platelet level increases above 600×109/L, the risk of intravascular thrombus formation significantly increases. This, in turn, is a risk factor for myocardial infarction, strokes and circulatory disorders of other internal organs.
Relationship between platelet levels and cardiovascular disease
The risk of developing cardiovascular pathologies is more related to platelet function than to their number. For example, even a normal number of platelets, which tend to aggregate (“clump”), can increase the likelihood of a heart attack or stroke. Therefore, in addition to measuring platelet levels, other blood clotting tests are used.
Consequences of thrombocytopenia
When the level of platelets in the blood decreases below 150×109/l, pathological bleeding occurs. This is manifested by bleeding from the gums and nose. Even with minor impacts, large ecchymoses (bruises) and articular hematomas (bleeding into the joint cavity) occur. Small red dots (petechiae) are also observed on the skin. Women complain of heavy, prolonged menstrual flow. With a strong decrease in platelet levels, internal bleeding may develop.
How to reduce the number of platelets in the blood?
It is first important to identify the cause of thrombocytosis. Reactive thrombocytosis does not need correction. If a sharp increase in platelet levels is associated with any pathology, treatment of the primary disease plays a key role in correction.
Since a high level of platelets in the blood is associated with intravascular thrombus formation, in this condition it is imperative to consult a doctor: your treating specialist or hematologist. Only a doctor can choose the correct correction, taking into account the individual characteristics of the patient.
The following remedies and recommendations can help reduce platelet levels in the blood:
- Medicines, primarily acetylsalicylic acid.
- Drink enough fluids per day.
- Adding more vegetables to your diet: tomatoes, beets, zucchini, garlic and onions.
- Increasing the consumption of fresh fruits and berries: pomegranates, cherries, oranges, grapes.
- Adding or increasing the amount of olive oil and fish oil.
Vegetables help lower platelet levels in the blood.
Photo: timolina / freepik.com A healthy lifestyle also plays an important role: proper nutrition, normalization of work and rest schedules, minimizing stress, moderate physical activity, and stopping the use of tobacco products.
Medicinal herbs
Medicinal herbs, including ginko biloba, can also reduce the level of blood platelets. This plant contains terpenoids that reduce blood viscosity and prevent the formation of blood clots. This remedy can be used both in the form of solutions or capsules, and decoctions from the leaves of the plant.
How to increase the number of platelets in the blood?
Just like thrombocytosis, a deficiency of platelets in the blood should be correlated under the supervision of a physician, taking into account the cause of its occurrence. If there is a risk of bleeding, the basis of therapy is medications, including: etamsylate, aminocaproic acid, thrombopoietin. In critical situations, platelet transfusions may be performed.
With a slight decrease in platelet levels, diet correction is also carried out as an adjuvant. It includes the following products:
- Products made from rye flour and durum wheat.
- Boiled chicken meat and chicken broth.
- Low-fat varieties of fish in the form of boiled meat or cutlets.
- Nuts, including almonds and peanuts.
- Green apples, bell peppers, carrots.
- Fresh vegetable salads based on vegetable oil.
It is important to stop taking medications that may reduce platelet levels or replace them. In this case, the decision to change the medications taken should be made by the attending physician.
PRP therapy
PRP therapy (Patelet Rich Plasma) is a method of treating joints, ligaments, tendons, and bones with a person’s own blood plasma (autoplasma), enriched with platelets.
Due to the presence of growth factor in the blood platelets, they stimulate the natural process of repairing damaged tissue. However, to achieve a noticeable result, the platelet count must be quite large. Therefore, the goal of such therapy is to increase platelet concentration while minimizing the number of red blood cells⁴. Injection into the knee of platelet-rich plasma. Photo: romanzaiets / freepik.com
Causes of increased platelet count
This condition is called thrombocytosis. A large number of platelets occurs with the appearance of diseases such as leukemia, lymphogranulomatosis, oncological diseases of the blood, kidneys and liver, as well as lung diseases (COPD). It can also be accompanied by erythrocytosis, arthritis, enteritis, acute infectious diseases, hemolysis and myeloid leukemia. The number of plates increases under stress, poisoning, and as a result of bleeding. Their number may also increase if the hematopoietic system in the bone marrow is disrupted. Now you know what platelets are in a blood test.
Important! An interesting and important fact is that during bleeding, the number of platelets increases. This is influenced by the body’s compensatory ability. Our body tries to compensate for blood loss as quickly as possible. At the beginning of bleeding, their amount decreases, and after a day it increases noticeably.
causes of thrombocytosis
There is such a condition as secondary thrombocytosis, it develops with obesity, after injuries and surgical interventions, and alcoholism. In this case, the body increases the production of thrombopoietin, which promotes the maturation of bone marrow cells.
In any case, a deviation from the norm requires consulting a doctor and prescribing appropriate treatment. Only after additional research can the doctor identify the cause of the increase in platelet count.