materials » Microscopes » Articles about microscopes, microspecimens and studies of the microworld » Human blood under a microscope
Have you ever wanted to see with your own eyes what human blood looks like under a microscope? After all, this is one of the most interesting tissues of the body! It consists of many cells of different types and performs vital functions: transport (carries oxygen throughout the body), protective (special cells eliminate harmful microorganisms) and homeostatic (maintains the constancy of the internal environment of the body).
In order for you to be able to see how human blood works, the microscope must provide at least 1000x magnification. Take this into account when choosing it.
Blood composition
Blood consists of 4 main components:
- red blood cells - red blood cells that transport oxygen from the lungs to the human organs;
- white blood cells - leukocytes responsible for fighting infections that attack the body;
- blood platelets - platelets that ensure blood clotting, thereby protecting the body from fatal blood loss due to injuries and cuts.
All these cells are suspended in blood plasma, which not only serves as a transport medium for blood cells, moving them throughout the human body, but also contains proteins and salts necessary for the body.
What is a microscope
This is an optical device that produces images magnified several times.
Both visible and invisible objects are subject to research. Most often these are microorganisms, cells of living tissues, elements of the structure of substances and much more. Microscopes can be simple or complex. The first device consists of one plano-convex lens (for example, a regular magnifying glass), the complex one combines a combination of two simple lenses. Interesting!
Modern microscopes can provide magnification up to 2000x, at which the image quality will be excellent.
A compound microscope is used to examine blood, as it provides high magnification and has high resolution. The action is based on a two-step scheme:
- One objective (lens) is brought close to the object. It enlarges the image with the required resolution.
- The second lens (eyepiece) is placed directly close to the observer’s organ of vision.
Two lens systems are located at opposite ends of the device tube. The tripod is the main part of the tube.
Red blood cells - erythrocytes
Red blood cells perform one of the important functions of blood. A drop of blood contains millions of red blood cells, which constantly circulate through the blood vessels, delivering oxygen to the organs and removing carbon dioxide formed during cellular respiration.
Red blood cells are called red blood cells because they contain the protein hemoglobin, which is bright red in color. It is hemoglobin that carries oxygen and carbon dioxide. As blood passes through the lungs, oxygen molecules attach to hemoglobin, which delivers it to every cell in our body. Freed from oxygen, hemoglobin attaches carbon dioxide molecules to itself. In the lungs, carbon dioxide is released and removed from the body through breathing.
The average lifespan of a red blood cell is 120 days. The bone marrow constantly produces blood cells, replenishing their natural loss.
Clinical blood analysis: from light microscope to hematological analyzers
A general clinical blood test is the most common diagnostic test that a doctor prescribes to a patient.
Over the past decades, the technology of this routine, but very informative research has made a colossal leap - it has become automatic. High-tech automatic hematology analyzers came to the aid of the laboratory diagnostics doctor, whose tool of work was an ordinary light microscope. In this post we will tell you what exactly happens inside the “smart machine” that sees right through our blood, and why you should trust it. We will consider the physics of processes using the example of the UniCel DxH800 hematology analyzer
global brand Beckman Coulter. It is on this equipment that studies ordered from the laboratory diagnostics service LAB4U.RU are performed. But to understand automated blood testing technology, we'll look at what the lab technicians saw under the microscope and how they interpreted that information.
Blood test parameters
So, there are three types of cells in the blood:
- leukocytes that provide immune protection;
- platelets, responsible for blood clotting;
- red blood cells that transport oxygen and carbon dioxide.
These cells are found in the blood in very specific quantities. They are determined by the person’s age and state of health. Depending on the conditions in which the body is located, the bone marrow produces as many cells as the body requires. Therefore, knowing the number of a certain type of blood cells and their shape, size and other qualitative characteristics, you can confidently judge the condition and current needs of the body. It is these key parameters - the number of cells of each type, their appearance and qualitative characteristics
- that make up a general clinical blood test.
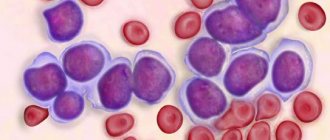
When conducting a general blood test, the number of red blood cells, platelets and leukocytes is counted. It’s more complicated with leukocytes: there are several types of them, and each type performs its own function. There are 5 different types of leukocytes:
- neutrophils, which mainly neutralize bacteria;
- eosinophils, neutralizing antigen-antibody immune complexes;
- basophils involved in allergic reactions;
- monocytes are the main macrophages and utilizers;
- lymphocytes providing general and local immunity.
In turn, neutrophils according to the degree of maturity are divided into:
- stab,
- segmented,
- myelocytes,
- metamyelocytes.
The percentage of each type of leukocyte in their total volume is called the leukocyte formula, which has important diagnostic value.
For example, the more pronounced the bacterial inflammatory process, the more neutrophils in the leukocyte formula. The presence of neutrophils of varying degrees of maturity indicates the severity of the bacterial infection. The more acute the process, the more band neutrophils in the blood. The appearance of metamyelocytes and myelocytes in the blood indicates an extremely severe bacterial infection. Viral diseases are characterized by an increase in lymphocytes, and in allergic reactions - an increase in eosinophils. In addition to quantitative indicators, cell morphology is extremely important. A change in their usual shape and size also indicates the presence of certain pathological processes in the body.
An important and most well-known indicator is the amount of hemoglobin in the blood - a complex protein that ensures the supply of oxygen to tissues and the removal of carbon dioxide. The concentration of hemoglobin in the blood is the main indicator in the diagnosis of anemia.
Another important parameter is the erythrocyte sedimentation rate (ESR). During inflammatory processes, red blood cells tend to stick together, forming small clots. Having greater mass, clumped red blood cells settle faster under the influence of gravity than single cells. The change in their sedimentation rate in mm/h is a simple indicator of inflammatory processes in the body.
How it was: scarifier, test tubes and microscope
Blood collection
Let's remember how they used to donate blood: a painful puncture of the pad with a scarifier, endless glass tubes into which precious drops of squeezed blood were collected.
How a laboratory assistant traced one piece of glass over another, where there was a drop of blood, scratching a number on the glass with a simple pencil. And endless test tubes with different liquids. Now it already seems like some kind of alchemy. Blood was taken specifically from the ring finger, for which there were quite serious reasons: the anatomy of this finger is such that its injury poses a minimal threat of sepsis in case of infection of the wound. Taking blood from a vein was considered much more dangerous. Therefore, venous blood analysis was not routine, but was prescribed as necessary, and mainly in hospitals.
It is worth noting that already at the sampling stage significant errors began. For example, different thicknesses of the skin give different depths of the injection; tissue fluid entered the test tube along with the blood - hence the change in blood concentration; in addition, with pressure on the finger, blood cells could be destroyed.
Remember the row of test tubes where the blood collected from your finger was placed? To count different cells, you actually needed different tubes. For erythrocytes - with saline solution, for leukocytes - with a solution of acetic acid, where the erythrocytes were dissolved, for the determination of hemoglobin - with a solution of hydrochloric acid. There was a separate capillary for determining ESR. And at the last stage, a smear was made on the glass for subsequent calculation of the leukocyte formula.
Blood test under a microscope
To count cells under a microscope in laboratory practice, a special optical device was used, proposed back in the 19th century by a Russian doctor, after whom this device was named - the Goryaev camera.
It made it possible to determine the number of cells in a given microvolume of liquid and was a thick glass slide with a rectangular recess (chamber). A microscopic mesh was applied to it. The top of Goryaev’s chamber was covered with a thin cover glass. This grid consisted of 225 large squares, 25 of which were divided into 16 small squares. Red blood cells were counted in small striated squares located diagonally in Goryaev’s chamber. Moreover, there was a certain rule for counting the cells that lie on the border of the square. The number of red blood cells per liter of blood was calculated using a formula based on the dilution of the blood and the number of squares in the grid. After mathematical abbreviations, it was enough to multiply the calculated number of cells in the chamber by 10 to the 12th power and enter it into the analysis form.
Leukocytes were counted here, but larger grid squares were used, since leukocytes are a thousand times larger than red blood cells. After counting leukocytes, their number was multiplied by 10 to the 9th power and entered into the form. An experienced laboratory technician took an average of 3-5 minutes to count cells.
Methods for counting platelets in the Goryaev chamber were very labor-intensive due to the small size of this type of cell. Their number had to be estimated only on the basis of a stained blood smear, and the process itself was also very labor-intensive. Therefore, as a rule, platelet counts were calculated only upon specific request from the physician.
Leukocyte formula
, that is, the percentage composition of each type of leukocytes in their total number could only be determined by a doctor - based on the results of studying blood smears on glasses.
Visually identifying the different types of leukocytes in the field of view by the shape of their nucleus, the doctor counted the cells of each type and their total number.
Having counted 100 in total, he received the required percentage of each type of cell. To simplify counting, special counters with separate keys for each type of cell were used. It is noteworthy that such an important parameter as hemoglobin was determined by the laboratory assistant visually (!) by the color of hemolyzed blood in a test tube with hydrochloric acid. The method was based on the conversion of hemoglobin into brown hydrochloric acid hematin, the color intensity of which is proportional to the hemoglobin content. The resulting solution of hematin hydrochloride was diluted with water to the color of the standard corresponding to the known concentration of hemoglobin. In general, the last century
How it became: vacuum containers and hematology analyzers
Let's start with the fact that the technology of blood sampling has now completely changed. Scarifiers and glass capillaries with test tubes were replaced by vacuum containers. The blood sampling systems now in use are low-traumatic, the process is completely unified, which has significantly reduced the percentage of errors at this stage. Vacuum tubes containing preservatives and anticoagulants allow blood to be stored and transported from the point of collection to the laboratory. It is thanks to the advent of new technology that it has become possible to take tests as conveniently as possible - at any time, anywhere.
At first glance, it seems impossible to automate such a complex process as identifying and counting blood cells. But, as usual, everything ingenious is simple. Automatic blood testing is based on fundamental physical laws. The technology for automatic cell counting was patented back in 1953 by Americans Joseph and Wallace Coulter. It is their name that is in the name of the global brand of hematological equipment Beckman&Coulter.
Cell counting
The aperture-impedance method (Coulter method or conductometric method) is based on counting the number and assessing the nature of impulses that occur when a cell passes through a small-diameter hole (aperture), on both sides of which two electrodes are located. As a cell passes through a channel filled with electrolyte, the resistance to electric current increases. Each passage of the cell is accompanied by the appearance of an electrical impulse. To find out what the cell concentration is, it is necessary to pass a certain volume of sample through the channel and count the number of pulses that appear. The only limitation is that the sample concentration must ensure that only one cell passes through the aperture at a time.
Automated hematology analysis technology has come a long way over the past 60 years. At first, these were simple cell counters that determined 8-10 parameters: red blood cell count (RBC), white blood cell count (WBC), hemoglobin (Hb) and several calculated ones. These were first class
.
Second class
analyzers have already determined up to 20 different blood parameters. They are significantly higher in the level of differentiation of leukocytes and are able to isolate populations of granulocytes (eosinophils + neutrophils + basophils), lymphocytes and an integral population of medium cells, which included monocytes, eosinophils, basophils and plasma cells. This differentiation of leukocytes has been successfully used in the examination of practically healthy people.
The most technologically advanced and innovative analyzers today are third-class
, which determine up to hundreds of different parameters, carry out detailed differentiation of cells, including by degree of maturity, analyze their morphology and signal the laboratory assistant about the detection of pathology.
Third-class machines, as a rule, are also equipped with automatic systems for preparing smears (including their coloring) and displaying images on the monitor screen. These advanced hematology systems include BeckmanCoulter equipment, such as the UniCel DxH 800 Cell Analysis System
.
Modern BeckmanCoulter devices use multiparameter flow cytometry based on patented VCS (Volume-Conductivity-Scatter) technology.
VCS technology involves assessing cell volume, its electrical conductivity and light scattering. The first parameter, cell volume, is measured using the Coulter principle based on an estimate of the resistance as a cell passes through an aperture at a constant current. The size and density of the cell nucleus, as well as its internal composition, are determined by measuring its electrical conductivity in high-frequency alternating current. Scattering of laser light at different angles allows one to obtain information about the structure of the cell surface, the granularity of the cytoplasm and the morphology of the cell nucleus.
The data obtained from three channels is combined and analyzed. As a result, the cells are distributed into clusters, including separation according to the degree of maturity of erythrocytes and leukocytes (neutrophils). Based on the obtained measurements of these three dimensions, many hematological parameters are determined - up to 30 for diagnostic purposes, more than 20 for research purposes and more than a hundred specific calculated parameters for highly specialized cytological studies. Data is visualized in 2D and 3D formats. A laboratory technician working with a BackmanCoulter hematology analyzer sees the analysis results on the monitor looking something like this:
And then he decides whether they need to be verified or not.
Needless to say, the information content and accuracy of modern automatic analysis is many times higher than manual analysis? The productivity of machines of this class is about a hundred samples per hour when analyzing thousands of cells in a sample. Let us remember that during microscopy of a smear, the doctor analyzed only 100 cells!
However, despite these impressive results, microscopy still remains the “gold standard” for diagnosis. In particular, when the apparatus detects pathological cell morphology, the sample is analyzed manually under a microscope. When examining patients with hematological diseases, microscopy of a stained blood smear is performed only manually by an experienced hematologist. This is exactly how, manually, in addition to automatic cell counting, the leukocyte formula is assessed in all children's blood tests according to orders made using the online laboratory service LAB4U.RU.
Instead of a resume
Technologies for automated hematological analysis continue to develop rapidly.
Essentially, they have already replaced microscopy in routine preventive tests, leaving it for particularly significant situations. We mean children's tests, tests of people with confirmed diseases, especially hematological ones. However, in the foreseeable future, in this area of laboratory diagnostics, doctors will receive devices capable of independently performing morphological analysis of cells using neural networks. By reducing the burden on doctors, they will at the same time increase the requirements for their qualifications, since only atypical and pathological cell conditions will remain in the human decision-making zone. The number of informative parameters of blood analysis, which has increased many times over, raises the requirements for professional qualifications and for the clinician, who needs to analyze combinations of values of a mass of parameters for diagnostic purposes. Expert systems come to the aid of doctors on this front, which, using analyzer data, provide recommendations for further examination of the patient and give a possible diagnosis. Such systems are already available on the laboratory market. But this is a topic for a separate article.
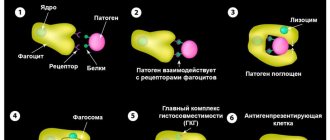
White blood cells - leukocytes
Leukocytes perform protective functions; as soon as an infection enters the body, white blood cells - leukocytes - come into play. Leukocytes are constantly on guard. Some white blood cells (lymphocytes) produce protective antibodies - proteins that neutralize or destroy viruses and pathogenic bacteria.
The life cycle of leukocytes is relatively short - from several days to several weeks. One cube of blood from a healthy person contains from 4 to 8 thousand leukocytes. If the body is fighting an infection, this number may increase. A persistently too high or too low number of white blood cells in the blood may indicate the presence of serious illnesses.
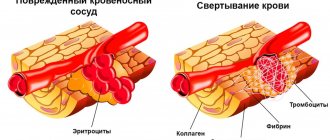
Platelets are cells that protect the body from fatal blood loss.
Platelets are formed blood elements that participate in hemostasis. They are represented by small biconvex cells that do not have a nucleus. The diameter of the platelet varies between 2-10 microns.
Platelets are produced by red bone marrow, where they undergo 6 cycles of maturation, after which they enter the bloodstream and remain there for 5 to 12 days. Platelet destruction occurs in the liver, spleen and bone marrow.
Platelets
While in the bloodstream, platelets have the shape of a disk, but when activated, the platelet takes on the shape of a sphere, on which pseudopodia are formed - special outgrowths with the help of which platelets connect to each other and adhere to the damaged surface of the vessel.
In the human body, platelets perform 3 main functions:
- Create plugs on the surface of a damaged blood vessel, helping to stop bleeding (primary thrombus),
- Participate in blood clotting, which is also important for stopping bleeding,
- Platelets provide nutrition to vascular cells.
Platelets are classified into:
- Microforms – platelet with a diameter of up to 1.5 microns,
- Normal forms of platelets with a diameter of 2 to 4 µm,
- Macroforms of a platelet with a diameter of 5 microns,
- Megaloform platelets with a diameter of up to 6-10 microns.
Platelets
It is very difficult for a person to tolerate massive blood loss. However, our body has a mechanism that protects it from blood loss, and platelets play a major role in this mechanism.
Platelets are colorless, irregularly shaped bodies that circulate in the blood. They have the ability to form clots (thrombi) that stop bleeding.
If bleeding begins, platelets gather at the wound and try to block the bleeding. Calcium, vitamin K and the protein fibrinogen help platelets form a clot to close a bleeding vessel. As the curd dries, it hardens, forming the well-known “crust”.
Blood groups and Rh factor
On the surface of red blood cells there are antigens, of which there are many varieties. This is why one person's blood can be different from another's. Antigens form the Rh factor and blood group.
antigen; blood type
| 0 | I |
| 0A | II |
| 0B | III |
| AB | IV |
The presence/absence of Rh antigen on the surface of an erythrocyte is determined by the Rh factor (if Rh is present, Rh is positive, if Rh is not present, Rh is negative).
Determining the Rh factor and blood group of a person is of great importance when transfusing donor blood. Some antigens are incompatible with each other, causing destruction of blood cells, which can lead to the death of the patient. It is very important to receive a blood transfusion from a donor whose blood type and Rh factor match those of the recipient.
Norm of red blood cells, leukocytes and platelets in the blood (table)
age; polyerythrocytes (x 10 12 / l); leukocytes (x 10 9 /l); platelets (x 10 9 /l)
| 1-3 months | husband | 3,5 — 5,1 | 6,0 — 17,5 | 180 — 490 |
| wives | ||||
| 3-6 months | husband | 3,9 — 5,5 | ||
| wives | ||||
| 6-12 months | husband | 4,0 — 5,3 | 180 — 400 | |
| wives | ||||
| 1-3 years | husband | 3,7 — 5,0 | 6,0 — 17,0 | 160 — 390 |
| wives | ||||
| 3-6 years | husband | 5,5 — 17,5 | ||
| wives | ||||
| 6-12 years | husband | 4,5 — 14,0 | 160 — 380 | |
| wives | ||||
| 12-15 years | husband | 4,1 — 5,5 | 4,5 — 13,5 | 160 — 360 |
| wives | 3,5 — 5,0 | |||
| 16 years | husband | 4,0 — 5,5 | 4,5 — 12,0 | 180 — 380 |
| wives | 3,5 — 5,0 | 150 — 380 | ||
| 16-65 years old | husband | 4,0 — 5,6 | 4,5 — 11,0 | 180 — 400 |
| wives | 3,9 — 5,0 | 150 — 340 | ||
| over 65 years old | husband | 3,5 — 5,7 | 180 — 320 | |
| wives | 3,5 — 5,2 | 150 — 320 |