Blood provides metabolism, nutrition and even respiration for all cells and tissues in the body. Doctors always closely monitor its indicators, using tests to determine the presence of certain diseases that destroy the body from the inside without visible symptoms. That is why blood tests are regularly taken: both for preventive purposes and to make a more accurate diagnosis.
One of the most important components of blood are red blood cells or, as they are also called, red cells. They have a disc-shaped, doubly concave shape and perform one of the most important functions in the body - transporting oxygen to cells and carbon dioxide for its removal. Their size is not as important as their volume. In a healthy person, the volume of all red blood cells should be approximately the same, or with slight deviations from the norm; in the case of pathology, different cells appear. To identify such abnormalities, a blood test for RDW is performed.
The abbreviation RDW stands for Red Cells Indicies and translated means “red blood cell distribution width.” This indicator can be found in the results of a general blood test, since a separate study of red blood cells is not carried out. It has two markers:
- RDW-CV: shows how much cell size differs from the average (measured as a percentage)
- RDW-SD: Reflects the difference in size between the smallest and largest red blood cells (measured in femtoliters).
Indications for testing
Often, such an analysis is preventive and is taken on a regular basis (on average once a year) to identify diseases in the early stages, when they are much faster and easier to treat. It is prescribed to pregnant women to monitor their general condition and identify problems such as anemia, and for inpatient monitoring.
A general blood test is required during hospitalization to conduct a basic examination and obtain a more accurate picture of the disease, as well as before surgery to prevent possible complications. If the body is severely weakened, this may indicate that the person will not survive the operation; in such cases, it is necessary to undergo preliminary treatment for recovery.
The analysis is prescribed to identify and diagnose different types of anemia, as well as for possible diseases of the hematopoietic system. A general blood test helps track dynamics during monitoring of ongoing treatment, accurately determining the onset of improvements or deteriorations in the body’s condition, which helps to timely adjust treatment. It can be prescribed by a physician, general practitioner, surgeon, neurologist and hematologist.
Blood levels
As mentioned above, the RDW indicator has two markers: RDW-CV and RDW-SD, each of which has its own units of measurement and content standards. Next we will look at each of them.
RDW-CV reflects the deviation of red blood cell size from the average, measured as a percentage and has different standards depending on the person’s age.
- Children under 6 months: from 14.9 to 18.7%
- Children over 6 months: from 11.6 to 14.8%
- Adults: 11.5 – 14.5%
RDW-SD shows deviations in the distribution of red blood cells by volume and is measured in femtoliters. The standard deviation is 37 – 54 femtoliters, regardless of age or gender.
Complete blood count with leukocyte count and ESR
Complete blood count is the most widely used laboratory method in clinical practice. It allows you to identify numerous pathological disorders in the body, often plays a key role in making a diagnosis, and may be an indication for prescribing other studies.
Prescribed in case of:
- Preventive examination;
- Planning hospitalization, invasive interventions, surgical operations;
- The presence of anemic symptoms (pallor of the skin, weakness, dizziness, tinnitus, tachycardia);
- Diseases of the hematopoietic organs;
- Infectious and inflammatory diseases;
- Monitoring the effectiveness of treatment.
It includes a large number of different parameters, each of which has its own value both individually and in a comprehensive study.
| № | Russian name | Reduction | Norm | Decrease in normal level | Increase in normal level | |
| Men | Women | |||||
| 1 | Red blood cells | RBC,Er, | 4.0-5.6*1012l | 3.4-5.0*1012l | Hemolytic, hemorrhagic, sideroblastic, iron deficiency anemia (IDA); Deficiency of vit B12, folic acid; Enteropathology; After intensive infusion, hypervolemia; Renal pathology associated with insufficient formation of erythropoietins - stimulators of red blood cell growth | Dehydration; Tumor hematopoiesis; Kidney neoplasms leading to hypersecretion of erythropoietin; Erythrocythemia, polycythemia; Chronic hypoxia, cardiopulmonary failure |
| 2 | Hemoglobin | HGB, Hb | 130-160g/l | 120-140g/l | ||
| 3 | Average HGB content in RBC | MCH | 27-31pg | |||
| 4 | Average Hb concentration in RBC | MCHC | 30-38g/dl | |||
| 5 | Color index | CPU | 0,84-1,0 | |||
| 6 | Hematocrit | HCT | 40-60% | 35-45% | ||
| 7 | Distribution width | RDW-CV | 11,4-14,8% | When going beyond any limits of reference values: Microcytosis or macrocytosis in a deficient anemic status; Metastases; Thalassemia; After blood transfusion | ||
| 8 | Heterogeneity index | RDW-SD | 35-60fl | |||
| 9 | Red blood cell volume | MCV | 80-100fl | IDA, intravascular hemolysis | Lack of vitamin B-12, folate, hepatopathology | |
| 10 | Absolute number of Er containing a nucleus | NRBC# | Normally absent | Used to diagnose thalassemia, sickle cell anemia; Oncohematology; Critical moments in resuscitation practice; Severe hypoxia; Widely used in neonatology and pediatrics. | ||
| 11 | Relative number of Er containing a nucleus | NRBC% | ||||
| 12 | Reticulocytes | RTC | 0,2-1,2% | Inhibition of hematopoiesis due to deficiency conditions or damage to the CMC | Posthemorrhagic, hypoxic status, the result of active treatment of anemia | |
| 13 | Platelets | PLT, Tr | 180-320*109l | Malignant destruction of red bone marrow, platelet germ, deficiency of vitamin B12, Fe and folic acid, viruses, hyperthyroidism | Myelofibrosis, autoimmune processes, tuberculosis, depression of megakaryocyte stem cells, collagenosis, liver cirrhosis, side effect of cytostatics | |
| 14 | Thrombocrit | PCT | 0,14-0,37% | |||
| 15 | Platelet volume | MPV | 7.5-12fl | Pregnancy; Multiple myeloma; Infections and inflammation; Oncohematology | After bleeding; Hereditary syndromes | |
| 16 | Large PLT Ratio (P-LCR) | P-LCR | 13-43% | |||
| 17 | Distribution width Tr | PDW | 15-17% | Exceeding the limits in any of the above situations, leading to quantitative and qualitative platelet changes | ||
| 18 | Leukocytes | WBC | 4-9.0*109l | Metastatic destruction of BMC, after chemotherapy, toxic effects, pneumonia, sepsis, immunodeficiency | The vast majority of infectious and inflammatory syndromes, trauma, surgical interventions, systemic immune hyperreactions | |
The leukocyte formula is used in the differential diagnosis of inflammatory aseptic, bacterial, viral, parasitic, and fungal diseases. Usually includes relative values of different types of leukocytes, however, if necessary (determined by the doctor), absolute numbers can be calculated:
- Basophils (BASO): above 1% occurs with allergies, hypothyroidism, chronic myeloid leukemia;
- Eosinophils (EO): 1-5%. Increased in allergic, parasitic, autoimmune conditions. Decrease in sepsis, abscesses, poisoning;
- Neutrophils (NEUT): band-nuclear up to 0-5%, growth in severe inflammatory-infectious pathology. Segmented up to 72%, less than 30% in case of anemia, damage to hematopoiesis due to intoxication, viral invasion, metastases, after chemotherapy;
- Lymphocytes (LYMPH) 19-37% . Lower in lymphogranulomatosis, AIDS, after cytostatic and glucocorticoid therapy. Higher in leukemia, toxicosis, drug overdose;
- Monocytes (MONO) 3-11%. Growth in bacterial invasion, rheumatoid arthritis. Fall due to immunodeficiency.
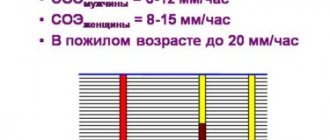
ESR (ESR): for men – up to 10 mm/hour, for women – up to 15 mm/hour. One of the markers of acute inflammatory process. It increases with increasing concentrations of immunoglobulins, C-reactive protein, fibrinogen, which is observed during inflammation, intoxication, and progression of malignant tumors.
To correctly interpret the results obtained, it is not enough to know the reference numbers; you need clinical thinking and the ability to comprehensively assess the current medical situation, which only an experienced specialist can help with.
Deviations from the norm (what they talk about)
Before talking about the possible reasons for deviations in this indicator, it is worth noting that it is not specific and cannot serve to accurately determine a particular disease. RDW is analyzed only in conjunction with other data from a general and biochemical blood test. So, if there is a slight deviation from the norm, but other indicators do not cause concern, then, most likely, this simply indicates the characteristics of the body, but to make a more accurate diagnosis, you need to consult a doctor.
An increase in RDW is normal only for newborns under 6 months of age. There is also a slight increase as a result of recent nervous stress and after a blood transfusion, but in all other cases, elevated results indicate the presence of the disease. They may indicate various types of anemia:
- Anemia of megaloblastic, myelodysplastic and siderablastic types
- Anemia with heterogeneity in red blood cell size (most often due to diet)
- Anemia due to impaired myelopoiesis
- Anemia due to chronic diseases
- Anemia due to acute blood loss (may indicate internal bleeding)
- Aplastic anemia
Also, elevated RDW levels may indicate the following diseases:
- Some homozygous hemoglobinopathies and homozygous thalassemias
- Increased reticulocyte count
- Hyperglycemia
- Congenital genetic diseases
Reduced indicators do not indicate the presence of any abnormality or disease, therefore such values are not taken into account during the examination. Most likely, this is a variant of the norm.
MEDICAL CENTER
Interpretation of study results contains information for the attending physician and is not a diagnosis.
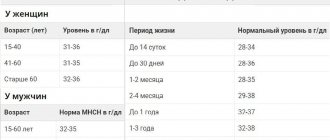
The information in this section should not be used for self-diagnosis or self-treatment. The doctor makes an accurate diagnosis using both the results of this examination and the necessary information from other sources: medical history, results of other examinations, etc. Hemoglobin (Hb, hemoglobin) Units of measurement in the medical center STUDIO DOCTOR: g/dl. Alternative units: g/l. Conversion factor: g/l x 0.1 ==> g/dl. Reference values
| Age, gender | Hemoglobin level, g/dl | |
| Children | ||
| 1 day - 14 days | 13,4 — 19,8 | |
| 14 days - 4.3 weeks | 10,7 — 17,1 | |
| 4.3 weeks - 8.6 weeks | 9,4 — 13,0 | |
| 8.6 weeks - 4 months | 10,3 — 14,1 | |
| 4 months – 6 months | 11,1 — 14,1 | |
| 6 months – 9 months | 11,4 — 14,0 | |
| 9 months - 12 months | 11,3 — 14,1 | |
| 12 months - 5 years | 11,0 — 14,0 | |
| 5 years - 10 years | 11,5 — 14,5 | |
| 10 years - 12 years | 12,0 — 15,0 | |
| 12 years - 15 years | Women | 11,5 — 15,0 |
| Men | 12,0 — 16,0 | |
| 15 years - 18 years | Women | 11,7 — 15,3 |
| Men | 11,7 — 16,6 | |
| 18 years - 45 years | Women | 11,7 — 15,5 |
| Men | 13,2 — 17,3 | |
| 45 years - 65 years | Women | 11,7 — 16,0 |
| Men | 13,1 — 17,2 | |
| > 65 years old | Women | 11,7 — 16,1 |
| Men | 12,6 — 17,4 | |
Increased hemoglobin levels:
- dehydration (with severe diarrhea, vomiting, increased sweating, diabetes, burn disease, peritonitis);
- physiological erythrocytosis (in residents of high mountains, pilots, athletes);
- symptomatic erythrocytosis (with insufficiency of the respiratory and cardiovascular systems, polycystic kidney disease);
- erythremia.
Decreased hemoglobin:
- anemia of various etiologies;
- overhydration.
Hematocrit (Ht, hematocrit)
Units of measurement in the medical center STUDIO DOCTOR: %.
Reference values
| Age, gender | Hematocrit indicator, % | |
| Children | ||
| 1 day - 14 days | 41,0 — 65,0 | |
| 14 days - 4.3 weeks | 33,0 — 55,0 | |
| 4.3 weeks - 8.6 weeks | 28,0 — 42,0 | |
| 8.6 weeks - 4 months | 32,0 — 44,0 | |
| 4 months – 9 months | 32,0 — 40,0 | |
| 9 months - 12 months | 33,0 — 41,0 | |
| 12 months - 3 years | 32,0 — 40,0 | |
| 3 years - 6 years | 32,0 — 42,0 | |
| 6 years - 9 years | 33,0 — 41,0 | |
| 9 years - 12 years | 34,0 — 43,0 | |
| 12 years - 15 years | Women | 34,0 — 44,0 |
| Men | 35,0 — 45,0 | |
| 15 years - 18 years | Women | 34,0 — 44,0 |
| Men | 37,0 — 48,0 | |
| 18 years - 45 years | Women | 35,0 — 45,0 |
| Men | 39,0 — 49,0 | |
| 45 years - 65 years | Women | 35,0 — 47,0 |
| Men | 39,0 — 50,0 | |
| 65 years - 120 years | Women | 35,0 — 47,0 |
| Men | 37,0 — 51,0 | |
Increased hematocrit:
- dehydration (with severe diarrhea, vomiting, increased sweating, diabetes, burn disease, peritonitis);
- physiological erythrocytosis (in residents of high mountains, pilots, athletes);
- symptomatic erythrocytosis (with insufficiency of the respiratory and cardiovascular systems, polycystic kidney disease);
- erythremia.
Decreased hematocrit:
- anemia of various etiologies;
- overhydration.
Red blood cells
Units of measurement at the STUDIO DOCTOR medical center: million/µl (106/µl). Alternative units: 1012 cells/L.
Conversion factors: 1012 cells/l = 106 cells/μl = million/μl.
Reference values
| Age, gender | Red blood cells, million/µl (x106/µl) | |
| Children | ||
| 1 day - 14 days | 3,90 — 5,90 | |
| 14 days - 4.3 weeks | 3,30 — 5,30 | |
| 4.3 weeks - 4 months | 3,50 — 5,10 | |
| 4 months – 6 months | 3,90 — 5,50 | |
| 6 months – 9 months | 4,00 — 5,30 | |
| 9 months - 12 months | 4,10 — 5,30 | |
| 12 months - 3 years | 3,80 — 4,80 | |
| 3 years - 6 years | 3,70 — 4,90 | |
| 6 years - 9 years | 3,80 — 4,90 | |
| 9 years - 12 years | 3,90 — 5,10 | |
| 12 years - 15 years | Women | 3,80 — 5,00 |
| Men | 4,10 — 5,20 | |
| 15 years - 18 years | Women | 3,90 — 5,10 |
| Men | 4,20 — 5,60 | |
| 18 years - 45 years | Women | 3,80 — 5,10 |
| Men | 4,30 — 5,70 | |
| 45 years - 65 years | Women | 3,80 — 5,30 |
| Men | 4,20 — 5,60 | |
| 65 years - 120 years | Women | 3,80 — 5,20 |
| Men | 3,80 — 5,80 | |
Increased red blood cell concentration:
- dehydration (with severe diarrhea, vomiting, increased sweating, diabetes, burn disease, peritonitis);
- physiological erythrocytosis (in residents of high mountains, pilots, athletes);
- symptomatic erythrocytosis (with insufficiency of the respiratory and cardiovascular systems, polycystic kidney disease);
- erythremia.
Decreased red blood cell concentration:
- anemia of various etiologies;
- overhydration.
MCV (mean erythrocyte volume) Determination method: calculated value. Units of measurement at the STUDIO DOCTOR medical center: fl (femtoliter). Reference values
| Age, gender | Mean erythrocyte volume, MCV, fl | |
| Children | ||
| 1 day - 14 days | 88,0 — 140,0 | |
| 14 days - 4.3 weeks | 91,0 — 112,0 | |
| 4.3 weeks - 8.6 weeks | 84,0 — 106,0 | |
| 8.6 weeks - 4 months | 76,0 — 97,0 | |
| 4 months – 6 months | 68,0 — 85,0 | |
| 6 months – 9 months | 70,0 — 85,0 | |
| 9 months - 12 months | 71,0 — 84,0 | |
| 12 months - 5 years | 73,0 — 85,0 | |
| 5 years - 10 years | 75,0 — 87,0 | |
| 10 years - 12 years | 76,0 — 90,0 | |
| 12 years - 15 years | Women | 73,0 — 95,0 |
| Men | 77,0 — 94,0 | |
| 15 years - 18 years | Women | 78,0 — 98,0 |
| Men | 79,0 — 95,0 | |
| 18 years - 45 years | Women | 81,0 — 100,0 |
| Men | 80,0 — 99,0 | |
| 45 years - 65 years | Women | 81,0 — 101,0 |
| Men | 81,0 — 101,0 | |
| 65 years - 120 years | Women | 81,0 — 102,0 |
| Men | 83,0 — 103,0 | |
Increasing MCV values:
- B12 deficiency and folate deficiency anemia;
- aplastic anemia;
- liver diseases;
- hypothyroidism;
- autoimmune anemia;
- smoking and drinking alcohol.
Reducing MCV values:
- Iron-deficiency anemia;
- anemia of chronic diseases;
- thalassemia;
- some types of hemoglobinopathies.
It should be taken into account that the MCV value is not specific; the indicator should be used to diagnose anemia only in combination with other indicators of a general blood test and biochemical blood test.
RDW (Red cell Distribution Width, distribution of red blood cells by size)
Method of determination: calculated value Units of measurement in the medical center STUDIO DOCTOR: %
Reference values
< 6 months — 14.9 – 18.7
> 6 months — 11.6 – 14.8
Increasing RDW values:
- anemia with heterogeneity of red blood cell size, including those associated with nutrition; myelodysplastic, megaloblastic and sideroblastic types; anemia accompanying myelophthisis; homozygous thalassemia and some homozygous hemoglobinopathies;
- a significant increase in the number of reticulocytes (for example, due to successful treatment of anemia);
- condition after red blood cell transfusion;
- interferences – cold agglutinins, chronic lymphocytic leukemia (high number of leukocytes), hyperglycemia.
There are also a number of anemias that are not characterized by an increase in RDW:
- anemia of chronic diseases;
- anemia due to acute blood loss;
- aplastic anemia
- some genetically determined diseases (thalassemia, congenital spherocytosis, presence of hemoglobin E).
It should be taken into account that the value of the RDW indicator is not specific; the indicator should be used to diagnose anemia only in combination with other indicators of a general blood test and biochemical blood test.
MCH (average amount of hemoglobin in 1 red blood cell)
Determination method: calculated value.
Units of measurement and conversion factors: pg (picograms).
Reference values
| Age, gender | Average hemoglobin content in 1 red blood cell, MCH, pg | |
| Children | ||
| 1 day - 14 days | 30,0 — 37,0 | |
| 14 days - 4.3 weeks | 29,0 — 36,0 | |
| 4.3 weeks - 8.6 weeks | 27,0 — 34,0 | |
| 8.6 weeks - 4 months | 25,0 — 32,0 | |
| 4 months – 6 months | 24,0 — 30,0 | |
| 6 months – 9 months | 25,0 — 30,0 | |
| 9 months - 12 months | 24,0 — 30,0 | |
| 12 months - 3 years | 22,0 — 30,0 | |
| 3 years - 6 years | 25,0 — 31,0 | |
| 6 years - 9 years | 25,0 — 31,0 | |
| 9 years - 15 years | 26,0- 32,0 | |
| 15 - 18 years old | Women | 26,0 — 34,0 |
| Men | 27,0 — 32,0 | |
| 18 – 45 years old | Women | 27,0 — 34,0 |
| Men | 27,0 — 34,0 | |
| 45 – 65 years | Women | 27,0 — 34,0 |
| Men | 27,0 — 35,0 | |
| 65 years - 120 years | Women | 27,0 — 35,0 |
| Men | 27,0 — 34,0 | |
Increasing MCH values:
- B12 deficiency and folate deficiency anemia;
- aplastic anemia;
- liver diseases;
- hypothyroidism;
- autoimmune anemia;
- smoking and drinking alcohol.
MCH Downgrade:
- Iron-deficiency anemia;
- anemia of chronic diseases;
- some types of hemoglobinopathies.
It should be taken into account that the MCH value is not specific; the indicator should be used to diagnose anemia only in combination with other indicators of a general blood test and biochemical blood test. MCHC (mean erythrocyte hemoglobin concentration) Determination method: calculated value
Units of measurement at the STUDIO DOCTOR medical center: g/dl. Alternative units: g/l. Conversion factor: g/l x 0.1 ==> g/dl.
Reference values
| Age, gender | Average hemoglobin concentration in erythrocytes, MSHC, g/dl | |
| Children | ||
| 1 day - 14 days | 28,0 — 35,0 | |
| 14 days - 4.3 weeks | 28,0 — 36,0 | |
| 4.3 weeks - 8.6 weeks | 28,0 — 35,0 | |
| 8.6 weeks - 4 months | 29,0 — 37,0 | |
| 4 months – 12 months | 32,0 — 37,0 | |
| 12 months - 3 years | 32,0 — 38,0 | |
| 3 years - 12 years | 32,0 — 37,0 | |
| 12 years - 15 years | Women | 32,0 — 36,0 |
| Men | 32,0 — 37,0 | |
| 15 years - 18 years | Women | 32,0 — 36,0 |
| Men | 32,0 — 36,0 | |
| 18 years - 45 years | Women | 32,0 — 36,0 |
| Men | 32,0 — 37,0 | |
| 45 years - 65 years | Women | 31,0 — 36,0 |
| Men | 32,0 — 36,0 | |
| 65 years - 120 years | Women | 32,0 — 36,0 |
| Men | 31,0 — 36,0 | |
Increased MSHC values: hereditary microspherocytic anemia. Decrease in MCHC values:
- Iron-deficiency anemia;
- anemia of chronic diseases;
- some types of hemoglobinopathies.
It should be taken into account that the MCHC value is not specific; the indicator should be used to diagnose anemia only in combination with other indicators of a general blood test and biochemical blood test.
Platelets Determination method: conductometry using the hydrodynamic focusing method.
Determination method: conductometry using the hydrodynamic focusing method. Units of measurement at the STUDIO DOCTOR medical center: thousand/μL (103 cells/μL). Alternate units: 109 cells/L. Conversion factors: 109 cells/l = 103 cells/µl = thousand/µl. Reference values:
| Age | Platelet concentration, thousand/µl (103 cells/µl) | |
| Children | boys | girls |
| 1 day - 14 days | 218 — 419 | 144 — 449 |
| 14 days - 4.3 weeks | 248 — 586 | 279 — 571 |
| 4.3 weeks - 8.6 weeks | 229 — 562 | 331 — 597 |
| 8.6 weeks - 6 months | 244 — 529 | 247 — 580 |
| 6 months - 2 years | 206 — 445 | 214 — 459 |
| 2 years - 6 years | 202 — 403 | 189 — 394 |
| Age | Platelet concentration, thousand/µl (103 cells/µl) | |
| 6 years - 120 years | 150 — 400 | |
Increased platelet concentration:
- physical stress;
- inflammatory diseases, acute and chronic;
- hemolytic anemia;
- anemia due to acute or chronic blood loss;
- conditions after surgical interventions;
- condition after splenectomy;
- oncological diseases, including hemoblastosis.
Decreased platelet concentration:
- pregnancy;
- B12 deficiency and folate deficiency anemia;
- aplastic anemia;
- viral and bacterial infections;
- taking medications that inhibit platelet production;
- congenital thrombocytopenia;
- splenomegaly;
- autoimmune diseases;
- conditions after massive blood transfusions.
Leukocytes Determination method: conductometry using the hydrodynamic focusing method. Units of measurement at the STUDIO DOCTOR medical center: thousand/μL (103 cells/μL). Alternate units: 109 cells/L. Conversion factors: 109 cells/l = 103 cells/µl = thousand/µl. Reference values:
| Age | Leukocyte concentration, thousand/µl (103 cells/µl) |
| 1 day – 12 months | 6,0 – 17,5 |
| 12 months – 2 years | 6,0 – 17,0 |
| 2 years – 4 years | 5,5 – 15,5 |
| 4 years – 6 years | 5,0 – 14,5 |
| 6 years – 10 years | 4,50 – 13,5 |
| 10 years – 16 years | 4,50 – 13,0 |
| 16 years – 120 years | 4,50 – 11,0 |
Increased leukocyte concentration:
- physiological leukocytosis (emotional and physical stress, exposure to sunlight, cold, food intake, pregnancy, menstruation);
- inflammatory processes;
- viral and bacterial infections;
- conditions after undergoing surgical interventions;
- intoxication;
- burns and injuries;
- heart attacks of internal organs;
- malignant neoplasms;
- hemoblastoses.
Decreased leukocyte concentration:
- viral and some chronic infections;
- taking medications (antibiotics, cytostatics, non-steroidal anti-inflammatory drugs, thyreostatics, etc.);
- autoimmune diseases;
- exposure to ionizing radiation;
- wasting and cachexia;
- anemia;
- splenomegaly;
- hemoblastoses.
How the research works
In modern medicine, equipment plays an important role in treatment. the same can be said about a blood test. On an empty stomach, blood is drawn either from a vein in the elbow or from a finger (this method is especially often practiced in the case of children), and then all the work is transferred to a modern analyzer, which conducts research quickly and with high quality, giving an accurate result .
It counts the number of red blood cells of different sizes per microliter of blood, calculates the average cell size and determines the degree of deviation from the norm of this indicator. The largest and smallest cells are also measured and the difference between this spread and the possible norm is analyzed. This indicator is recorded in femtoliters.
Of course, the equipment may not always be accurate; maximum accuracy of results can only be obtained by manual counting, but this is a very long and labor-intensive process, which is practically not used in modern medicine.
If deviations in this indicator occur, the blood test is performed again to obtain a reliable result, because the diagnosis cannot be made as a result of a single blood sample.
Preparation for the procedure
Since taking blood for a general analysis does not imply anything unusual, and the study itself is carried out regularly for almost all people, preparation does not require a person to take any special measures, but no one has canceled the standard recommendations before taking tests so that the results are reliable and correctly reflect the clinical picture:
- The RDW test is taken in the morning and on an empty stomach. Dinner in the evening of the previous day before donating blood should be light and at least 8 hours should pass between the last meal and the test, and preferably 12
- It is highly not recommended to drink alcohol 2 days before the test, as it can significantly distort the results
- It is advisable to give up fatty and fried foods, which have a negative effect on the body, 2 days in advance.
- You should not take a blood test after physiological and x-ray procedures
- It is recommended to refrain from smoking one hour before blood collection.
- It is advisable to exclude any physical and emotional stress; before the analysis, a 15-minute break and complete calm are required.
- Particular attention must be paid to the medications you are taking. Almost any medicine can distort the results of a blood test, so before donating blood you need to consult with a specialist: you may have to stop taking the medicine for a while to get an accurate clinical picture, or simply take the drug after the test.
If a repeat blood test is prescribed, it must be taken at the same time (since the composition of the blood may depend on the body’s circadian rhythms) and in the same laboratory. This is due to the fact that units and methods of measurement may vary between laboratories. Only if all recommended measures are followed will the result of the study be correct.
Indications for analysis
Determination of the number of neutrophils is included in the standard of performing a general blood test (CBC). A general blood test is recommended for all people without exception when referred for diagnostic or therapeutic procedures in a clinic or hospital.
Indications for determining the number of neutrophils:
- inflammatory diseases of any body system, for example, pneumonia or rheumatism;
- surgical inflammatory pathologies – appendicitis, peritonitis;
- significant burns to the body surface;
- destructive processes in the body, for example, myocardial infarction;
- oncological diseases;
- infectious pathologies – tuberculosis, measles, diphtheria, etc.;
- severe blood loss due to injury or internal bleeding;
- poisoning caused by chemicals and toxic substances.
Preparing for a blood test to determine the number of neutrophils
The number of neutrophils is determined during a general blood test. Before donating blood, a person is advised to refrain from drinking alcohol, fried or fatty foods. At least four hours before the procedure, the patient must completely avoid taking any products. Increased physical or psychological stress on the eve of the procedure should be limited.
Norms for the number of neutrophils in children and adults
In the results of a general clinical blood test, neutrophils are designated as NE and measured as a percentage.
- from 1 day to 15 days – 31.0%-56.0%;
- from 15 days to 1 year – 17.0%-51.0%;
- from 1 year to 2 years – 29.0%-54.0%;
- from 2 years to 5 years – 33.0%-61.0%;
- from 5 years to 7 years – 39.0%-64.0%;
- from 7 years to 9 years – 42.0%-66.0%;
- from 9 years to 11 years – 44.0%-66.0%;
- from 11 years to 15 years – 46.0%-66.0%;
- over 15 years old – 48.0%-78.0%.
Analysis for RDW in MedArt
The medical laboratory is equipped with modern high-precision equipment, high-quality reagents, all necessary consumables and qualified personnel. Our clients can rest assured of the reliability: if all preparation recommendations are followed, the results obtained will be 100% accurate. rdw in the blood test is reduced
Our team performs the work quickly, efficiently and with due understanding. Since there are people who are catastrophically afraid of any medical intervention, including blood sampling, we try to provide all our clients with the most comfortable and calm atmosphere, while performing all hematological studies at the highest level and providing accurate results.
With us, you can take a general blood test in a calm and comfortable environment and get a reliable result in the shortest possible time at an affordable price, without waiting in line for long hours, and then endlessly visiting doctors in an attempt to find out the result. We care about each of our clients and strive to do our work with the highest quality possible.