Removal of spider veins and visible vessels on the face. (Photocoagulation, photorejuvenation)
Spider veins on the cheeks, nose, red cheeks, purple face - all this is characteristic of the disease rosacea, its first manifestations are often called rosacea. This is a constitutional feature, it does not affect our well-being in any way, but it is of great importance in the perception of the people around us.
There are many options for camouflage, prevention, lifestyle rules, skincare cosmetics that slow down the process, but few techniques can remove dilated blood vessels that have already appeared on the face.
One of the most effective is a hardware procedure using IPL systems, also called photocoagulation or photorejuvenation. This can be done by a cosmetologist in his office. The processing area depends on the area of the process. Of course, what you won’t leave the consultation without is the wise advice of a cosmetologist
CLICK on one photo to view the entire photo gallery
Spider veins and redness. Before and after
Spider veins and redness can be of different shapes and locations on the face. Sometimes it’s a star on the nose, and sometimes there’s a sort of painful blush on the cheeks. And the desire to remove such a mark is understandable, because the foundation does not always cover this vascular feature.
Procedures using the IPL system allow you to do this in 1-4 visits. The number of procedures depends on the severity of the process and the individual characteristics of the skin. The interval between procedures is 3-5 weeks; it is better to plan them for the autumn-winter period (spring to April).
Recovery time is 1-3 days, redness and swelling are possible after the procedure. Immediately after, you can apply light makeup.
Cosmetologist's work:
- From 1 to 4 procedures
- Interval 3-5 weeks
- IPL system
- Rehabilitation up to 3 days
Spider veins on the face. Before and after
These are the spider veins that were on the face of a very young patient. There is no point in leaving them, since they themselves will not disappear and over time, on the contrary, they will become larger in size and quantity.
The procedure for removing them is quite short, a few flashes on the IPL system and you can go about your business. Locally there may be redness for 1-3 days, it goes away without a trace and can be covered with foundation from the very first day.
The number of procedures is 1-4, depending on many factors, all this is discussed at the preliminary consultation. It is better to carry out the procedure in a non-sunny period and not plan it a few days before your vacation.
Cosmetologist's work:
- From 1 to 4 procedures
- Short procedures
- IPL system
- Rehabilitation up to 3 days
Origin of vascular malformations
Malformations occur in the prenatal period. Geneticists are conducting a lot of research to study this phenomenon, but have not yet come to a definite concept. Therefore, the question of the causes of malformations remains not fully understood.
Congenital angiodysplasia (Parks-Weber-Rubashov syndrome) is characterized by the presence of pathological anastomosis (fistulas) between arteries and veins.
Arteriovenous anastomoses are often multiple and have a variety of sizes and shapes. Depending on the diameter, a distinction is made between macrofistulas, visible to the naked eye, and microfistulas, which are detected only by microscopic examination of the tissues of the limb.
The causes of the development of Parkes-Weber-Rubashov syndrome have not been definitively established. A number of authors consider it to be the result of mutations in the RASA1 gene, which encodes the p120-RasGAP protein, which is involved in the transmission of chemical signals from the extracellular space to the cell nucleus. However, exactly how these changes lead to specific vascular abnormalities in individuals with Parkes-Weber-Rubashov syndrome has not been established.
Pathological anastomosis are most often located in the area of the femoral, branches of the popliteal artery, as well as along the tibial arteries. Intensive discharge of arterial blood through arteriovenous fistulas leads to an increase in blood pressure in the veins.
Due to the increased functional load, the histological structure of the venous wall changes. There is a thickening of its muscular membrane and the formation of an internal elastic membrane (“arterialization” of the vein).
In the presence of fistulas, a significant part of the arterial blood enters the venous bed, bypassing the capillary network, so severe oxygen starvation occurs in the tissues and metabolic processes are disrupted. Due to venous hypertension, the load on the heart increases, which gradually leads to expansion of its boundaries and cardiac decompensation.
Wine stains on the face. Before and after
This is not the final result
Port-wine stains on the face and other open areas of the skin are very disturbing to owners. Some people get used to their presence over the years, while others come and remove them. Removing port-wine stains is not an easy task, but it is completely within the capabilities of both the patient and the doctor. This photo shows the result after 3 procedures and this is not the final result .
In addition to photo flashes on a device with an IPL system, special medications are prescribed for home care. The procedures are carried out at intervals of 3-5 weeks. Rehabilitation - redness and slight swelling of the treated area for 1 to 3 days.
Cosmetologist's work:
- Procedure interval 3-5 weeks
- Rehabilitation up to 3 days
- IPL system
- Not final result
Principles of treatment
The choice of treatment method should begin with a thorough assessment of the patient's condition. Based on this, it should be determined whether a particular method can solve the identified problem.
To treat deep-lying vessels, including those feeding hemangiomas and malformations, sclerotherapy - the introduction of a special substance into the vascular lumen, which causes destruction of the endothelium with the subsequent formation of a thin fibrous cord. In this way, vessels with a diameter of 4 mm or more can be eliminated.
The “gold standard” for removing small superficial vessels with a depth of up to 5 mm is the Nd : YAG laser . Its radiation has an optimal penetration depth and is well absorbed by blood hemoglobin. Laser therapy procedures are carried out without compromising the integrity of the skin, are well tolerated and do not require long-term rehabilitation. Nd:YAG laser can be combined with sclerotherapy or surgical removal of large and deep-lying vessels.
In the case of deep-lying vessels, they are often “covered” by a network of surface capillaries, which absorbs part of the laser radiation. Therefore, a combination of intense pulsed light (IPL) and a 1064 nm Nd:YAG laser is used for effective therapy. Both of these modules are part of the universal M22 platform from Lumenis.
Questions from our users:
- deep vessels removal
- remove blood vessels with laser
- vessels after laser resurfacing
- blood vessels treatment
Vessels on the face, redness and swelling. Before and after
The procedure is not very pleasant, but tolerable, and most importantly, quite fast. Rehabilitation takes an average of 24 hours; in rare cases, there may be redness and swelling for up to 3-5 days. Therefore, if you have not undergone a similar procedure before, it is better to schedule it before a couple of days off. Usually 3-4 procedures are required with an interval of 3-5 weeks, the effect is often visible after 1-2 procedures.
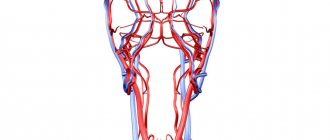
Human blood vessels
Blood circulates through the vessels that make up the systemic and pulmonary circulation.
All blood vessels consist of three layers:
- The inner layer of the vascular wall is formed by endothelial cells; the surface of the vessels inside is smooth, which facilitates the movement of blood through them.
- The middle layer of the walls provides the strength of blood vessels and consists of muscle fibers, elastin and collagen.
- The upper layer of the vascular walls is made up of connective tissue; it separates the vessels from nearby tissues.
Arteries
The walls of arteries are stronger and thicker than those of veins, since blood moves through them with greater pressure. Arteries carry oxygenated blood from the heart to the internal organs. The arteries of the dead are empty, which is revealed at autopsy, so it was previously believed that the arteries were air tubes. This is reflected in the name: the word “artery” consists of two parts; translated from Latin, the first part “aer” means air, and “tereo” means to contain.
Depending on the structure of the walls, two groups of arteries are distinguished:
- The elastic type of arteries are vessels located closer to the heart, these include the aorta and its large branches. The elastic framework of the arteries must be strong enough to withstand the pressure with which blood is thrown into the vessel from heart contractions. The elastin and collagen fibers that make up the frame of the middle wall of the vessel help resist mechanical stress and stretching.
Thanks to the elasticity and strength of the walls of the elastic arteries, blood continuously flows into the vessels and ensures constant circulation to nourish organs and tissues and supply them with oxygen. The left ventricle of the heart contracts and forcefully throws a large volume of blood into the aorta, its walls stretch to accommodate the contents of the ventricle. After relaxation of the left ventricle, blood does not flow into the aorta, the pressure is weakened, and blood from the aorta flows into other arteries into which it branches. The walls of the aorta regain their previous shape, since the elastin-collagen framework provides their elasticity and resistance to stretching. Blood moves through the vessels continuously, coming in small portions from the aorta after each heartbeat.
The elastic properties of the arteries also ensure the transmission of vibrations along the walls of the vessels - this is the property of any elastic system under mechanical influences, which is the cardiac impulse. The blood hits the elastic walls of the aorta, and they transmit vibrations along the walls of all the vessels of the body. Where the vessels come close to the skin, these vibrations can be felt as a weak pulsation. Pulse measurement methods are based on this phenomenon.
- Muscular-type arteries in the middle layer of the walls contain a large number of smooth muscle fibers. This is necessary to ensure blood circulation and continuity of its movement through the vessels. Muscular-type vessels are located further from the heart than elastic-type arteries, so the force of the cardiac impulse in them weakens; to ensure further movement of blood, contraction of muscle fibers is necessary. When the smooth muscles of the inner layer of the arteries contract, they narrow, and when they relax, they expand. As a result, blood moves through the vessels at a constant speed and promptly enters organs and tissues, providing them with nutrition.
Another classification of arteries determines their location in relation to the organ to which they supply blood. Arteries that pass inside an organ, forming a branching network, are called intraorgan. The vessels located around the organ, before entering it, are called extraorgan. Lateral branches that arise from the same or different arterial trunks may reconnect or branch into capillaries. At the point of their connection before they begin to branch into capillaries, these vessels are called anastomosis or anastomosis.
Arteries that do not have an anastomosis with adjacent vascular trunks are called terminal. These, for example, include the arteries of the spleen. The arteries that form the anastomosis are called anastomosing; most arteries belong to this type. The terminal arteries have a greater risk of blockage by a blood clot and a high predisposition to a heart attack, which can result in the death of part of the organ.
In the last branches, the arteries become very thin; such vessels are called arterioles, and the arterioles already pass directly into capillaries. Arterioles contain muscle fibers that perform a contractile function and regulate the flow of blood into the capillaries. The layer of smooth muscle fibers in the walls of arterioles is very thin compared to an artery. The place where the arteriole branches into capillaries is called the precapillary; here the muscle fibers do not form a continuous layer, but are located diffusely. Another difference between a precapillary and an arteriole is the absence of a venule. The precapillary gives rise to numerous branches into the smallest vessels - capillaries.
Capillaries
Capillaries are the smallest vessels, the diameter of which varies from 5 to 10 microns; they are present in all tissues, being a continuation of the arteries. Capillaries provide tissue metabolism and nutrition, supplying all structures of the body with oxygen. In order to ensure the transfer of oxygen and nutrients from the blood to the tissues, the capillary wall is so thin that it consists of only one layer of endothelial cells. These cells are highly permeable, so through them substances dissolved in the liquid enter the tissues, and metabolic products return to the blood.
The number of working capillaries in different parts of the body varies - they are concentrated in large numbers in working muscles, which need constant blood supply. For example, in the myocardium (the muscular layer of the heart) up to two thousand open capillaries are found in one square millimeter, and in skeletal muscles there are several hundred capillaries in the same area. Not all capillaries function at the same time - many of them are in reserve, in a closed state, to start working when necessary (for example, during stress or increased physical activity).
Capillaries anastomose and, branching, form a complex network, the main links of which are:
- Arterioles - branch into precapillaries;
- Precapillaries are transitional vessels between arterioles and the capillaries themselves;
- True capillaries;
- Postcapillaries;
- Venules are the transition points between capillaries and veins.
Each type of vessel that makes up this network has its own mechanism for transferring nutrients and metabolites between the blood they contain and nearby tissues. The muscles of larger arteries and arterioles are responsible for the movement of blood and its flow into the smallest vessels. In addition, regulation of blood flow is also carried out by the muscular sphincters of the pre- and post-capillaries. The function of these vessels is mainly distributive, while true capillaries perform a trophic (nutritional) function.
Vienna
Veins are another group of vessels, the function of which, unlike arteries, is not to deliver blood to tissues and organs, but to ensure its flow to the heart. To do this, blood moves through the veins in the opposite direction - from tissues and organs to the heart muscle. Due to the difference in functions, the structure of veins is somewhat different from the structure of arteries. The factor of strong pressure that blood exerts on the walls of blood vessels is much less manifested in veins than in arteries, therefore the elastin-collagen framework in the walls of these vessels is weaker, and muscle fibers are represented in smaller quantities. This is why veins that do not receive blood collapse.
Similar to arteries, veins branch widely to form networks. Many microscopic veins merge into single venous trunks, which lead to the largest vessels flowing into the heart.
The movement of blood through the veins is possible due to the action of negative pressure on it in the chest cavity. Blood moves in the direction of the suction force into the heart and chest cavity; in addition, its timely outflow is ensured by the smooth muscle layer in the walls of blood vessels. The movement of blood from the lower extremities upward is difficult, therefore, in the vessels of the lower part of the body, the muscles of the walls are more developed.
In order for blood to move towards the heart, and not in the opposite direction, valves are located in the walls of the venous vessels, represented by a fold of endothelium with a connective tissue layer. The free end of the valve freely directs blood in the direction of the heart, and the outflow is blocked back.
Most veins run adjacent to one or more arteries: small arteries usually have two veins near them, and larger ones usually have one vein near them. Veins, which do not accompany any arteries, are found in the connective tissue under the skin.
The walls of larger vessels are supplied with food by arteries and veins of smaller sizes, extending from the same trunk or from neighboring vascular trunks. The entire complex is located in the connective tissue layer surrounding the vessel. This structure is called the vascular sheath.
The venous and arterial walls are well innervated, contain a variety of receptors and effectors, well connected with the governing nerve centers, due to which the automatic regulation of blood circulation is carried out. Thanks to the work of reflexogenic areas of blood vessels, nervous and humoral regulation of metabolism in tissues is ensured.
Vessels (rosacea). Before and after
Red cheeks, red face, spider veins, rosacea, rosacea
Red cheeks, red face, spider veins, rosacea, rosacea - there are many names, but the essence is the same. Expansion of the superficial vascular network is a genetic predisposition that is enhanced by many external factors (air temperature, nutrition, stress).
Such redness on the face today can only be removed using IPL, broadband intense light, this is a hardware technique. 3-4 procedures at intervals of a month, and excellent results.
Share this post
Table of contents
- Etiology and pathogenesis
- Clinical manifestations
- Principles of treatment
Deep-lying vessels are pathologically altered capillaries that feed hemangiomas and malformations, as well as enlarged venules located in the skin at a depth of up to 5 mm.
In our company you can purchase the following equipment for removing deep-lying vessels:
- M22 (Lumenis)
Conditions in which deep-lying vessels are present in the skin include the following:
- Infantile hemangiomas
- Capillary hemangiomas
- Cavernous hemangiomas
- Vascular malformations
- Phlebeurysm