Detailed description of the study
Protein S is a plasma protein that prevents blood clotting, that is, it is a natural anticoagulant. It enters the blood, where some binds to another protein, and some remains in free form. It is with its help that the protein manifests its function.
When a vessel is damaged, a complex of platelets is formed to stop bleeding, which covers the damaged wall. Next, this complex receives blood plasma proteins - coagulation factors that contribute to the formation of a dense blood clot. To maintain normal blood flow, thrombus formation processes must be balanced by the action of the anticoagulant system.
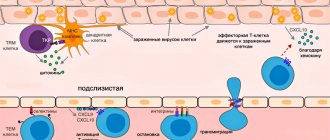
Protein S is a component of the anticoagulant system. It is a cofactor (helps in the work) of another anticoagulant - protein C. Both proteins are formed in the liver; their synthesis requires vitamin K. Normally, they disrupt the activity of factors V and VIII, that is, they prevent the formation of blood clots.
Determining the amount of protein S is of particular importance in the diagnosis of congenital deficiency (thrombophilia). This disease manifests itself with various thromboses, mainly at a young age (up to 50 years), and is not associated with risk factors for thrombosis, for example, prolonged bed rest, obesity, and dehydration.
With protein S deficiency, thrombosis of the superficial veins of the lower extremities is common. A person experiences pain, redness, and increased temperature at the site of the lesion. With thrombosis of the deep veins of the legs, swelling of the limb appears.
A particularly severe manifestation of thrombophilia is pulmonary embolism (PE), the causes of which are deep thrombosis of the veins of the legs, pelvic organs and the inferior vena cava. The blood clot enters the pulmonary artery and completely or partially blocks the vessel. The clinical manifestations of PE vary depending on the caliber of the artery. A person notices sudden chest pain, coughing, and breathing and heart problems may occur. Massive pulmonary embolism is accompanied by pulmonary edema.
A decrease in the amount of protein S negatively affects the course of pregnancy. Thrombophilia can lead to frozen pregnancy, spontaneous abortions due to the formation of microthrombi in the vessels of the placenta. Problems arise already at the beginning of gestation: the attachment (implantation) of the fetus to the wall of the uterus is disrupted. In later pregnancy, thrombophilia increases the risk of placental abruption. Reduced blood supply can lead to intrauterine growth retardation. Therefore, analysis for protein S and other coagulation proteins is important when planning pregnancy, especially if there have been previous episodes of thrombosis.
Acquired thrombophilias are also distinguished. They are usually temporary and associated with medications that interfere with the absorption of vitamin K, chronic infections, and severe liver and kidney diseases. Thus, liver diseases (hepatitis, cirrhosis) lead to a decrease in protein synthesis, including the production of protein S.
Determining the amount of protein S along with other tests helps to identify the cause of thrombosis and detect thrombophilia.
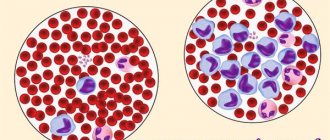
Blood plasma proteins
Of the 9–10% of the dry residue of blood plasma, proteins account for 6.5–8.5%. Using the method of salting out with neutral salts, blood plasma proteins can be divided into three groups: albumins, globulins and fibrinogen. The normal content of albumin in blood plasma is 40–50 g/l, globulin – 20–30 g/l, fibrinogen – 2.4 g/l. Blood plasma devoid of fibrinogen is called serum.
The synthesis of blood plasma proteins occurs primarily in the cells of the liver and reticuloendothelial system. The physiological role of blood plasma proteins is multifaceted.
1. Proteins maintain colloid osmotic (oncotic) pressure and thereby maintain a constant blood volume. The protein content in plasma is significantly higher than in tissue fluid. Proteins, being colloids, bind water and retain it, preventing it from leaving the bloodstream. Despite the fact that oncotic pressure makes up only a small part (about 0.5%) of the total osmotic pressure, it determines the predominance of the osmotic pressure of the blood over the osmotic pressure of the tissue fluid. It is known that in the arterial part of the capillaries, as a result of hydrostatic pressure, protein-free blood fluid penetrates into the tissue space. This occurs up to a certain point - the “turning point”, when the falling hydrostatic pressure becomes equal to the colloid-osmotic pressure. After the “turning” moment, a reverse flow of fluid from the tissue occurs in the venous part of the capillaries, since the hydrostatic pressure has become less than the colloid osmotic pressure. Under other conditions, as a result of hydrostatic pressure in the circulatory system, water would seep into the tissues, which would cause swelling of various organs and subcutaneous tissue.
2. Plasma proteins take an active part in blood clotting. A number of proteins, including fibrinogen, are the main components of the blood coagulation system.
3. Plasma proteins to a certain extent determine the viscosity of blood, which, as noted, is 4–5 times higher than the viscosity of water and plays an important role in maintaining hemodynamic relations in the circulatory system.
4. Plasma proteins take part in maintaining a constant blood pH, as they constitute one of the most important buffer systems in the blood.
5. The transport function of blood plasma proteins is also important: combining with a number of substances (cholesterol, bilirubin, etc.), as well as with drugs (penicillin, salicylates, etc.), they transport them to tissues.
6. Plasma proteins play an important role in immune processes (especially immunoglobulins).
7. As a result of the formation of non-dialyzable complexes with plasma proteins, the level of cations in the blood is maintained. For example, 40–50% of serum calcium is bound to proteins, and a significant portion of iron, magnesium, copper and other elements are also bound to whey proteins.
8. Finally, blood plasma proteins can serve as a reserve of amino acids. Modern physicochemical methods have made it possible to discover and describe about 100 different protein components of blood plasma. The electrophoretic separation of blood plasma (serum) proteins has acquired particular importance.
In the blood serum of a healthy person, electrophoresis on paper can detect 5 fractions: albumin, α1-, α2-, β-, γ-globulins. Using agar gel electrophoresis, 7–8 fractions are isolated in blood serum, and with starch or polyacrylamide gel electrophoresis, up to 16–17 fractions are isolated. It should be remembered that the terminology of protein fractions obtained by various types of electrophoresis has not yet been completely established. When changing electrophoresis conditions, as well as during electrophoresis in different media (for example, in starch or polyacrylamide gel), the migration rate and, consequently, the order of protein zones can change.
An even larger number of protein fractions (over 30) can be obtained by immunoelectrophoresis (Fig. 17.1). This method is a unique combination of electrophoretic and immunological methods for analyzing proteins. In other words, the term “immunoelectrophoresis” means carrying out electrophoresis and precipitation reactions in the same medium, i.e. directly on the gel block. With this method, using a serological precipitation reaction, a significant increase in the analytical sensitivity of the electrophoretic method is achieved.
Previous page | Next page
CONTENT
More on the topic:
- Blood plasma proteins - Visual biochemistry
References
- Russian clinical guidelines for the diagnosis, treatment and prevention of venous thromboembolic complications (VTEC). Phlebology, 2015. - V. 2. - 51 p.
- Galayko, M.V., Rybina, O.V., Litvinenko, M.S. and others. Thrombophilia and pregnancy. Clinical oncohematology, 2021. - V. 10(3). — P. 409–22.
- Pathophysiology: textbook / ed. V.V. Novitsky, E.D. Goldberg, O.I. Urazova. — 4th ed., revised. and additional - M.: GEOTAR-Media, 2009. - T. 2. - 640 p.
- Tun, A., Gupta, K., Tuma, F. Protein S Deficiency Ashish Gupta. StatPearls, 2021.
Blood test indicator table
Decoding a biochemical blood test is a comparison of the results obtained with normal values. The analysis form contains a complete list of indicators determined by the biochemical laboratory and their reference values.
The norms for biochemical blood test indicators in adults are shown in the table:
| Analysis: | Men: | Women: |
| Total protein | 64-84 g/l. | 64-84 g/l. |
| Hemoglobin | 130-160 g/l | 120-150 g/l. |
| Haptoglobin | 150-2000 mg/l | 150-2000 mg/l |
| Glucose | 3.30-5.50 mmol/l. | 3.30-5.50 mmol/l. |
| Urea | 2.5-8.3 mmol/l. | 2.5-8.3 mmol/l. |
| Creatinine | 62-115 µmol/l | 53-97 µmol/l. |
| Cholesterol | 3.5-6.5 mmol/l. | 3.5-6.5 mmol/l. |
| Bilirubin | 5-20 µmol/l. | 5-20 µmol/l. |
| AlAT (ALT) | up to 45 units/l. | up to 31 units/l. |
| ASAT (AST) | up to 45 units/l. | up to 31 units/l. |
| Lipase | 0-190 units/l. | 0-190 units/l. |
| Alpha amylase | 28-100 units/l. | 28-100 units/l. |
| Pancreatic amylase | 0-50 units/l. | 0-50 units/l. |
Each of the criteria indicated in the table reflects the condition of one or more human organs. And a combination of some of them sometimes makes it possible to make an accurate diagnosis or direct the diagnostic process in the right direction.
Sometimes it is enough to establish a final diagnosis based on deviations from the norm of one or more parameters. But much more often, a full diagnosis requires other results of additional research methods and an assessment of the clinical picture of the disease.
Total protein
Total protein is the total concentration of proteins found in the blood. Proteins take part in all biochemical reactions of the body - they transport various substances, act as catalysts for reactions, and participate in immune defense.
Normal levels of protein in the blood are 64-84 g/l. If the protein is higher than this, the body may be susceptible to infection. In addition, the cause of increased protein may be arthritis, rheumatism, or the onset of cancer. With a low protein content in the blood, the likelihood of liver disease increases many times, as well as problems with the intestines and kidneys. The most difficult diagnosis for low protein is cancer.
Albumen
This protein is produced by the liver and is considered the main protein in the blood plasma. In general, experts distinguish albumins as a separate protein group, called protein fractions.
An increase in the concentration of albumin in the blood (hyperalbuminemia) may be associated with the following pathologies:
- dehydration, or dehydration (loss of fluid from the body through vomiting, diarrhea, profuse sweating);
- extensive burns.
A reduced albumin level is observed in smoking patients and in women during pregnancy and breastfeeding. In other people, a decrease in albumin may indicate various liver pathologies (for example, cirrhosis, hepatitis, or oncology), or intestinal inflammation of an infectious nature (sepsis). In addition, in case of heart failure or cancer, burns or fever, various injuries or drug overdose, the albumin in the blood will be lower than normal.
Glucose (sugar)
The most common indicator of carbohydrate metabolism is blood sugar. Its short-term increase occurs during emotional arousal, stress reactions, pain attacks, and after eating. The norm is 3.5-5.5 mmol/l (glucose tolerance test, sugar load test).
Sugar is elevated - diabetes, endocrine disorders, pancreatitis, pancreatic tumor, cerebral hemorrhage, chronic liver and kidney damage, myocardial infarction, cystic fibrosis.
Sugar is low - damage to the liver and pancreas, hypothyroidism, stomach or adrenal cancer, arsenic poisoning or certain medications, alcohol intoxication.
Uric acid
The main breakdown product of the main component of nucleic acids - purine bases. Since it is not used further in metabolic processes, it is excreted unchanged by the kidneys. The normal level in blood plasma is 0.16-0.44 mmol/l.
An increase in uric acid levels in the blood indicates:
- renal failure;
- leukemia, lymphoma;
- prolonged fasting;
- alcohol abuse;
- overdose of salicylates and diuretics.
A decrease in the level of uric acid in the blood can be observed during treatment with piperazine drugs, allopurinol, prebenecid, ACTH, sometimes with hepatitis, anemia.
Urea
It is a consequence of the breakdown of proteins. The permissible amount of this substance in a person’s blood changes with age. Often, the level of urea goes through the roof in patients who have pathologies in their kidneys: doctors prescribe a similar blood test to diagnose and predict the disease.
A decrease in the level of urea in the blood can be triggered by reasons that are physiological (pregnancy, fasting, excessive exercise), or pathological (celiac disease, cirrhosis of the liver, heavy metal poisoning).
Creatinine
This substance, like urea, is a product of protein metabolism and is also excreted by the kidneys. Creatinine is a product of metabolic processes occurring in skeletal muscles, and to a lesser extent in the brain. Accordingly, its level will depend on the condition of the kidneys and muscles.
Increased creatinine is observed in renal failure, severe injuries with muscle damage, increased thyroid function, and after the use of certain anti-inflammatory and antibacterial agents. Moderately high creatinine is found in athletes.
Alanine aminotransferase (ALT, AlAt)
This indicator, along with AST, is used in medical practice for laboratory diagnosis of liver damage. Alanine aminotransferase is synthesized intracellularly, and normally only a small part of this enzyme enters the blood. When the liver is damaged (hepatitis, cirrhosis) as a result of cytolysis (cell destruction), this enzyme enters the blood, which is detected by laboratory methods.
The level of this transaminase may also increase during myocardial infarction and other conditions. An increase in ALT that exceeds an increase in AST is characteristic of liver damage; if the AST indicator increases more than the ALT increases, then this, as a rule, indicates problems with myocardial (heart muscle) cells.
Aspartate aminotransferase (AST, AST)
A cellular enzyme involved in amino acid metabolism. AST is found in the tissues of the heart, liver, kidneys, nervous tissue, skeletal muscles and other organs. An AST blood test may show an increase in AST in the blood if the body has a disease such as:
- myocardial infarction;
- viral, toxic, alcoholic hepatitis;
- angina pectoris;
- acute pancreatitis;
- liver cancer;
- acute rheumatic carditis;
- heavy physical activity;
- heart failure.
AST is elevated in skeletal muscle injuries, burns, heat stroke, and as a result of cardiac surgery.
Alkaline phosphatase
Many laboratories automatically include this enzyme in their biochemical analysis. From a practical point of view, only an increase in the activity of this enzyme in the blood may be of interest.
This is evidence of either intrahepatic stagnation of bile in the small bile ducts, which occurs with mechanical and parenchymal jaundice, or progressive osteoporosis or destruction of bone tissue (myeloma, aging of the body).
Cholesterol
A component of fat metabolism, it is involved in the construction of cell membranes, the synthesis of sex hormones and vitamin D. There is total cholesterol, low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol.
Degrees of increased cholesterol in the blood:
- 5.2-6.5 mmol/l – mild degree of increase in the substance, a risk zone for atherosclerosis;
- 6.5-8.0 mmol/l – a moderate increase, which is corrected by diet;
- over 8.0 mmol/l – a high level requiring drug intervention.
An increase in cholesterol levels in the serum or blood plasma is an argument in favor of atherosclerosis, hypothyroidism (low activity of the thyroid gland), chronic hepatitis, decompensated diabetes mellitus, obstructive jaundice.
This indicator decreases when:
- malignant liver tumors;
- cirrhosis of the liver;
- rheumatoid arthritis;
- hyperfunction of the thyroid and parathyroid glands;
- starvation;
- malabsorption of substances;
- chronic obstructive pulmonary diseases.
Bilirubin
Bilirubin is a yellow-red pigment that is formed when hemoglobin breaks down in the spleen, liver and bone marrow. Its normal level in the blood of children and adults is 3.4–20.5 µmol/l.
If the table with the examination results contains an elevated level of bilirubin, then the doctor can diagnose one of the following diseases in adults:
- cholelithiasis;
- pancreatic tumors;
- inflammatory diseases of the biliary tract.
If bilirubin is below normal, then the patient may have one of the following diseases:
- acute viral hepatitis;
- bacterial liver damage (leptospirosis, brucellosis, etc.);
- toxic hepatitis;
- medicinal product;
- neoplasms in the liver and primary biliary cirrhosis;
- hemolytic anemia of various etiologies.
Bilirubin, formed as a result of the breakdown of hemoglobin (indirect), is released into the blood, where it binds to albumin and is transported to the liver. In liver cells, bilirubin combines with glucuronic acid. This bilirubin bound to glucuronic acid is called direct bilirubin.
Amylase
Breaks down carbohydrates from food and ensures their digestion. Contained in the salivary glands and pancreas. There is alpha-amylysis (diastase) and pancreatic amylase.
- alpha-amylase rate: 28-100 units/l.
- pancreatic amylase rate: 0-50 units/l.
A high amylase content in a biochemical blood test indicates: peritonitis, pancreatitis, diabetes mellitus, pancreatic cyst, stone, cholecystitis or renal failure.
Decreased alpha-amylase: thyrotoxicosis; myocardial infarction; complete necrosis of the pancreas; toxicosis of pregnant women.
Potassium
Another important intracellular electrolyte. Its normal content in the body ranges from 3.5 to 5.5 mmol per liter.
Reduced potassium content:
- excess hormones of the adrenal cortex (including taking dosage forms of cortisone);
- chronic fasting (failure to receive potassium from food);
- prolonged vomiting, diarrhea (loss with intestinal juice);
- renal dysfunction;
- cystic fibrosis.
Increased potassium content:
- dehydration;
- acute renal failure (impaired renal excretion); ,
- adrenal insufficiency.
- cell damage (hemolysis - destruction of blood cells, severe starvation, convulsions, severe injuries).
The condition when potassium is elevated is called hyperkalemia, and when it is low, hypokalemia.
Sodium
Sodium does not directly participate in metabolism. It is completely abundant in the extracellular fluid. Its main function is to maintain osmotic pressure and pH. Sodium excretion occurs in the urine and is controlled by the adrenal hormone aldosterone.
Sodium reduction:
- decreased concentration due to increased fluid volume (diabetes mellitus, chronic heart disease)
- failure, liver cirrhosis, nephrotic syndrome, edema).
- loss of an element (abuse of diuretics, kidney pathology, adrenal insufficiency).
Increased sodium content:
- increased function of the adrenal cortex;
- excess salt intake;
- loss of extracellular fluid (profuse sweat, severe vomiting and diarrhea, increased urination in diabetes insipidus);
- violation of the central regulation of water-salt metabolism (pathology of the hypothalamus, coma).
An increase in a microelement is called hypernatremia, and a decrease is called hyponatremia.
Total protein analysis
Total protein in the blood is the main indicator on which to focus when assessing amino acid metabolism in the human body. This analysis is never prescribed separately - it is always carried out in conjunction with other studies. Assessing the level of total protein in the blood is necessary for diagnosing a number of diseases: pathologies of the kidneys, liver, oncology, and various infections. This analysis is also prescribed to monitor the effectiveness of ongoing therapeutic measures. In order to conduct a quantitative analysis to determine total protein, a sample of the patient’s biological material is required - venous blood plasma. Normal levels of protein in the blood are from 65 to 85 g/l. The research will take no more than 1 day.
Total blood protein is a general indicator of the concentration of all organic proteins that circulate in the blood plasma. The main substances isolated during the study are albumins and globulins. Albumin is a substance produced by the liver. Its concentration is about 60% of the total amount of proteins present in the human body. Globulins are a substance that is formed in the liver, lymphocytes and plasma cells. The concentration of this protein is not a constant indicator, which depends on the rate of its production from amino acids. In turn, this speed is influenced by a number of factors.
If the body produces excessive amounts of protein, it is not retained in the body. Passing a long way through the entire body, the substance eventually ends up in the kidneys and is converted into uric acid, which leaves the body in urine and feces.
The main task of blood serum proteins is to organize correct homeostasis in the body. Protein is involved in almost all biochemical processes of the human body. Plasma proteins are responsible for maintaining the normal state of the blood. They directly affect the degree of blood fluidity. In addition, proteins perform a transport function - they carry various substances to human tissues and organs: lipids, pigments, hormones, fragments of drugs.
Proteins are also responsible for the correct functioning of the human immune system. The production of antibodies, immunoglobulins and other protective cells of the body directly depends on their concentration in the blood.
Assessing the level of total protein is one of the stages of complex biochemical screening. Using the results of this analysis, surgeons and resuscitators evaluate the effectiveness of intensive care for critically ill patients, and also monitor patients after various surgical interventions. Also, the results of this analysis are necessary in cardiology and nephrology. Using the data obtained, doctors can determine the cause of edema, as well as impaired renal excretory function.
Fibrinogen - role and norm in the blood (Fibrinogen, FF, FA)
Fibrinogen is a soluble plasma protein synthesized in the liver and is directly involved in the formation of a thrombus (blood clot) after a violation of the integrity of the vascular wall. This indicator is determined in a coagulogram (hemostasiogram) - a special test for clotting.
Under the influence of special factors, Fibrinogen at the site of damage to the blood vessel is converted into insoluble fibrin. Its threads intertwine with each other and create a dense network, to which, as if on a filter, platelets settle and create a durable temporary patch to stop bleeding. The lower the FF level, the longer it takes for a blood clot to form. The norm is from 2 to 4 g/l. A change, either upward or downward, is fraught with serious consequences.
A decrease in concentration is observed in the case of:
- Liver failure (loss of the ability to synthesize the required amount of proteins due to hepatitis or cirrhosis);
- Poisoning with snake venom;
- Deficiency of ascorbic acid and vitamin B12;
- Long-term infusion therapy or after massive transfusion of blood-substituting solutions and components;
- Pathological intravascular coagulation (DIC syndrome).
The consequences of low fibrinogen are:
- Risk of hemorrhage;
- Hemorrhagic stroke;
- Blood loss during invasive interventions;
- Bleeding gums;
- Hemoptysis;
- The appearance of bloody impurities in the stool;
- Difficult to stop bleeding from wounds and abrasions.
There are a sufficient number of reasons leading to an increase in concentration:
- Loss of body fluids (vomiting, diarrhea, polyuria, superficial extensive burns);
- Malignant neoplasms, systemic tumor processes;
- The presence of acute inflammation or exacerbation of chronic;
- Hormonal therapy (contraceptives).
High Fibrinogen increases the risk of pathological clots, especially against the background of atherosclerotic damage to blood vessels. It leads to:
- Myocardial infarction and other cardiovascular diseases;
- Ischemic stroke;
- Thrombosis of internal organs and limbs.
There are no specific signs of high or low FA, so its determination should always be carried out before planning any surgical interventions, as well as in the case of increased bleeding, the presence of ischemic symptoms of any localization, and after severe infections.