Pathologies of the cardiovascular system require regular monitoring and special care for the patient. They are dangerous due to the rapid development of an acute condition and sudden death of the patient. To maintain a stable condition, the patient must live according to the regimen prescribed by the doctor and control his emotional state, but this is not always possible without outside support. People with cardiovascular pathologies often suffer from increased anxiety and fear of death, they are afraid of being alone for a long time or of being without vital medications at hand. Such patients require the help of a professional caregiver at home or in a boarding house. Peace, proper routine, care and attention to their needs have a calming effect on the wards and improves their well-being.
Principles of caring for patients with cardiovascular diseases
To prevent the development of acute conditions in the patient, the nurse carries out a whole range of preventive measures every day. This is painstaking work that requires discipline and patience from both the caregiver and the ward, but the result is worth it. Strengthening the heart muscle leads to an overall improvement in physical and psychological condition.
Proper care for patients reduces the risk of pathologies of the cardiovascular system. It assumes:
- daily monitoring of blood pressure and pulse,
- compliance with diet and medication,
- regular cleansing of the body,
- therapeutic massage to improve blood circulation,
- moderate physical activity,
- prevention of thrombosis and thromboembolism in bedridden patients,
- creating a calm environment and psychological support.
The caregiver must be able to recognize signs of dangerous conditions and have emergency medical skills. The life of the ward may depend on his qualifications.
Symptoms of Cardiovascular Diseases
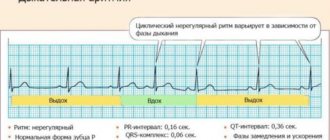
Arrhythmia
An accelerated or slowed heartbeat is not dangerous in itself, but it may be the first manifestation of a serious pathology. Treated with special medications
Dyspnea
Stagnation of venous blood leads to excess carbon dioxide and lack of oxygen in cells. An acute attack is called cardiac asthma and in severe cases is accompanied by pulmonary edema. A patient with shortness of breath needs fresh air first. In addition, tourniquets on the legs and inhalation of humidified oxygen may be required.
Edema
Fluid retention in the body occurs due to overflowing of the veins and blood particles leaving their walls. Swelling reduces the protective properties of the skin, causing a feeling of nausea and bloating in the abdomen. To normalize fluid outflow, diet and diuretics are required.
Pain in the heart area
This is a sign of poor blood supply to the organ. With prolonged oxygen starvation, biochemical changes occur in the heart muscle, manifested by pressing sensations, weakness, and profuse sweating. In mild cases, the pain is relieved with a validol or nitroglycerin tablet. However, an attack can be caused by a developing myocardial infarction. If the syndrome does not go away even after taking medications, the patient requires emergency hospitalization
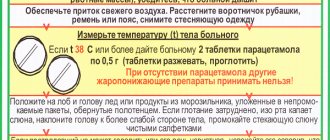
Increased blood pressure
Regular increases in blood pressure cause the development of hypertension and concomitant dysfunction of the brain and kidneys. To avoid this, the patient needs to get enough sleep, measure blood pressure twice a day, give up bad habits and take medications regularly. If there is a sharp increase in blood pressure (hypertensive crisis), you need to call an ambulance
Collapse
This is a sharp decrease in blood pressure, provoked by acute vascular insufficiency, myocardial infarction, severe bleeding, including internal bleeding, poisoning or infection. In this state, the patient’s breathing and pulse become more frequent, and the extremities become cold. Possible loss of consciousness. The patient needs to be warmed and positioned so that blood flows to the brain. Caffeine-containing medications are recommended to raise blood pressure.
"Nursing process in acute cardiovascular failure"
Nursing care for acute cardiac and vascular failure
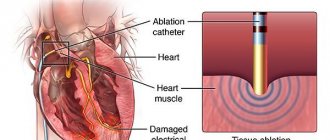
Acute heart failure (AHF)
- this is a sudden decrease in contractility (heart function) leading to disturbances in intracardiac hemodynamics, stagnation of blood circulation, which can lead to disruption of the functions of individual organs.
O.S.N. can be of two types: left ventricular (left type) and right ventricular (right type).
Acute heart failure is also called acute left ventricular failure, since the main pathophysiological mechanism is a sharp decrease in the contractile function of the left ventricle.
Etiology
Hypertension, aortic heart defects, acute myocardial infarction (as is known, the infarction is most often localized in the left ventricle), severe forms of diffuse myocarditis, post-infarction cardiosclerosis (especially with chronic post-infarction aneurysm of the left ventricle).
Pathogenesis
The essence of hemodynamic disorders in acute heart failure is that a sharp decrease in the contractile function of the left ventricle leads to excessive stagnation and accumulation of blood in the vessels of the pulmonary circulation. As a result, gas exchange in the lungs is disrupted, the oxygen content decreases and the carbon dioxide content in the blood increases. In this regard, the oxygen supply to organs and tissues deteriorates; The central nervous system is especially sensitive. In patients, the excitability of the respiratory center increases, which leads to the development of shortness of breath, reaching the level of suffocation. Stagnation of blood in the lungs as it progresses is accompanied by the leakage of serous fluid into the lumen of the alveoli, which threatens the subsequent development of pulmonary edema.
Clinic
A typical attack of cardiac asthma usually develops during sleep, at night. The patient suddenly wakes up from an acute feeling of lack of air and fear of death.
At the same time, a hacking cough appears
.
Severe shortness of breath with predominantly
difficulty inhaling
forces the patient to sit on the edge of the bed or stand up and go to an open window.
The facial expression is pained, the eyes express concern. The skin is initially pale and then acquires a bluish tint; increased sweating is noted. The neck veins become swollen. Breathing is rapid. A dry cough may then be accompanied by the production of a small amount of mucous sputum mixed with blood.
If circulatory disorders in the pulmonary circle progress, then a copious discharge of liquid, foamy sputum mixed with blood appears or a uniformly
pink
colored liquid is released (this sign is characteristic of developing
pulmonary edema
).
Objectively:
When examining the respiratory organs, shortness of breath is noted (the number of breaths per minute reaches 40-60). At the height of an attack of cardiac asthma, against the background of weakened vesicular breathing, moist, silent, fine-bubble rales are heard in the lower parts of the lungs. In some cases, an attack of cardiac asthma occurs without moist rales. In some patients, dry wheezing may be heard (usually characteristic of an attack of bronchial asthma), the appearance of which is caused by the development of bronchospasm in response to developing circulatory disorders in the pulmonary vessels. The most characteristic changes are noted when examining the circulatory system: frequent, often arrhythmic pulse, muffled heart sounds. Blood pressure may be elevated at the beginning of an attack and then decrease; sometimes blood pressure is low from the very beginning. If the attack is accompanied by severe shortness of breath, cough with sputum and a large number of coarse wheezing in the lungs, then it is difficult to listen to extremely muffled heart sounds; in this case, pulse and blood pressure will be more accurate indicators of heart function.
The attack may last several minutes and end without any intervention. More often the attacks have a protracted course. In such cases, untimely provision of medical care can lead to death as a result of the development of pulmonary edema, a drop in blood pressure, or sudden depression of the respiratory center.
Urgent Care
for left ventricular failure:
1. Call a doctor urgently
2.Sit the patient with legs down, with back support at 15' - apply 3 tourniquets to the thighs and 1 arm/change.
3. Influx of fresh air, give oxygen inhalation through a defoamer (alcohol or antifomsilane).
4.Give a nitroglycerin tablet under the tongue (not if A/D is below 100 ml Hg)
5. As prescribed by the doctor, administer morphine 1% - 1 ml intravenously.
6. Neuroleptanalgesia – fentanyl with droperidol 0.25% = 1-2 ml.
7. If A/D is normal, administer 40-160 mg of furosemide (Lasix) intravenously.
For high A/D, ganglion blocker 5% - 2 ml of pentamine.
8. For tachycardia, 0.025% solution of strophanthin - 1 ml with 10 ml of saline and 2.4% - 10 ml of aminophylline solution intravenously slowly.
After stopping the attack, the patient is transported to the intensive care unit in an elevated position (in case of collapse, in a horizontal position). If, when transferred to a horizontal position, the attack of suffocation does not resume, then the attack has been stopped.
Acute vascular insufficiency
- This is a violation of peripheral circulation, it is accompanied by low blood pressure and impaired blood supply to organs and tissues.
Etiology
:
O.S.N. can develop as a result of severe physical trauma, psychological shock, poisoning, overheating, blood loss, dehydration (vomiting, diarrhea). In this case, vascular tone is disturbed, the venous bed expands, low-venous blood enters the heart and arterial system, the heart cannot push enough blood into the arterial bed, and symptoms of bleeding of the brain and heart appear.
O.sos.week appears. Fainting, collapse, shock.
Fainting
(syncope) is a short-term loss of consciousness associated with cerebral ischemia. This is the lightest form of the vessel. weeks, can occur in people with a weak nervous system with extreme heat, stress, the sight of blood, with a change in body position, sudden standing up (orthostatic fainting) with severe illnesses, pleurisy, ascites (after removal of fluid from the abdominal or pleural cavity).
The development of fainting is preceded by a pre-syncope state, in which the patient experiences weakness, nausea, tinnitus, ringing in the head, darkening of the eyes, yawning, sweating, then the patient falls, loses consciousness,
the skin is pale and covered with cold sweat, breathing is shallow, slows down, the pulse is weak, the pupils are constricted, A/D is reduced. Lasts from a few seconds to several minutes.
There are 3 groups of syncope states:
Neurocardiogenic
(occurs from pain, the sight of blood, fear, in a stuffy room, a coughing fit, constipation, childbirth)
Cardiogenic
– obstructive and arrhythmic. Obstructive ones are caused by heart diseases (aortic stenosis, pulmonary stenosis). Arrhythmic - with bradycardia, paroxysmal tachycardia, flutter and ventricular fibrillation.
Angiogenic
fainting – orthostatic and cerebrovascular. Orthostatic - with quick standing, cerebrovascular - with damage to the cerebral arteries, osteochondrosis of the cervical spine.
It is necessary to differentiate fainting from epileptic and hysterical seizures, as well as hypoglycemia and cerebrovascular accidents.
Help for fainting:
- Call a doctor
- Lay the patient horizontally, without a pillow, elevate the legs (for blood flow to the brain). Unbutton tight clothing, provide a flow of fresh air, sprinkle the patient's face and chest with cold water, then rub with a towel, apply heating pads to the arms and legs.
- Give the swab moistened with ammonia (or vinegar) to sniff.
- Measure blood pressure.
- If there is no effect, as prescribed by the doctor,
administer 2 ml of cordiamine or 10% - 1 ml caffeine solution subcutaneously.
For bradyarrhythmic syncope, administer 1 ml of 0.1% atropine solution
For paroxysmal tachycardia, 5 ml - 10% solution of novocainamide intravenously slowly.
After restoration of consciousness, normalization of pulse, A/D, the patient is provided with physical and mental rest and observation, hot, strong, sweet tea.
Patients with fainting due to epilepsy, traumatic brain injury, or heart block are subject to hospitalization. If fainting occurs frequently, be examined by a doctor.
Collapse
– this is a manifestation of acute vascular insufficiency with a sharp and sustained decrease in blood pressure and circulatory disorders due to a decrease in BCC (circulating blood volume), a drop in vascular tone, and blood redistribution.
Etiology
:
due to large blood loss, with a sharp decrease in body temperature, for example, with lobar pneumonia, infectious diseases (food toxin infections, typhus, dysentery with vomiting, diarrhea, dehydration).
There are:
1) Hypoxemic collapse can occur when staying in an atmosphere with insufficient oxygen content.
2) Cardiogenic collapse (with myocardial infarction, myocarditis, pericarditis).
3) Vascular from decreased venous tone.
4) Hemorrhagic from acute massive blood loss.
Clinic
A characteristic feature of collapse is a sharp decrease in blood pressure. The patient experiences severe general weakness without loss of consciousness. The skin is pale, covered with cold sticky sweat, visible veins are collapsed, breathing is shallow, rapid, body temperature is reduced, the tongue is dry, the pulse is frequent, thread-like.
With collapse, consciousness is often preserved, but the patient becomes inhibited, indifferent to the environment, almost does not react to external stimuli, with blood loss, thirst, chilliness, coldness of the extremities, vision may decrease, and a “veil” may appear before the eyes.
On auscultation, heart sounds are muffled, frequent, sometimes arrhythmic, and oliguria is possible.
Urgent Care
- The nurse should call the doctor
- Create complete peace
- Horizontal position without pillow
- Warm the patient (cover with a blanket, heating pads to the limbs and lumbar region).
- Increase fresh air access and O2 supply.
Prepare and, as prescribed by the doctor, administer 2-3 ml of cordiamine subcutaneously or 2 ml of a 10% caffeine solution, or 2 ml of a 10% sulphocamphocaine solution to increase vascular tone (not administered for hemorrhagic collapse, useless if the bloodstream is empty, must be replenished O.Ts.K.).
If necessary, the injections are repeated. If there is no effect, 1 ml - 1% mesatone solution is administered (or 0.3 ml with 10 ml of isotonic NaCl solution - slowly intravenously, in the presence of a doctor.) In severe cases, 60-90 mg of prednisolone or 125 mg of hydrocortisone is administered intravenously from the main one.
Further treatment depends on the cause of the disease. Patients with collapse are hospitalized lying on a stretcher, accompanied by a doctor and a nurse (in the hospital they are transfused with the same type of blood, blood substitutes) and the underlying disease is treated.
- Prepare and, as prescribed by the doctor, administer 2-3 ml of cordiamine subcutaneously or 2 ml of a 10% caffeine solution, or 2 ml of a 10% sulphocamphocaine solution to increase vascular tone (not administered for hemorrhagic collapse, useless if the bloodstream is empty, must be replenished O.Ts.K.). If necessary, the injections are repeated. If there is no effect, 1 ml - 1% mesatone solution is administered (or 0.3 ml with 10 ml of isotonic NaCl solution - slowly intravenously, in the presence of a doctor.) In severe cases, 60-90 mg of prednisolone or 125 mg of hydrocortisone is administered intravenously from the main one. Further treatment depends on the cause of the disease. Patients with collapse are hospitalized lying on a stretcher, accompanied by a doctor and a nurse (in the hospital they are transfused with the same type of blood, blood substitutes) and the underlying disease is treated.
Shock
Shock
- this is a severe form of o. vascular insufficiency. This is a set of symptoms that characterize the severity of the patient’s condition, explained by a sharp deterioration in the blood supply to organs and tissues, impaired tissue respiration, the development of dystrophy, acidosis and tissue necrosis.
Shock develops as a result of the impact of extreme irritants on the body of both exogenous and endogenous origin. The most common hyocogenic factor is pain.
Depending on the cause, there are different types of shock:
1. Hypovolemic (with bleeding, with severe vomiting);
2. Cardiogenic (shock due to acute myocardial infarction, decompensated heart disease, cardiac tapmoponade);
3. Redistribution (anaphylactic, septic, toxic);
4. Obstructive (tension, pneumothorax, thromboembolism of the pulmonary artery trunk).
As well as painful, traumatic, electrotraumatic, post-hemotransfusion, septic, exotic shock.
Shock goes through 2 phases:
1 – erectile – excitement
2 – torpid – braking
According to the severity there are: mild, moderately severe, severe, preagonal stage, agony.
The clinic depends on the type of shock and severity.
Common symptoms of shock:
The patient is conscious (unconscious in the last stages). Complaints of general severe weakness, pain, chills, trembling, body temperature is sharply reduced, A/D is sharply reduced below 80/50 or is not determined. Facial features are pointed, pallor with an earthy tint, cold sticky sweat, thirst, dry mouth, tongue is dry and coated, pulse is weak, frequent, small or thready, visible neck veins are in a collapsed state, as well as symptoms of the disease that caused shock, the course of shock may be complicated impaired myocardial contractility, liver and kidney failure.
The prognosis depends on the type of shock, its severity, the time period for starting treatment, the presence of concomitant diseases and complications. If left untreated, shock is usually fatal. With cardiogenic, septic, mortality exceeds 50% even with early treatment.
General anti-shock measures
- General anti-shock measures
- Immediately call a doctor through the third person Eliminate the cause of shock if possible Check the airway and restore it In all cases of shock - inhalation of O 2 hydr. The following are carried out as prescribed by the doctor:
- Call a doctor immediately through your third person
- Eliminate the cause of shock if possible
- Check the patency of the airways and restore it. In all cases of shock - inhalation of O 2 hydrochloride.
- The following are carried out as prescribed by the doctor:
If there is no pulmonary edema, infusion solutions (saline and colloid) and vasopressors (poradrenaline, defalin) are administered.
For pain, use non-narcotic and narcotic analgesics or neuroleptanalgesia.
For pulmonary edema: oxygen through the defoamer antifomsilan or alcohol, as well as cardiac glycosides, aminophylline, depending on the A/D value.
In case of anaphylactic shock, adrenaline is administered at the site of subcutaneous injection and above subcutaneous injection, and the antichistaminics diphenhydramine, seprastin - intramuscularly, prezhinsolone intravenously.
For bronchospasm - intravenous aminophylline.
In case of cardiac arrest - urgent cardiopulmonary resuscitation.
- If there is no pulmonary edema, infusion solutions (saline and colloid) and vasopressors (poradrenaline, defalin) are administered. For pain, use non-narcotic and narcotic analgesics or neuroleptanalgesia. For pulmonary edema: oxygen through the defoamer antifomsilan or alcohol, as well as cardiac glycosides, aminophylline, depending on the A/D value. In case of anaphylactic shock, adrenaline is administered at the site of subcutaneous injection and above subcutaneous injection, and the antichistaminics diphenhydramine, seprastin - intramuscularly, prezhinsolone intravenously. For bronchospasm - intravenous aminophylline. In case of cardiac arrest - urgent cardiopulmonary resuscitation.
Be sure to be hospitalized in intensive care. Transportation on a stretcher. When transporting the patient, place the patient in a position that prevents retraction of the tongue and aspiration of vomit, cover with a blanket, cover with heating pads, give warm sweet tea in the absence of contraindications (gastrointestinal bleeding), reoxygenation, accompaniment and observation of a doctor and nurse to provide emergency assistance.
Diet for cardiac diseases
The patient must strictly follow the diet prescribed by the doctor. The diet should include sufficient quantities of foods rich in potassium and proteins:
- lean meat,
- vegetables,
- cereals,
- eggs,
- fish,
- greenery,
- high protein bread,
- potato,
- butter,
- cottage cheese.
It is recommended to eat 5-6 times a day in small portions. You need to have dinner no later than 2-3 hours before bedtime. Fluid intake should be limited by half, and salt should be replaced with spices, as it retains fluid in the body.
Physiotherapy
Caring for patients with cardiovascular diseases involves mandatory physical activity. The doctor selects a set of exercises individually depending on the patient’s health condition. The doctor will recommend special poses to relieve spasms, increase chest volume and relax muscles. Exercises should be performed at a slow pace, controlling breathing and smoothly changing positions. The sudden transition may cause shortness of breath or irregular heart rhythm.
It is recommended to start doing simple light exercises immediately after sleep, without getting out of bed. This is necessary to prepare the cardiovascular system for the climb. You need to train 3-4 times a day. The duration of classes is 10-25 minutes.
In addition to warming up for joints, the complex includes:
- balance exercises,
- training with a stick and ball,
- breathing practices.
In addition, daily walking for 30 minutes to 2 hours is necessary. Moderate aerobic exercise strengthens the heart muscle and blood vessels, normalizes blood pressure and metabolism.
Living conditions in boarding houses "Doverie"
Our specialists will provide patients suffering from various pathologies of the cardiovascular system with comprehensive care. Careful observation and timely assistance will prevent the development of acute conditions in our patients.
We accept elderly people with heart disease for rehabilitation, for example, we provide rehabilitation for patients with myocardial infarction, offer permanent residence, and also organize patronage. The Trust network of boarding houses for the elderly with rehabilitation has created comfortable conditions for cardiac patients. Our guests can count on:
- for medical care at any time of the day;
- regular observation by a doctor;
- dietary tasty food;
- comfortable rooms with functional furniture;
- favorable psychological environment;
- safe area for walking;
- a variety of pleasant leisure activities.
Friendly staff not only provide physical care for patients, but also help people with cardiovascular diseases quickly adapt to new living conditions and remain socially active even when lying down.
Relatives of our wards can visit them at a convenient time and always stay in touch via phone or instant messengers. We invite you to take a tour of any of our boarding houses so that you can personally see the conditions in which our guests live and communicate with our specialists. Leave a request on the website. Our manager will answer all your questions.
FIRST AID for acute heart failure
FIRST AID for acute heart failure
Acute heart failure (AHF) is a severe pathological condition that develops in patients with various heart diseases and hypertension. This is one of the most common reasons for calling an ambulance and hospitalization of patients, as well as mortality in our country and around the world.
The main manifestations (symptoms) of acute heart failure are:
- heavy, frequent (more than 24 per minute) noisy breathing - shortness of breath, sometimes reaching the level of suffocation, with predominant difficulty in inhaling and a clear increase in shortness of breath and cough in a horizontal position. A sitting position or a lying position with the head of the head raised up alleviates the patient's condition;
- Often when breathing, wet, squelching wheezing/sounds, interrupted by coughing, become audible; in the terminal stage, breathing takes on a bubbling character with the appearance of foam at the patient’s mouth;
- characteristic sitting position of the patient, resting his straight arms on his knees or on the seat (to facilitate breathing)
Acute heart failure can develop very quickly and lead to the death of the patient within 30-60 minutes. In most cases, 6-12 or more hours pass from the first clinical signs to severe manifestations of AHF, but without medical care, the vast majority of patients with AHF die.
Algorithm of emergency actions for acute heart failure (advice to the patient) - a reminder for the patient
When the above symptoms of AHF appear in patients with hypertension or heart disease (but not the lungs or bronchi), it is necessary:
- call an ambulance • give the patient a sitting position, preferably in a chair with armrests on which he can lean and engage the intercostal muscles in the act of breathing
- provide physical and psycho-emotional peace and fresh air by ventilating the room
- lower your feet into a large container (basin, tank, bucket, etc.) with hot water
- in extremely severe cases, tourniquets are applied to the legs in the groin area, compressing the superficial veins, but not the deep arteries, which reduces blood flow to the heart and thereby facilitates its work
If the patient or the person providing first aid has experience in the use of nitroglycerin, it is prescribed in a dose of 0.4 (0.5) mg (inhalation into the oral cavity is carried out under the root of the tongue, the tablet/capsule is placed under the tongue, the capsule must first be bitten, do not swallow). If the patient’s well-being improves after using nitroglycerin, it is reapplied every 10-15 minutes until the arrival of the emergency medical team. If there is no improvement in the patient’s well-being after the next dose of nitroglycerin, it is no longer used.
Attention! A patient with AHF must exclude all physical activity; it is strictly forbidden to walk, smoke, drink water and take liquid food until special permission from the doctor; Nitroglycerin should not be taken if blood pressure is less than 100 mm Hg. with severe headache, dizziness, acute impairment of vision, speech or coordination of movements.
All patients with hypertension or heart disease with shortness of breath and swelling in the legs should discuss with their doctor what medications should be taken if AHF develops, clearly write down their names, dosage and time sequence (algorithm) for taking them, and also check with the doctor for which manifestations of the disease, it is necessary to urgently call an ambulance. Each such patient needs to create an individual first aid kit for AHF and constantly have it with him.