Deficit of motor activity as one of the triggers of hypokinesia
Hypokinesia is a complex of disorders that includes decreased motor activity and slowness of movements.
Pathology usually develops with lesions of the central nervous system. For example, hypokinesia is observed in patients with Parkinson's disease. The effect of hypokinesia on the body:
- adaptive and compensatory reactions decrease;
- the functional and structural basis of movement changes (discoordination, joint stiffness);
- there is a pathological decrease in motor activity with a violation of statokinetic reflexes (maintaining balance);
- Energy and basal metabolism decreases, oxygen deficiency increases.
Why is hypokinesia harmful to our heart?
Decreased motor activity or hypokinesia has long been known for its side effects on our body.
What do we know about when we start to move less?
The modern world has advanced in the study of the genome and microstructures of cells, has looked beyond the invisible, but people still do not want to learn from their mistakes. Technologies designed to improve the quality of human life lead to the total destruction of his health. The paradox of what is happening is that progress in medicine prolongs the life of seriously ill patients, but at the same time does not have a strong impact on preventing the development of the diseases themselves. That is, every year a person becomes insensitive to discoveries in modern medicine, which indicate the possibility of preventing certain diseases.
We are blind to discoveries and possibilities of prevention, thinking that if the time comes, modern medicine will transplant any organ. This is the utopia of the modern technogenic world!
What can be changed? How to use modern knowledge for the benefit of humanity? Very simple! We need to act!
"A rolling stone gathers no moss!" - that's what our ancestors said. And they were right! "Movement is life!" - this is what modern medicine says. Experts from all areas of health care agree that physical activity prolongs life. It turns out that in order to live longer, you need to move!
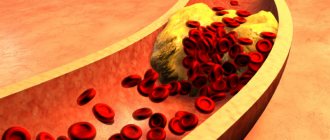
Modern medical statistics show disappointingly that the number of deaths from cardiovascular diseases is increasing every year. Having studied the reasons for this increase, scientists came to the conclusion that the main risk factors in the development of complications associated with diseases of the cardiovascular system are: physical inactivity, obesity, poor nutrition, arterial hypertension and atherosclerosis.
What do they have in common, you ask? And you will be immediately surprised! It all starts with a decrease in physical activity!
A long time ago, scientists noticed the fact that muscles play a very important role in the functioning of our body, providing it with more than just movement. Numerous muscles, and there are 600 of them, help the work of our heart. Contracting during physical activity, they turn into peripheral micropumps and push blood.
The first researchers of the cardiovascular system believed that in addition to the heart, “peripheral arterial hearts” function in humans. These little motors that help push blood through. But over time and the development of medicine, this hypothesis was refuted. Although the idea itself allowed us to delve deeper into the study of the mechanisms of influence of muscle contractility on the cardiovascular system.
And what do you think? What did scientists discover?
They discovered that the working muscle turns into a powerful pump, capable of pushing blood with the same pressure as in the aorta. Unique experiments on connecting an isolated muscle to the vascular system confirmed the fact that a muscle working on its own can perform a function similar to that of the heart. From here, doctors came to the conclusion that working muscles in the periphery are assistants to our heart.
It turns out that the more we move, the easier it is for our heart to pump blood. The same observations were noted in patients with heart failure. They were recommended a special regimen of physical activity aimed at relieving the “tired heart.” The results were stunning. Heart failure patients who exercised had fewer complications than patients who did not exercise. This gave scientists the idea to develop a special set of physical activity for patients with cardiovascular diseases. And today these techniques have actively entered the system of rehabilitation of cardiac patients.
So what happens? If movement is necessary for people with diseases, then did God himself command it for healthy people?
This is true! Let's list together what happens when muscles move and contract.
- Muscles contract, which means they pump more blood and faster. This means more oxygen enters organs and tissues.
- Muscle contraction makes the heart work easier. This means the reserve of the heart muscle increases.
- Muscle tension requires energy. This means that excess glucose is consumed and insulin resistance decreases. Here's the prevention of diabetes.
- Static muscle load requires a large amount of calories. This means we burn excess fat deposits, including the most insidious – visceral.
- Constant muscle activity regulates hormonal levels, especially in men.
- Good muscle tone is the basis for healthy posture, normal functioning of the gastrointestinal tract, and pelvic organs.
Before you give up physical activity again, think about your hard worker, your heart! Is it worth throwing away what nature has given us?
previous article
Jerzy Starak awarded by GMU
next article
Intestinal colic and correction of microbial colonization in children in the first months of
life
Causes of hypokinesia
The most common causes of pathology are dysfunction of the basal ganglia and a decrease in excitation processes in the motor cortex. Hypokinesia can also be caused by a lack of motor activity - for example, with prolonged immobilization due to injuries or serious illnesses. A decrease in motor activity is also observed in some mental disorders.
Causes of hypokinesia:
- degenerative disorders;
- taking certain medications;
- vascular disorders;
- injuries;
- intoxication;
- CNS infections;
- metabolic disorders;
- neuromuscular disorders.
Hypokinesia of the gallbladder occurs due to a decrease in its motor-evacuation function. If the gallbladder contracts insufficiently, less bile enters the digestive tract. Patients complain of dull pain in the right hypochondrium without clear irradiation. You can learn more about biliary dyskinesia by consulting a doctor - you can make an appointment on our website.
PROGNOSIS, COMPLICATIONS, TREATMENT AND PREVENTION OF RECURRENCE
The prognosis for systemic (diffuse) myocarditis is favorable in more than 50% of cases. Especially if myocarditis discovered itself at the (sub)acute stage. The exception is diffuse idiopathic myocarditis, which is often accompanied by complications.
The latter may include:
- cardiogenic shock;
- thromboembolism;
- myocardiosclerosis;
- DCM (diffuse myocarditis can cause stretching of the cardiac cavities).
The most common complication of myocarditis remains diabetes.
How long will the treatment take?
The treatment regimen for myocarditis includes three mandatory points.
- Elimination of signs and risks of diabetes (mainly reduced to drug treatment of myocarditis with diuretics, ACE inhibitors and glycosides).
- Elimination of the platform for the development of diffuse myocarditis (protozoal infection, virus, fungal infection, bacterial attack).
- Stimulating therapy (here - antiallergic support for diffuse myocarditis).
For idiopathic acute and subacute diffuse myocarditis, antibiotics, antihistamines and NSAIDs are often recommended. Hospital stay (strict physical inactivity, hemodynamic monitoring, vitamin supplementation) will take up to a month. Full recovery – in a year (or longer).
Since the diffuse form is characterized by extremely severe myocarditis, the person remains registered with cardiology for at least a year after remission. You can go for sanitary resort treatment no earlier than after 10-12 months.
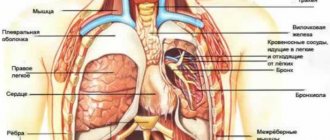
Hypokinesia of the ventricles of the heart
A decrease in the amplitude of movement of the left ventricle is also classified as hypokinesia. Zones of hypokinesia during echocardiography indicate either acute or previous myocardial infarction (post-infarction cardiosclerosis), myocardial ischemia, and thickening of the myocardial walls. Disorders of local contractility of left ventricular segments in patients with coronary heart disease are assessed on a five-point scale:
- Normal contractility.
- Moderate hypokinesia.
- Severe hypokinesia.
- Akinesia (lack of movement).
- Dyskinesia (a segment of the myocardium does not move in the desired direction, but in the opposite direction).
Right ventricular hypokinesia is detected in patients with acute pulmonary embolism (PE). Studies have shown that the presence of right ventricular hypokinesia in patients with acute PE doubles the risk of mortality within the next month. This fact allows us to identify high-risk patients who appear stable.
What cardiac abnormalities are visible through echocardiography?
1. Why can’t ultrasound of the heart be done using a conventional ultrasound machine?
It is possible, but the result of the research will be incomplete. The fact is that an echocardiograph has additional capabilities and special sensors that allow you to obtain a high-quality image of an organ that is constantly in motion. In addition, any device is capable of conducting research with the Doppler effect. Dopplerography makes it possible to evaluate the speed of blood flow, its direction, and the presence of pathological discharge. This is fundamentally important when assessing the condition of the heart valves and septa located between the atria and ventricles. Finally, a special transesophageal echocardiography probe, which looks more like a gastroscope, can be connected to the echocardiograph.
2. They say that echocardiography is the gold standard in the final diagnosis of a heart attack?
In fact, it is EchoCG that puts an end to the question of whether there was a myocardial infarction or not. This opportunity is provided by a targeted study of the walls of the heart - anterior, lateral, posterior or inferior, as well as the interventricular septum. If the myocardium in these areas has received necrotic damage and a scar has formed there, echocardiography will reveal a violation of its contractility. This means that the wall contracts worse, lags behind those located nearby (hypokinesia), contracts in its own way, as they say, without hitting the leg (dyskinesia), or will not contract at all, getting out of the general march (akinesia). If such changes are detected (and they are often an accidental finding, without indicating a previous heart attack), then the probability of a heart attack in the past is more than 90%. If the diagnosis is a heart attack, but ECG and EchoCG data cannot confirm this, most likely we are talking about overdiagnosis and the heart attack did not actually occur.
3. What EchoCG indicators can be called the most important?
The strength of the heart muscle is shown by the so-called ejection fraction (EF). If this indicator is reduced, we may be talking about chronic heart failure. The presence of disturbances in local contractility of the myocardium of the heart walls (hypokinesia, dysikinesia, akinesia) indicates a previous infarction or ischemia. Valve assessment includes the number of leaflets, the size of the opening, and Dopplerography determines the presence of reverse blood discharge (valve insufficiency) or an increased pressure gradient across the valve, indicating the formation of narrowing (stenosis) of the valve. Valve insufficiency or regurgitation is measured in degrees: from first to fourth. If the first and second can be classified as a variant of the norm, then the third (pronounced), and even more so the fourth, is considered a pathology that requires surgical correction. Analysis of the heart septa helps to identify the presence of pathological holes and blood discharge through them (atrial and ventricular septal defects). Important information is provided by the size of the heart chambers, the thickness of the myocardium and the presence of its hypertrophy, and blood clots in the heart cavity.
4. What is stress - EchoCG?
If a patient is suspected of having coronary heart disease, a stress test is prescribed. Often this is bicycle ergometry or treadmill, when the patient pedals a bicycle or walks on a treadmill, and his ECG is constantly recorded, waiting for ischemia to appear. But before the appearance of changes on the ECG, the same changes in the kinetics of the walls that we have already discussed appear. Moreover, you can immediately accurately detect the wall of the heart that suffers the most, and guess which artery is narrowed by plaques. Therefore, a stress test with echocardiography is considered more informative. It is carried out through physical activity, when the patient pedals a special bicycle in a supine position, or by stimulating the heart by injecting special medications into a vein. As a result, the heart works much more actively, and fragments of the myocardium experiencing a lack of nutrition contract worse than others.
5. Why is transesophageal echocardiography prescribed?
In some cases, even after performing a standard EchoCG, cardiologists require clarification. What could not be seen through the chest using a conventional probe can be seen from the esophagus using a probe that is more reminiscent of a gastroscope. It turns out that from the inside it is better to see heart valve defects, the condition of its septa and the presence of blood clots in the atria. The study is carried out in consciousness under the influence of mild sleeping pills; the sensations cannot be called pleasant, but it is also too uncomfortable, but it resembles a regular gastroscopy.
6. How to prepare for EchoCG?
A regular examination, called transthoracic, does not require special preparation. If we are talking about a transesophageal examination, then you will first need to perform a gastroscopy to make sure that there are no erosions, varicose veins or other disorders in the esophagus. If during the study it turns out that a person has difficulty tolerating the insertion of a “hose” into the upper gastrointestinal tract, transesophageal echocardiography can be performed under intravenous anesthesia, as patients say “in their sleep.”
Today, echocardiography, like all studies, is actively developing. Now it is done not only from the esophagus, but also directly from the heart cavity - the so-called intracardiac echocardiography. To do this, the sensor is brought to the heart from the inguinal vessels. The results of the study are presented in the form of three-dimensional moving images of such quality that it is difficult for the doctor to distinguish the reconstruction from the real beating heart.