Human blood consists of two components. The first is fluid plasma rich in proteins. The second is formed cells, among which platelets stand apart. These red plates ensure normal coagulation and help the body cope with mechanical damage.
PDW in a blood test is an indicator of platelet heterogeneity; in other words, it demonstrates which cell forms predominate: young and functionally active, or old and practically unsuitable for solving physiological problems.
Normally, the blood contains both, but they must be in dynamic balance. Mostly in the mainstream of a healthy person, young, ready-to-work forms are found. The abbreviation PDW stands for relative platelet distribution width across the blood volume.
Deviations in the study do not always mean a pathological process. It often turns out that we are talking about a functional version of the norm.
The issue is complex and requires discussion with a hematologist. It is possible to say anything concrete only after a group of analyses. The data is decrypted in the system.
There is also not always a need for treatment. Changes in PDW are not an independent diagnosis, but rather a laboratory indicator. You need to fight the underlying disease.
The essence of the analysis and what it shows
To understand what we are talking about, you need to turn to human anatomy and physiology.
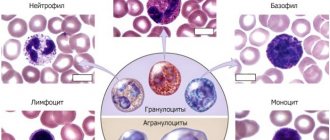
Platelets are special shaped blood cells. They ensure its normal coagulation.
The development of cytological structures occurs in special tissues of the bone marrow. This process is called hematopoiesis, and if we talk about platelets in isolation, then thrombocytopoiesis.
Platelets perform their functions for quite a long time. Within 5-12 days. Then they die, and new ones come to replace them.
But this is not a quick phenomenon. Over the course of a short period of time, a shaped cell goes through all stages of life from youth to old age.
After maturation and immediately after leaving the bone marrow, the structure is large. The blood plate is capable of performing its tasks as efficiently as possible.
It takes less time and not as many platelets to close the wound surface. Moreover, adhesion and aggregation occur faster. That is, attachment to the wall of the vessel and accumulation, layering.
Old cells are no longer as active. More of them are needed, and the natural processes themselves proceed slowly and not as well as before. Hence the problems.
Accordingly, if there are more obsolete cytological units, then coagulability will suffer. Its intensity will not be so great that it will be reflected in the coagulogram.
The platelet distribution index or PDW precisely indicates the heterogeneity of cells: that is, the percentage of red plates distributed.
Normally they should be in dynamic equilibrium. Numbers from 1 to 20% are used as values. When young forms of cytological structures predominate, the formula shifts to the right. That is, in a big way. In the opposite case, when there are a lot of old cells, the opposite is true. The number will be lower.
The conditional generalized norm is approximately 15-17%. That is, young forms of platelets should predominate in the bloodstream. This is an indispensable condition for normal coagulation and functioning of the body. Of course, there are differences depending on the gender and age of the patients.
The analysis shows several main violations:
- Thrombocytopathies. A classic pathological process in which the functional activity of red blood platelets decreases. Formally, their number remains normal. This is where the index in question comes to the rescue.
Because the reason is often on the surface and lies in a change in the platelet ratio. The more old cells there are, the worse the body’s functioning is. In critical cases, obsolete structures remain.
- Thrombocytopenia. Different condition. With it, not only the PDW index changes, but also other indicators. The hallmark of the pathological process is a decrease in the number of platelets. It all depends on the primary diagnosis.
- Bone marrow disorders. It’s quite difficult to say exactly which ones. As a rule, with disorders of this kind, the previous named pathologies develop. At the same time, immature hematopoietic cells appear in the bloodstream. Megakaryocytes. They are unable to perform any functions. In this case, it makes sense to conduct a diagnosis. A bone marrow puncture is prescribed.
A blood test for PDW is far from the only necessary test. To tell exactly what is wrong with the patient, auxiliary measures are needed.
Preventive actions
Anyone can maintain blood counts at the proper level - it is not difficult. Initially, we should not forget that the main aspect of normal well-being for absolutely all people is a healthy lifestyle. If you follow a few simple rules every day, the body, regardless of age, will delight with its excellent performance not only of the circulatory system, but also of all other functional systems.
So, preventive measures aimed at maintaining normal PDW are as follows. Throughout the day, adhere to the correct drinking regime. After all, more than 90% of blood consists of plasma, and it, in turn, is renewed and has the ability to circulate only if clean drinking water continuously enters the human body.
It is necessary to eat a balanced diet, and make up your diet exclusively from high-quality products that contain sufficient amounts of minerals, vitamins and other useful substances. Take regular walks or bike rides. You can simply walk in the fresh air for at least 2 hours in places where there are many trees: in squares, parks, forest belts, etc.
Try to avoid stressful conditions and other psycho-emotional disturbances of a negative nature. Physical activity should be non-intense, that is, you should not overwork yourself, and after overexertion you need to recover well. You should not take any medications without first consulting your doctor, as this may cause side effects that may adversely affect your health.
The conditions necessary to maintain health are actually quite simple and easy to implement. But at the same time they have enormous benefits for all functional systems of the human body. That is why, simply by simply adhering to them, you can prevent the development of dangerous violations in its activities.
A healthy lifestyle will help keep your body healthy until old age.
Indications for the study
There are quite a lot of reasons for diagnosis. In more detail:
- Bone marrow disorders. Myeloproliferative diseases and conditions in which the maturation of formed cells is disrupted. Not only platelets, but also red white blood cells. Also other bone marrow disorders. Up to blood cancer.
Unfortunately, the analysis is too general to show specific changes. Deviations by PDW are merely indications of a violation. But it is by no means an exhaustive diagnostic method. A bone marrow puncture and other tests will be required.
- Previously diagnosed thrombocytopathy. A condition in which the functional activity of blood cells decreases, but their number remains at a normal level. Happens quite often. It practically never happens to be primary. As a rule, the disorder is caused by other pathological processes.
- Cancer diseases. Regardless of type, stage and location. The platelet distribution index (PDW) may well be a nonspecific marker of the oncological process.
The reason for this is bone marrow dysfunction. It can no longer function in “normal” mode. Consequently, cell maturation slows down. Precursors and old forms of platelets circulate in the bloodstream. This is a fairly typical clinical picture of cancer.
- Preparing for hospitalization. The study of the platelet distribution index is included in the mandatory list. Especially if doctors are planning surgical treatment or invasive procedures. The decrease clearly speaks in favor of coagulopathies.
Attention:
Coagulation disorders are a contraindication for surgical treatment.
- Therapy control. The study of the platelet distribution index is also practiced as part of dynamic observation, when specialists assess the patient’s health status after therapy. This is necessary, for example, in the treatment of megaloblastic, iron deficiency anemia and other pathological processes.
- Preventive examinations. Semiannually. Typically, PDW testing is performed as part of a routine blood test. Therefore, the patient does not have to break down and run for additional research.
The list of indications is approximate. The doctor, at his own discretion and discretion, prescribes the study. If there is a reason for it.
Normal indicators
In people who do not have problems with clotting, regardless of age, the majority of platelets in the bloodstream should be kept in a mature form, because it is at this stage that they are able to fulfill their main purpose - to carry out normal activities aimed at blood clotting. The permissible deviation in the quantitative indicator of mature platelets should not exceed 10%, both in the direction of decrease and increase.
Excessive excess of normal parameters means a high probability of the formation of blood clots, which lead to blockage of blood vessels and then to the development of various pathological processes. And too low platelet counts are a direct path to heavy blood loss, which is no less dangerous for human life and health.
The normal PDW in children under 18 years of age who do not have diseases associated with blood clotting is 10–15%. In adults, this index should not leave the range of 15–17%. Significant deviations from generally accepted parameters in almost all situations are observed as a result of functional disorders of a particular organ or system that require immediate medical attention.
Reasons for the increase
An increase in the platelet distribution index is indicated in cases where the number of young structures prevails over the concentration of old cells. If we talk about the condition, there may be several culprit factors.
Megaloblastic anemia
In this case, the concentration of healthy platelets increases only at the very beginning of the disease. When the body is still able to produce normal formed cells. This is a kind of reflex response to the body’s need for a sufficient number of cytological units.
As vitamin B12 or folic acid deficiency worsens, immature progenitor cells are released into the bloodstream. The so-called megaloblasts. They replace both platelets and red blood cells.
Without treatment, the disease poses a threat of death to the patient. Correction is carried out with loading doses of B vitamins.
At the same time, it is important to cope with the primary pathological process. For example, if the reason for everything is insufficient absorption of substances in the digestive tract. For ulcers, colitis and other disorders.
Without etiotropic therapy there is little point in fighting. Read more about the mechanisms of development, causes and treatment of megaloblastic anemia in this article.
Iron-deficiency anemia
It works in the same way. Micro and macroelements are necessary for normal functioning of the body and cell maturation.
If there is a deficiency of both the first and second, first a stress response occurs, such as excessive cell synthesis, then the process goes to the opposite extreme. The same applies to this case.
Treatment. Iron deficiency anemia requires taking iron supplements. Parenterally, bypassing the digestive tract.
Often the disease develops against the background of colitis, gastritis and other inflammatory processes. The gastrointestinal tract needs to be treated in order to normalize or accelerate the absorption of iron.
Cancer (not always)
Typically, cancer can manifest itself in two ways.
- The first concerns the increase in PDW in the blood test. Typically, an increase in the indicator, which means an increase in the number of formed cells, is possible only at the initial stage of the disorder. Then everything happens exactly the opposite.
- At the extreme stages of the pathological process, the growth of magekaryocytes begins. Predecessors. This is the body's attempt to compensate for the lack of healthy cells.
Treatment. Depends on the stage of cancer, its type and location. As a rule, they start with surgical correction. Remove the modified tumor as much as possible.
Then radiation and chemotherapy are prescribed. Not always though. Depends on the sensitivity of the tissue to this effect.
Infectious diseases
The relative width of platelet distribution by volume increases during an inflammatory process of infectious origin: infection with bacteria, viruses, fungi.
Increased cell synthesis begins. Platelets also mature. Red blood platelets are indirectly involved in the immune response and the functioning of defenses.
The distribution index of formed cells is close to 20%. With a prolonged course of the pathology, weakening of the body, the concentration decreases. Which is immediately reflected in PDW.
Treatment. Calibrated doses of antibiotics, anti-inflammatory drugs. Non-hormonal, since glucocorticoids inhibit the functioning of the defenses.
Autoimmune diseases
They cause a reflex release of additional cells. Including from the spleen, which acts as a kind of depot, a repository of shaped structures.
It doesn't matter much. However, in a blood test, a deviation in the index can be considered an indication of an autoimmune process.
Treatment. Glucocorticoids in adequate doses. If ineffective, high concentrations of the substance are prescribed. The drugs used are Prednisolone, Dexamethasone and more powerful analogues as needed.
If there is no effect, cytostatic agents are used. In small doses and strictly short courses.
Prevention
In order to normalize the PDW indicator, you should use recommendations for improving the quantitative and qualitative composition of blood :
- adhere to a proper balanced diet, rich in vitamins and beneficial microelements that can affect blood quality;
- avoid physical overexertion (especially typical for athletes);
- limit uncontrolled use of medications;
- maintain a hydrated diet, drinking at least 2 liters of clean water per day;
- limit consumption of sweet foods and carbonated drinks.
Thus, a blood test indicator such as PDW allows one to determine the width of platelet distribution by volume. This indicator depends on many factors, indicating possible health problems, namely with hematopoietic functions. In order for the test result to reflect a reliable picture of your health status, you need to take it on an empty stomach and in a good mood. The presence of menstruation and psychomotor disorders can significantly affect the results of the study, giving false indicators. Only an experienced specialist is able to interpret PDW indicators, comparing them with the norm, and also insist on undergoing a more detailed examination.
We recommend reading all the information about elevated platelets in the blood of men. We tell you how to reduce platelets in the blood. We find out the reasons for the increased ratio of large platelets. What to do if platelets are elevated during pregnancy? Share:
Reasons for falsely high results
Among them:
- Wrong analysis.
- Violations of sample processing techniques.
Sometimes the patient himself may be to blame. Many factors influence the final result.
Deviation occurs in the following cases:
- Intense physical activity. Approximately a day before taking the test, you should not practice excessive mechanical activity.
- Smoking. It is abandoned a few days before the study.
- Eating. Food should be avoided 3-4 hours before blood sampling. This way the results will be more accurate.
- It is not advisable to take the test during menstruation, pregnancy and breastfeeding. Because the results will definitely be false. Possibly within the margin of error.
- You should also not drink alcohol, overheat or become hypothermic. In about 1-2 days. Deviations within small values are possible. If other analysis indicators are normal, such errors are not paid attention to.
When the platelet distribution index is increased, this means that the number of young cells is greater than the number of old, waste structures. As a rule, blood diseases are to blame.
It often turns out that there is no pathological process and the deviation is due to the actions of the patient. Smoking, leading an unhealthy lifestyle.
How to prepare for the procedure
Very often, patients ignore the specialist’s recommendations for preparing for blood sampling, but the result of the laboratory test depends on this. In case of uncharacteristic changes in PDW, one should not discount the fact that it was incorrect preparation for the analysis that led to this result.
How to properly prepare for the procedure?
- 24 hours before the procedure, avoid absolutely all physical activity. This is due to the fact that during sports the body requires more oxygen consumption, which leads to an increase in platelets in the blood.
- Before taking blood, you should sit quietly for 20 minutes and calm down.
- It is necessary to take the test on an empty stomach. And also, at least 24 hours in advance, give up everything spicy, salty and peppery. This is due to the fact that such products enhance liver function, which leads to false test results.
- It is forbidden to drink coffee on the day of the test itself.
- Alcoholic beverages should not be consumed at least three days before the scheduled event.
- The test results are affected by the use of synthetic hormones, so you should take a break from taking medications. If this is not possible, then you must notify your doctor.
If there are deviations in the results of the laboratory test, the specialist is obliged to reschedule the procedure. This will help to accurately determine the reason for the change in indicators. If during a complete examination of the patient no abnormalities in health are noted, then monitoring of PDW is necessary; it is possible that its decrease is a temporary phenomenon of unknown origin. In any case, a diagnosis can only be made after receiving repeated results from blood tests and other procedures.
Reasons for the decline
If the width of platelet distribution is below normal, this means that the volume of old, unfit for work cells in the blood is greater than that of young, functionally active cells.
The percentage drops in several cases.
Megaloblastic anemia
As mentioned earlier, the concentration of young cells increases only at an early stage. Plus, medical errors are possible when megaloblasts, the precursors of mature structures, are perceived incorrectly.
In the later stages of the disorder, the opposite is true. Only old cells remain. The formula on the PDW chart shifts to the left, downward.
Therapy consists of using loading doses of vitamins B9 and B12.
Liver diseases
Pathologies such as hepatitis - an inflammatory process or cirrhosis of the organ.
The largest gland is indirectly involved in platelet maturation. When a disorder begins, the number of healthy formed cells drops sharply and is restored only when the organ returns to normal.
Treatment is standard. Hepatoprotectors are used: Essentiale, Karsil. In case of subcompensated cirrhosis, transplantation is required. This is the only method of radical correction.
Cancer
The same applies to oncology. Platelet counts change as the tumor progresses.
The process forces the bone marrow to work at its maximum capacity. At a certain point, the organ is no longer able to function as it should.
Treatment is surgery, chemotherapy and radiation therapy.
Taking certain medications
From the point of view of the maturation of platelets, red and white blood cells, medications such as glucocorticoids and cytostatics are especially dangerous. The first and second inhibit the functioning of the body's defenses. This is extremely dangerous. Immunosuppressants pose a particularly great threat.
The treatment is simple. It is enough to refuse a specific medication. On the other hand, you can replace it with a safer analogue.
Attention:
The same applies to non-steroidal anti-inflammatory drugs and antibiotics. At the end, you need to stimulate bone marrow function.
Blood loss
Hypovolemia. In this case, the number of mature cells and old, functionally incompetent platelets decreases. But not proportionally.
As a rule, trauma is to blame. Consequently, young platelets will undergo adhesion and aggregation, and old ones will remain in place, but the formal number of functional red platelets will be lower. This is a temporary phenomenon.
Treatment. Transfusion of blood and its formed elements.
Pregnancy
Of course, it is not considered a disease. The number of young cells does not always decrease during gestation. But this is possible, especially when bearing several fruits. Changes in PDW values are temporary. No special treatment is required.
If the width of the platelet distribution by volume is reduced, the cause is diseases of the internal organs or blood loss, but medications or natural conditions such as pregnancy are often to blame.
Decoding
Many people ask what PDW is in a blood test and who interprets the test. The doctor must decipher the PDW blood test. PDW may be normal, elevated, or decreased. A normal index occurs when the number of old and young cells is the same. This index occurs in healthy people. If the indicator is elevated, then their number has sharply increased, and a large number of young and old cells are contained. This happens with bone marrow pathologies or other diseases.
An increased value of the indicator is determined in cancer, iron deficiency, and inflammatory processes. This result occurs with infectious diseases or when the patient uses hormonal drugs. A decreased PDW indicates that there are more old particles, which may indicate bone marrow disease, viral diseases, or certain medications.
When doctors decipher the result, sometimes the study shows that a person has too large platelets, which indicates the presence of disturbances in the functioning of the immune system or Bernard-Soulier disease.
Norm
The normal PDW in adults is 15-17%. The breadth of platelet population distribution in children under 18 years of age is 10-15%. If there is a deviation from the norm, the doctor considers the possibility of dysfunction of organs or systems. This indicates some kind of disease.
Increased level
An increase in the indicator indicates heterogeneity in platelet volume. This can cause the development of pathologies in the body. In patients, blood vessels gradually become clogged, blood circulation is disrupted, and metabolism slows down. Heart disease gradually develops.
An increase in PDW occurs:
- For anemia. The process causes oxygen starvation, which contributes to a change in cell volume.
- For bleeding after surgery.
- With the development of neoplasms and inflammatory processes.
- If, in addition to an increase in PDW, an increased number of leukocytes is noted, then the doctor diagnoses inflammation.
Additional examinations
Supportive measures allow us to establish the correct diagnosis:
- Oral interview with a hematologist.
- Anamnesis collection.
- Bone marrow puncture. It is prescribed to clarify the nature of the pathology.
- Assessment of the size of the spleen, ultrasound of the digestive tract. At the same time, the liver is examined.
- Biochemistry of blood.
- MRI or CT as needed. With contrast enhancement with gadolinium and iodine, respectively.
The question of what caused the index to rise or fall is complex. The doctors decide. Treatment is carried out as needed. It is mainly etiotropic, that is, aimed at correcting the underlying cause. Primary disease.
Treatment
To treat, you need to know what to treat. Therefore, treatment is not prescribed until a final diagnosis is made. After diagnosing the root cause, drug therapy is aimed at eliminating it as much as possible.
The presence of cancer and problems with hematopoietic function is eliminated by transplanting spinal cord cells, as well as undergoing a course of chemotherapy.
Thrombocytosis
Pathogenetic groups | Clinical forms, situations |
| Primary | Myeloproliferative diseases: chronic myeloid leukemia, myelofibrosis, erythremia. |
| Secondary: 1. Reactive | |
| - for malignant tumors | carcinoma, lymphoma, lymphogranulomatosis |
| - for inflammatory diseases | acute rheumatism, rheumatoid arthritis, ulcerative colitis, tuberculosis, osteomyelitis |
| - for acute anemia | acute posthemorrhagic, acute hemolytic anemia |
| — after operations | within 2 weeks |
| 2. After splenectomy. | within 2 months |
How is the analysis carried out?
The PDW value is determined during a general blood test along with many other indicators. Blood is taken from the (ring) finger on an empty stomach in the morning. Whole blood with an anticoagulant is used for the study.
The result may be unreliable if the patient ate food before the analysis, is being treated with medications during this period of time, or underwent an X-ray examination or physical procedures the day before. In addition, the indicator may be higher or lower than normal during pregnancy, before menstruation, or after heavy mental or physical stress. In such cases, a repeat study is prescribed. To avoid distortion of the results, you should properly prepare for the analysis.
Nowadays, modern hematological analyzers are used for blood testing, which obtain up to 24 indicators. Determining platelet volume alone is not sufficient for effective diagnosis. Normal hemostasis depends not only on the quantitative content of nuclear-free plates, but also on their functional indicators. Therefore, it is so important to study their quality characteristics, which is only possible on new equipment. Hardware methods for studying blood elements have many advantages over manual ones:
- a large number of cells are examined - from 10,000;
- provide accurate results - without errors;
- all stages of the study are standardized.
With the help of modern blood analyzers, histograms are obtained - a graphical representation of the results in the form of thrombocytometric curves. The importance of this study is due to the fact that the size of platelets determines their functionality, the change in their volume before gluing the plates in the process of clot formation, as well as the tendency to adhesion and the content of bioactive substances in anucleate cells.
Hardware blood testing methods allow you to get accurate results in a shorter time
If there are predominantly young platelets in the blood, the histogram is shifted to the right, old platelets are located on the left of the graph. Thus, platelet volume decreases as platelet aging occurs.
Recommendations for taking the test
There is no need to prepare extensively to take the pdw test. It is recommended to donate blood on an empty stomach in the morning so that there is no reason for false results. If a person is taking medications, the specialist must be informed about this before taking blood. This blood test will be ready very quickly.
Usually blood is taken from a finger, but if additional information is required for research, then venous blood is needed, which contains a larger number of indicators that are needed for a more accurate analysis. If any of the components deviates from the norm, then the analysis from venous blood will be more informative and there is no need to repeat the test.
Blood sampling from children on pdw is carried out from a finger, as this is more comfortable for the child and more convenient for the nurse.
The material is sent to the laboratory for testing and preparation of results. It takes two days to complete all these actions.
In addition, different laboratories have different equipment and different reagents, so two laboratories may produce completely different results in terms of accuracy.
Thrombocytopenia
Thrombocytopenia groups | Clinical forms, situations |
| I. Decreased platelet production (hematopoietic insufficiency) | |
| 1. Purchased: | |
| - idiopathic | idiopathic hypoplasia of hematopoiesis |
| - after viral infections | viral hepatitis, adenoviruses |
| - due to intoxication: | |
| a) exogenous | chemicals (benzene, insecticides), antibiotics (chloramphenicol, streptomycin), alcohol, ionizing radiation |
| b) endogenous | uremia, severe liver disease |
| - infectious-toxic | viral or bacterial sepsis, miliary tuberculosis, rickettsiosis, toxoplasmosis |
| - for tumor diseases | acute leukemia, myelodysplastic syndrome, myelofibrosis and osteomyelosclerosis, metastases of carcinoma and sarcoma to the bone marrow |
| - for megaloblastic anemia | B12 and folate deficiency anemia. |
| - with nocturnal paroxysmal hemoglobinuria | |
| 2. Hereditary: | Fanconi syndrome, Wiskott-Aldrich syndrome, May-Heglin anomaly, Bernard-Soulier syndrome |
| II. Increased platelet destruction | |
| 1. Immune: | |
| - autoimmune | |
| a) primary | idiopathic thrombocytopenic purpura |
| b) secondary | for systemic lupus erythematosus, chronic active hepatitis, chronic lymphocytic leukemia, etc. |
| - isoimmune | in newborns (penetration of maternal antibodies), post-transfusion |
| - heteroimmune (haptenic) | |
| a) medicinal | hypersensitivity to drugs |
| b) viral | hypersensitivity to viruses |
| 2. Destruction in the spleen | hypersplenism in histiocytosis, storage diseases, lymphomas, hairy cell leukemia, splenic tuberculosis, myeloproliferative diseases, portal hypertension |
| 3. Platelet consumption | disseminated intravascular coagulation |
Possible reasons for deviation from the norm
Elevated parameters may indicate the following pathological processes:
- inflammation in the body;
- cardiovascular diseases;
- liver diseases;
- oncological processes, metastasis to the bone marrow;
- anemic syndrome;
- heavy metal poisoning;
- Alzheimer's disease.
The index will be increased due to the following factors:
- consequences of corticosteroid therapy;
- massive blood loss;
- postoperative period after removal of the spleen;
- excessive physical activity;
- recovery after surgery.
Reduced index values will indicate the following pathological processes:
- DIC syndrome;
- anemia;
- myelodysplastic syndrome;
- viral diseases;
- septic processes;
- radiation sickness;
- severe liver diseases.
PDW can be lowered temporarily as a result of taking certain medications, including cytostatics.
Mean platelet volume (MPV - mean platelet volume)
Expressed in femtoliters or µm3. Normally, this figure varies from 7.4 to 10.4 fl and tends to increase with age. “Young” blood platelets have a larger volume, so as thrombocytopoiesis accelerates, the average platelet volume increases.
An increase in MPV is observed when:
- idiopathic thrombocytopenic purpura
- hyperthyroidism
- atherosclerosis
- diabetes mellitus
- in smokers and alcoholics
- myeloproliferative diseases
A decrease in MPV is observed after splenectomy and in Wiskott-Aldrich syndrome.
Who to contact
First of all, you should contact a general practitioner - therapist. Next, a consultation with a hematologist will be required; an oncologist, a neurologist, a medical geneticist, an allergist, a cardiologist, and an infectious disease specialist may additionally be involved.
Further measures will depend on the clinical picture, general condition of the patient and family history, since congenital blood diseases cannot be excluded, which will affect the platelet distribution index.
Main publication
- Platelets
Table of contents:
What can cause a low blood count?
If PDW platelet distribution is reduced, then most likely the cause of this condition is:
- blood oncology;
- illness due to increased exposure to radiation;
- myelodysplastic syndrome;
- DIC (disseminated intravascular coagulation);
- diseases caused by viruses;
- sepsis;
- taking cytostatics;
- iron deficiency;
- liver problems.
Myelodysplastic syndrome is often diagnosed in patients with reduced PDW. This disease affects the bone marrow, where platelets are formed. In addition, with metastases in bone marrow cells, the rate will also be low.
Hepatitis can provoke a decrease in PDW. To confirm the diagnosis, it is necessary to take a liver test and a biochemical blood test.
If one or more diseases are detected, therapy must be started immediately. With effective and successful treatment, the platelet count will also return to normal. Constant monitoring of your health will allow you to see deterioration in time and make predictions, as well as change your treatment regimen.
In addition to pathological processes in the body that could provoke a decrease in PDW, improper preparation for the analysis could lead to this phenomenon. To exclude false test results, it is necessary to retake it.
Low values
An insufficient concentration of platelets per 1 liter of blood negatively affects its clotting.
At low thrombocrit values, the risk of causeless bleeding (both external and internal) increases, which will be very difficult to stop. Depending on the age and gender of the patient, hematologists and therapists differently characterize the identified indicator as low.
According to the standards:
- for women it is less than 0.14%;
- for men - similarly;
- for pregnant women or girls taking a blood test at the beginning of the cycle - below 0.06%;
- for people over 75 years old - less than 0.16%;
- for children aged from birth to 12 months – below 0.1%;
- for children older than one year – less than 0.17%.
The platelet count may decrease due to existing pathological processes or due to previously suffered diseases.
Most often, such changes in the composition of the blood are caused by:
- a tendency to develop anemia (low hemoglobin or “anemia”);
- renal failure;
- liver problems;
- deficiency of vitamins, in particular folic acid;
- infectious or viral disease;
- lupus erythematosus disease;
- existing leukemia or hemoblastosis;
- indiscriminate use of antibacterial and diuretic drugs;
- recently completed chemotherapy;
- intoxication of the body;
- radiation damage;
- underweight;
- the presence of intestinal parasites.
It is possible to normalize thrombocrit levels only with the help of an integrated approach. The patient is usually recommended to review his diet and undergo a course of drug therapy.
In your daily menu you should focus on:
- fruits (bananas, apples, pomegranates, melons);
- vegetables;
- seaweed;
- gluten-free porridges (buckwheat, rice, corn);
- nuts (hazelnuts, walnuts);
- peas;
- beans;
- lean meat (in particular beef);
- fresh herbs;
- green tea
Among the drugs used to increase the level of platelets in the blood, the most effective are:
- "Dicinon" (a drug for the treatment of capillary bleeding);
- "Derinat" (remedy for parasites);
- "Vikasol" (medicine for hemorrhagic disease and hypovitaminosis).
After treatment, it is necessary to take a blood test again to ensure that the thrombocrit level has returned to normal.
Reasons for the increase
If the blood test results for PDW are elevated, we may be talking about the presence of the following diseases:
- Oncological pathologies. In the presence of malignant tumors, there is an increased production of platelets that have different sizes and properties. Platelet platelets contribute to the development of cancer by helping cancer cells spread through the body and become metastases.
- Severe blood loss. With a lack of blood, the bone marrow begins to function intensively, producing new blood elements, including platelets. Before cell gluing, the distribution width increases sharply, causing the analysis result to deviate greatly from the norm.
- Chronic inflammatory processes. Along with the production of leukocytes, platelet maturation increases. Some cells are larger in size and have a longer lifespan. This affects the PDW index, which can be many times higher than the established standards.
Other reasons leading to changes in analysis results include:
- anemia of various origins (the width of platelet distribution increases in response to a decrease in hemoglobin levels);
- pregnancy and lactation;
- recovery after complex surgery;
- helminthic infestations (a change in the test result means the body is highly sensitive to substances secreted by parasites);
- heavy menstruation, accompanied by severe blood loss;
- psycho-emotional overload;
- eating before the test;
- use of certain medications;
- increased activity of the thyroid gland and adrenal glands.
Why are platelets needed in the blood?
Platelets are components of blood that, together with plasma coagulation factors, protect the body from bleeding. It is platelets that respond to vascular damage by forming a blood clot.
In their normal state, platelets circulate in the blood in free form and are represented by nuclear-free fragments of the cytoplasm of megakaryocytes. In a healthy person, megakaryocytes are found in the bone marrow in a ratio of 1 to 10,000 bone marrow cells and can vary widely depending on diseases.
Normally, platelets in the blood of men and women are represented by biconvex disc-shaped lens-shaped structures with a diameter of 2-3 microns. The ratio of platelets to red blood cells in human plasma varies from 1 in 10 to 1 in 20.
However, depending on age and individual characteristics, the normal number of platelets in the blood may vary.
Platelet-related disorders can be divided into the following groups:
- Thrombocytosis (platelets in the blood are increased);
- Thrombocytopenia (platelet levels in the blood are low);
- Thrombocytopathies (the normal number of platelets in the blood is determined, but their properties are impaired).
Regardless of who has elevated platelets - an adult or a child, it is customary to distinguish between primary and secondary (reactive) thrombocytosis. Primary thrombocytosis was first discovered in 1934 and was called hemorrhagic thrombocythemia. While secondary thrombocytosis is a consequence of the body's reaction to external factors, primary thrombocytosis is a manifestation of bone marrow dysfunction. In 2021, scientists from Nassau Medical University, New York, published the results of a scientific study, according to which primary thrombocytosis occurs with a frequency of 2 people per 100,000 population and is almost always combined with anemia and leukocytosis.
What are platelets?
Platelets (PLT) are cells designed for the stable functioning of the body's blood vessels. The site of PLT formation is the bone marrow. The method for determining blood platelets is a general blood test.
Blood plates perform a number of functions:
- Hemostatic - for skin lesions, PLTs are combined into large and small groups to stop bleeding.
- Nourishing - in case of wounds or damaged skin, they nourish the inner surface of blood vessels.
- Protective - can independently absorb small bacteria (phagocytosis).
- Transport - capable of delivering various substances to the body, for example, serotonin.
- Strengthening - help maintain the density of the walls of blood vessels to reduce their premature destruction.
The optimal PLT level is 150-400*109/l. These indicators depend on the patient’s age, as well as gender and general condition of the body. In addition, platelet values change by 10-15% throughout the day.
In medicine, it is worth distinguishing 5 forms of blood platelets, namely:
In addition, PLTs go through 3 stages to stop bleeding, namely:
- Adhesion is the adhesion of blood platelets to the walls of a damaged vessel.
- Activation - enlargement of cells in order to increase the area of interaction.
- Aggregation is the sticking together of PLT with the help of fibrinogen (via receptors).
Increasing the width of platelet distribution by volume
Diagnostically significant parameters that assess the state of the level of enzyme platelets in the blood in relation to its total volume include the width of the distribution of platelets.
Based on the analysis data, it is possible to diagnose the presence of a pathological increase in values and suggest the reasons that caused the appearance of the symptom.
Based on the analysis data, it is possible to diagnose the presence of a pathological increase in values and suggest the reasons that caused the appearance of the symptom.
The role of platelets in the body
Platelets are small, anucleate, red, spherical plates of blood ranging in size from two to four microns.
These blood elements, formed in the red bone marrow with the direct participation of megakaryocytes, are involved in maintaining homeostasis in the body.
The main function of small blood plates can be defined as protective - after all, they are actively involved in blood clotting.
The process by which blood “clottes” is called hemostasis. With the help of hemostasis, the body fights bleeding, preventing blood loss.
Platelets perform their main function due to their ability to transform their shape. When blood elements are activated, specific growths are formed on their body - pseudopodia.
They add special qualities to platelets, giving them the ability to form bonds with different surfaces.
If necessary, small blood plates activated in this way can unite with each other, forming a dense “lump” and aggregating.
Pseudopodia help platelets attach to damaged vessel walls, “plugging” gaps in the structures of the circulatory system.
Formed clots from platelets are not permanent - normally, after a certain period of time (when the damaged area has time to recover), they “resolve” without creating “congestion” in the vessels and without interfering with blood flow.
Depending on age, size and condition, 5 forms of platelets are distinguished:
- young;
- ripe;
- old;
- activated;
- degenerative.
As you age, the size of blood cells decreases.
Indications for analysis
Determination of platelet population breadth is required in the following cases:
- Planned hospitalization. The study is included in the list of mandatory tests required for the initial assessment of the body’s condition.
- Monitoring the effectiveness of therapy. The PDW reading in a blood test helps determine whether treatment is working. If the value remains unchanged after conducting the study twice, the treatment regimen is adjusted.
- Regular medical examination. Mandatory for children and workers in some industries.
- There are suspicions of pathologies of the hematopoietic system or cancer. Analysis of the platelet distribution index helps to identify signs of chronic inflammatory diseases.
How is it carried out?
To determine the required indicator, blood is taken from a finger. The material is placed in a test tube with an anticoagulant. Using special equipment, the width of the platelet distribution is studied and the cell sizes are assessed. To obtain reliable results, physical activity and stress are excluded before taking the test. Blood is donated in the morning on an empty stomach.
Increased PDW level: what pathologies does this indicate?
Platelet indices increase in cases such as :
- presence of anemia (especially during pregnancy);
- blood was drawn incorrectly;
- presence of cancer;
- severe blood loss during surgery or during menstruation in women;
- the presence of an inflammatory process, in which the number of platelets sharply increases, as evidenced by an increase in the width of the distribution.
Often, when a blood test is suspected of cancer, they are forced to retake it several times, taking into account all the nuances of the procedure. Many patients are unaware of how to prepare properly, which results in inaccurate data. Only those cases where abnormalities in the blood test are noted not only in the PDW indicator, but also in other indicators deserve special attention.
What does the PDW index mean in a blood test: interpretation and norm
Blood contains various enzymes and substances
Currently, up to 24 different indicators are known in medicine that are important for the functioning of the human body. Of these, the most vital are leukocytes, hemoglobin concentration, red blood cells, hematocrit, platelets and the average concentration in the blood of each of them.
About hematocrit norms in children:
PDW indicator refers to blood platelet indices. The transcript of the analysis characterizes the relative width of the distribution of platelets by volume. In other words, it is also called an indicator of platelet heterogeneity. Accordingly, there is a certain norm that must be present in the blood. Otherwise, the patient will experience disruption of the circulatory system, possible chronic or acute diseases and other abnormalities.
For example, the normal width of platelet distribution by volume is in the range of 15% - 17%. If this percentage is increased, then they speak of a violation of the size of the platelet population. Platelet indices also include MPV - the average platelet volume, the norm of which ranges from 7 to 10 fl. PCT - thrombocrit, the component norm is 0.108 - 0.282 as a percentage of the entire proportion of blood that is occupied directly by platelets.
Details about thrombocrit:
Laboratory research
No special preparation is required to determine the test results. General analysis in this regard is very convenient, as it allows you to identify the presence of a particular problem in a patient at any time of the day. Only in this case there are some restrictions regarding food intake or medications. Therefore, it is still recommended to take a general analysis in the morning on an empty stomach, when there are no additional irritants for false results.
Blood is most often taken from a finger capillary, but there are cases of venous blood taken. This can only be explained by the fact that venous blood contains a larger and clearer amount of exactly those indicators that are expected from the analysis. For example, if one or another component is elevated, then in venous blood this figure will be more clear. This way you won’t have to take the test again. But for children, it is easier to transfer blood sampling from a finger, as it is faster and more convenient for the nurse herself.
The collected material is immediately sent for laboratory testing. Therefore, results should be ready in as little as two days, depending on the laboratory. It is also worth noting that you should not always rely on the results of one laboratory. This can be explained by the fact that each research point uses certain equipment and different reagents. Therefore, sometimes false results come. For greater reliability, it is better to take tests in two or three laboratories at once, so that the doctor can see the overall picture of the examination and prescribe further treatment.
Nuances and features of a general clinical blood test:
results
Research and analysis preparation are carried out in the laboratory
The interpretation of each analysis is carried out directly in the laboratory when examining the material. The patient receives ready-made results, which indicate the rate of the indicator or its increase. If the PDW result is still significantly elevated, this may indicate the presence of cancer. But it is worth considering that the norm of all others is also absent. If only one pdw is elevated, and everything else is within normal limits, then the cause must be sought in other ways.
Possible symptoms
There will be no specific clinical picture. Symptoms will depend on the underlying factor; the collective symptom complex may include the following:
- weakness, increasing malaise;
- sleep cycle disturbance - drowsiness or, on the contrary, insomnia;
- dizziness, frequent headaches;
- nosebleeds may be present;
- decreased ability to work, apathy and irritability;
- unstable blood pressure;
- pale skin;
- hemorrhagic rashes;
- exacerbation of chronic diseases - will be accompanied by additional symptoms;
- nausea and vomiting;
- disruption of the functioning of the gastrointestinal tract;
- symptoms of general intoxication.
This clinical picture can be present in almost any disease, so there is no need to self-medicate - you should consult a doctor for advice. The doctor will determine exactly what the relative width of the platelet distribution across the volume is.