Treatment under the compulsory medical insurance policy is possible!
Submit your application
Follow the news, subscribe to our social networks
Details
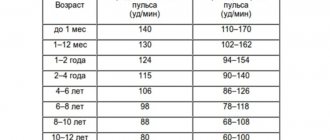
Heart rhythm disorders (arrhythmias) are conditions in which the heart beats irregularly, too fast, or too slow. With frequent heart contractions - above 100 beats per minute in adults, this condition is called tachycardia, with rare - less than 60 beats per minute, it is called bradycardia. Some types of arrhythmia have no symptoms. If the arrhythmia is symptomatic, then the main complaints are palpitations or a feeling of a pause between heartbeats. Sometimes patients may complain of dizziness, fainting, shortness of breath or chest pain. Most types of arrhythmia are not a serious threat to the patient, but complications such as stroke or heart failure can often occur, and sometimes the arrhythmia can lead to cardiac arrest.
The Innovative Vascular Center employs experienced cardiologists who will help determine exactly why cardiac arrhythmia occurs and prescribe the correct treatment. In addition to drug therapy, our clinic implants artificial pacemakers (pacemakers) of any configuration. Timely and correct treatment allows our patients to avoid many complications, which means prolonging life and improving its quality.
Slow heartbeat - bradycardia
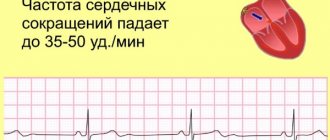
Bradycardia is a condition where the heart beats so slowly that it cannot pump enough blood to meet the body's needs. If bradycardia is left untreated, it can lead to extreme fatigue, dizziness, or fainting because not enough blood is supplied to the brain. This condition can be corrected by using an electronic pacemaker, which makes the heart beat normally.
Bradycardia occurs for various reasons:
- Sick sinus syndrome
The appearance of sinus bradycardia as a result of a “malfunction” in the sinus node (the natural pacemaker of the heart) occurs when discharges for contractions occur too infrequently. A weak sinus node can develop with age or be a consequence of illness. Some medications may also cause or worsen bradycardia. This arrhythmia may be temporary or permanent. It can be treated with medications or an electronic pacemaker.
- Blockage of the heart pathways
Heart block is a slowing or interruption of the electrical signal to the lower chambers of the heart (ventricles) that cause the heart muscle to contract. The heart's electrical conduction system typically sends signals from the upper chambers of the heart (atria) to the lower chambers (ventricles), which causes coordinated contractions of the heart muscle. Complete blockade of the atrioventricular node can manifest as a sudden loss of consciousness, since the ventricles contract very rarely without stimulus from the sinus node. An artificial pacemaker can eliminate this problem and normalize heart function.
Expert advice: “5 signs that it’s time to see a doctor”
An increased heart rate in itself does not necessarily indicate any illness. It is important under what circumstances this happens and what is accompanied by it. The following are situations in which you should consult a doctor:
- rapid heartbeat appears at rest;
- an increase in heart rate is accompanied by severe pain in the heart;
- the person often loses consciousness;
- tachycardia occurs sharply and suddenly and also stops;
- an increase in heart rate worsens the symptoms of existing cardiac pathology.
Rapid heartbeat - tachycardia
- Supraventricular tachycardia
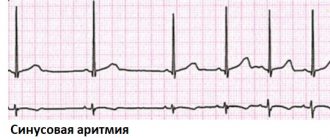
This is a rapid heartbeat in the atria (upper chambers of the heart) or in the atrioventricular (atrioventricular) node, the electrical connection between the atria and ventricles. The first signs of atrial fibrillation are usually detected on an ECG. Atrial fibrillation can be permanent or paroxysmal (periodic) in form, which determines the approach to treatment. Sinus tachycardia is a rapid heartbeat with the formation of regular complexes on the ECG. Sinus arrhythmia is usually associated with an emotional background, elevated temperature, endocrine diseases of the thyroid gland, as well as a predominance of the sympathetic autonomic nervous system.
- Atrial flutter
For atrial flutter to occur, an additional or early electrical impulse must move around the atrium in a circular path rather than along its normal path. This electrical signal causes the atria to contract very quickly, which is usually not life-threatening, but can cause chest pain, dizziness, or other more serious problems. Many chronic heart diseases lead to the development of flutter and atrial fibrillation - its variety.
- Atrial fibrillation
Coronary heart disease often leads to arrhythmia. This common form of tachycardia is more common in women and occurs when there is excess electrical activity in the atria that is extremely disorganized. The manifestation of this electrical activity is very frequent and chaotic contractions of the atria. The atria lose their contractile function, which leads to stagnation of blood in them and can contribute to the formation of clots. Blood clots are the main cause of complications and danger of atrial fibrillation, since they can break away from the atria and enter the general bloodstream. Such a blood clot can cause a blockage of any artery in the body (embolism), leading to a stroke or gangrene of the limbs.
- Paroxysmal supraventricular tachycardia (PSVT)
With PSVT, heart rate increases from 140 to 250 beats per minute (the norm is 60-90 beats per minute). Why does this condition happen, cause trouble, but rarely life-threatening? The causes of this type of cardiac arrhythmia are associated with congenital additional electrical pathways between the atria and ventricles. Idiopathic supraventricular tachycardia is treated by destroying additional electrical pathways using radiofrequency ablation. Tachycardia is felt as an increased heartbeat and is very worrying for patients.
- Wolff-Parkinson-White syndrome (WPW)
In people with Wolff-Parkinson-White syndrome (WWS), extra, abnormal electrical pathways in the heart lead to periods of very fast heartbeat (tachycardia). Most people with WPW syndrome can lead normal lives. Many have no symptoms and no episodes of tachycardia. In some people, WPW syndrome can cause a rapid heartbeat (paroxysmal supraventricular tachycardia), when the heart rate rises to 240 beats per minute (normal is 60 to 80 beats per minute). Other symptoms include palpitations, shortness of breath, fainting, and angina (chest pain) with exercise. The first symptoms of this form of cardiac arrhythmia do not always require treatment, but a thorough examination by a cardiologist is necessary.
- Ventricular tachycardia
Ventricular tachycardia occurs when the ventricles (lower chambers of the heart) contract too quickly, making this arrhythmia life-threatening. This condition can be very serious as the ventricles are responsible for pumping blood to the rest of the body. If the tachycardia becomes so severe that the ventricles cannot pump blood effectively, it can be life-threatening. Tachycardia can be treated with medications. Other procedures include implantation of a defibrillator, catheter radiofrequency ablation, or surgical removal of the heart's accessory pathways. Ventricular extrasystole is a cardiac arrhythmia, which manifests itself as a sudden strong interruption in the functioning of the heart. It is clearly visible on the ECG and interrupts the normal heart rhythm. Bigemeny is one extrasystole every normal cardiac cycle. Trigemeny - extrasystole after two normal cycles. This poor prognostic sign is of great importance and requires immediate attention to a cardiologist.
- Ventricular fibrillation
Erratic and inefficient contractions of the ventricles occur when the electrical signal that normally causes the heart to beat breaks up and travels along random paths around the ventricles instead of following its normal route. The result is a series of rapid but ineffective contractions of the ventricles, leading to loss of consciousness as a result of a sharp drop in blood pressure. This means that without emergency treatment, fibrillation becomes fatal, as it turns off the pumping function of the heart and stops blood circulation. Fibrillation can be stopped with an electric shock or a blow to the heart using a defibrillator. The discharge allows you to “reset” the electrical activity of the heart and return to normal rhythm. Ventricular fibrillation occurs with myocardial infarction, severe chronic heart disease, hemorrhagic shock, and intracardiac procedures.
Symptoms of the disease
Tachycardia, which is a sign of a disease, is characterized by the following symptoms.
- A feeling of interruptions and/or “failures” in the functioning of the heart is the most common manifestation.
- Shortness of breath (lack of air), which occurs with little physical activity or even at rest.
- Pain in the heart (accompanies an attack of tachycardia in vegetative-vascular dystonia and some other diseases).
- Dizziness and darkening of the eyes, lightheadedness and even fainting (this is due to impaired blood supply to the brain).
In general, the manifestation of clinical symptoms of tachycardia depends on the nature of the underlying disease, as well as on the severity and duration of the arrhythmia itself.
Forecast
Cardiac arrhythmias are dangerous because they can lead to sudden cardiac arrest due to complete blockade of conduction. In severe arrhythmia, there is a high risk of ventricular fibrillation, which can be fatal. Atrial fibrillation leads to the formation of blood clots in the atria and their transfer to other organs with the development of stroke and gangrene of the extremities. The probability of an unfavorable outcome in patients with arrhythmias depends on the form of rhythm disturbance and is more than 20% per year. You should not rely on folk remedies - arrhythmia is very dangerous and requires correction by a professional cardiologist.
Symptoms and signs of the condition
Often, TS does not manifest itself in any way and the person feels great. Some patients experience rapid heartbeat, fatigue, dizziness, and nausea. In people suffering from neuroses, this may be accompanied by a feeling of fear.
In POTS, these symptoms occur when a person lies for a long time and then suddenly stands up, but they quickly pass (within a few minutes).
Some patients tell me that they experience difficulty breathing and pain in the heart, and may even faint due to a decrease in blood pressure.
With TS, the course of cardiac disease may become more severe.
In addition to these complaints, patients with autonomic dysregulation syndrome have many other symptoms: chilliness, cold extremities, tingling sensation in the arms and legs, various gastrointestinal disorders (belching, flatulence, heaviness in the abdomen, intermittent constipation or diarrhea) with absence of confirmed gastroenterological disease, sweating, menstrual irregularities in women.
There are no specific changes on the cardiogram, except for an increase in heart rate, with TS.
Paroxysmal variant
Paroxysmal TS is called sinoatrial reciprocal tachycardia (SRT). This is a fairly rare form: among all types of paroxysmal tachycardias, it accounts for about 2-3%. Its distinctive feature is the sudden onset and cessation of tachycardia.
I see this type of progression only in people with cardiac pathology.
Since this tachycardia begins acutely, clinical manifestations (dizziness, difficulty breathing, heart pain) are more pronounced than with simple CT. Although asymptomatic attacks are also possible.
With CRT, an atrial extrasystole is always present on the electrocardiogram before the paroxysm.
Moderate tachycardia
A slight increase in heart rate (from 90 to 110) is called moderate tachycardia. The reasons for its occurrence are no different from ordinary TS. It may reflect the severity of the disease or condition that is causing the heart rate to increase.
Although most patients may not feel mild tachycardia, it requires the same attention as TS.
Paroxysmal tachycardia: danger and risk groups
Paroxysmal tachycardia has a negative impact on human health. This is expressed as follows:
- “wear and tear” of the heart muscle;
- cardiogenic shock;
- the efficiency of the circulatory system decreases;
- development of heart failure;
- pulmonary edema.
A recurrent form of the disease can trigger the occurrence of arrhythmogenic cardiomyopathy. In especially severe cases, the disease can cause clinical death and death.
Most often, paroxysmal tachycardia affects older people with a history of heart attack, myocardial disease, coronary heart disease and those with hypertension or heart disease.
Diagnosis and treatment
Vertical sinus tachycardia requires immediate diagnosis and treatment.
To identify such a disease, it is necessary to carry out a number of studies. Among them, the leading role is given to the ECG. After all, daily Holter ECG monitoring is highly informative and harmless to the patient.
How is sinus tachycardia treated? Heart rate must be brought to the optimal level.
It involves a number of measures to reduce the purity of heart contractions and is carried out with the help of sedatives, as well as consultations with a psychologist. If there is reflex or compensatory tachycardia, it is necessary to eliminate the causes of the problem. Otherwise, therapy to reduce heart rate can cause a drop in blood pressure and only worsen the situation.
Tachycardias: the same, but different
The myocardium consists of two types of cells - typical, which only contract, and atypical. The latter perform a function unusual for muscle cells: an electrical impulse appears in them, which is transmitted further along the conduction system of the same cells and ensures contraction of the heart chambers. Large collections of such cells are called nodes.
Heart rate can accelerate any element of the cardiac conduction system
The main elements of the conduction system are, in descending order:
- sinoatrial node (it is also called the pacemaker, since normally the heart contracts precisely at its command) - it is located above the right atrium;
- atrioventricular node (or AV node) - a collection of atypical myocardial cells at the border of the atria and ventricles;
- His bundle is a group of cells that transmit impulses from the AV node to the ventricles through Purkinje fibers.
Each of these elements has its own electrical activity, which is why a variety of tachycardias arise: an increase in heart rate (HR) can occur at any stage of the impulse. Therefore, all tachyarrhythmias (disorders of the heart rhythm according to the type of acceleration) are divided into two groups depending on the source of impulse generation:
- 1 Supraventricular - the impulse is born in the atria or above the His bundle (in the sinoatrial or atrioventricular node).
- 2
Ventricular - the source of the impulse is the bundle branches, Purkinje fibers or working ventricular myocardium.
The group of supraventricular tachycardias includes sinus tachycardia. This is the only physiological type of heart rate acceleration that occurs during stress, in children and pregnant women. All other supraventricular and ventricular types of tachycardia do not occur normally
In pathological types of tachycardia, the source of rhythm becomes another element of the conduction system, which generates impulses with a frequency greater than the sinus node
Treatment of sinus arrhythmia
Physiological sinus arrhythmia does not require treatment. Occasionally, herbal sedatives are prescribed.
To get rid of pathological sinus arrhythmia, you need to cure the disease from which it is a consequence.
For sinus tachycardia, treatment is predominantly medicinal and aimed at reducing the heart rate. For this purpose, sedatives (motherwort, valerian), beta-blockers, etc. are used.
Treatment of sinus bradycardia is aimed at increasing the heart rate. For this purpose, both medications (sympathomimetics, anticholinergics) and implantation of an electrical pacemaker are used for severe bradycardia that threatens the patient’s life.
Sinus extrasystole is treated with antiarrhythmic drugs.
Causes
The disease is provoked by the following factors:
- heart failure and a high risk of heart attack, myocarditis, cardiosclerosis, etc.
- disruptions of the endocrine system: can be provoked by thyrotoxicosis, increased production of hormones such as adrenaline in pheochromocytoma;
- physical and psycho-emotional stress: stress, excessive enthusiasm, hard work;
- pregnancy: sinus tachycardia during pregnancy is quite common and requires close monitoring by the medical professional who is caring for the woman’s pregnancy;
- disorders of the autonomic nervous system: neurosis, affective psychosis; cardiopsychoneurosis;
- congenital anomalies of the body's development.
All these factors that cause problems with heart rhythm in a healthy person, in women during pregnancy or in children, can be observed in combination, or they can appear one at a time.
Atrial or ventricular fibrillation
Fibrillation, or flicker, of the myocardium is called frequent uncoordinated contractions. Both the upper parts of the heart (atria) and the lower parts (ventricles) can flicker.
Fibrillation is the immediate mechanism of sudden cardiac death. If you suspect atrial fibrillation, you should immediately seek medical help
With fibrillation, a full contraction of the cardiac sections does not occur: one common impulse breaks up into parts, randomly twitching the myocardium without the slightest synchronization. This leads to stagnation of blood inside the chambers of the heart. Organs in the systemic circulation begin to experience oxygen starvation, like the heart muscle itself. At this time, blood stagnates in the cavity of the atria or ventricles, which increases the risk of blood clot formation. If the heart finally contracts with sufficient force, blood clots will enter the bloodstream and are likely to block the arterial ducts.
Complications of fibrillation:
- heart failure
- stroke
- heart attack
- thromboemoliia (blockage with thrombotic masses) of the vessels of internal organs and extremities
The risk of thromboemolius after an episode of fibrillation persists for up to three weeks.
The tricky thing about fibrillation is that its episodes can be asymptomatic. However, atrial fibrillation never occurs in a healthy heart. This obliges everyone who has a disease of the cardiovascular system to regularly visit a cardiologist to assess the condition of the heart and blood vessels, as well as to know first aid techniques for episodes of tachycardia.
Prevention of tachycardia development
Tachycardia itself is not a disease - it is only a symptom that indicates the presence of other heart problems. Therefore, prevention should be aimed at preventing the development of cardiovascular pathology.
Primary prevention of myocardial diseases (preventive measures recommended for people with a healthy heart and blood vessels) is compliance with the tenets of a healthy lifestyle. These include sufficient physical activity, maintaining optimal body weight, giving up bad habits, getting enough sleep and a balanced diet. Particular attention to these rules should be paid to people with established risk factors for the development of cardiovascular pathology.
Secondary prevention measures should be taken by people with already diagnosed heart disease to avoid complications. These measures include following the recommendations of your doctor, taking prescribed medications and timely visits to your cardiologist. Visit your doctor at least once a year before age 35, or once every six months after age 35.
How it appears
This disease can be diagnosed in completely healthy people of different age categories. However, it is more common in women and men of older age groups with heart problems. Sinus tachycardia can often be detected in a small child.
What causes an increase in the number of heart contractions, and what are the causes of a disease of this nature? In a healthy body, the automatism of the sinus node increases during psycho-emotional or physical overload, as well as with excessive consumption of coffee and other caffeine-containing products. Thus, the body ensures optimal blood supply to all organs during those moments when it performs strenuous work.
In other words, this is a completely adequate reaction of a healthy body to the active work of the sympathetic nervous system. Also, sinus tachycardia code ICD can also be observed in a person with a completely healthy heart, but if he is infected with any infection, suffers from anemia, or has problems with the thyroid gland. In addition, it is worth noting that such problems can be caused by such means as:
- aminophylline;
- glucocorticoid hormones, etc.
Clinical case
A 39-year-old woman consulted her local physician with complaints of constant rapid heartbeat up to 110 per minute and periodic dizziness. These symptoms have been bothering the patient for a month. According to the patient, the pulse was always within 70-80/min. Upon examination, a high heart rate (106/min) and a slight increase in blood pressure (130/80 mmHg) were revealed. The ECG showed sinus tachycardia. No clinical or laboratory signs of heart disease or other pathologies were found. Upon detailed questioning, the patient noted that she suffers from chronic rhinitis and takes vasoconstrictor nasal drops (Naphthyzin) 8-10 times a day for 2 months. A referral to an otolaryngologist was issued. Some time after the prescription of competent therapy, the pulse and blood pressure returned to normal.
How is sinus tachycardia treated?
Since sinus tachycardia has many causes, it is first necessary to find out why it developed.
Treatment of sinus tachyarrhythmia includes non-drug and drug methods. Non-drug treatment involves quitting smoking, limiting alcohol consumption, and eliminating coffee from the diet.
Therapy of the underlying disease quickly leads to normalization of heart rate.
If TS occurs against the background of a neurotic condition, sedatives (tranquilizers) and antidepressants (Fluoxetine) in tablet form are used.
I recommend that patients with postural tachycardia syndrome take a contrast shower and consume sufficient amounts of water and salt. If this turns out to be ineffective, I prescribe Fludrocortisone, a mineralocorticoid hormonal drug that allows you to retain fluid in the vascular bed.
To relieve an attack of SRT, the vagal Valsalva maneuver is very helpful - straining the face with swelling of the cheeks for 20-30 seconds after maximum inhalation.
If TS is accompanied by severe symptoms (poorly tolerated by the patient), I use medications.
In my practice, I prefer beta-blockers - Bisoprolol (Concor), Metoprolol, Nebivolol. These drugs reduce the sensitivity of the heart to various stimulating factors, and also slow down the conduction of nerve impulses in the conduction system.
Beta-blockers are excellent for people both without cardiac pathology and with heart disease (chronic heart failure). However, in some cases they are contraindicated, for example, for people with severe broncho-obstructive diseases (COPD, bronchial asthma).
Ivabradin (Coraxan), a blocker of If channels of the sinus node, has a good “pulse-cutting” effect. Calcium channel blockers (Verapamil, Diltiazem) also reduce heart rate quite well. These drugs should not be used in patients with severe heart failure (FC III-IV).
If the use of these drugs is unsuccessful, I prescribe cardiac glycosides (“Digoxin”). But you should be careful with them, as they can provoke other heart rhythm disturbances.
To prevent attacks during paroxysmal SRT, antiarrhythmic drugs are effective, stabilizing the cells of the conduction system and normalizing the pulse rate - Propafenone, Flecainide.
All of the above measures allow me to achieve a decrease in heart rate in the vast majority of patients.
However, it happens that no drug therapy helps. If CT significantly worsens the patient’s condition, I turn to cardiac surgeons to perform RFA (radiofrequency ablation). In this operation, the area of the heart that causes TS is destroyed by high-frequency current. However, after RFA, a permanent pacemaker is almost always required.
RFA should be the last treatment for TS when everything else has been tried.