At the first visit and for certain indications, a pediatric cardiologist in Saratov will be able to determine whether the child has bradycardia. The main feature of the disease is a decrease in the working pulse rate, which can be expressed to varying degrees. It is extremely important for parents to show their child to a specialist at the First Children’s Medical Center on time, undergo the necessary examinations in pediatric cardiology in Saratov, take tests and, based on their results, receive a doctor’s conclusion and recommendations.
Causes
So, bradycardia in children is a decrease in heart rate from 5 to 40% below normal. The complex formulation is explained by two phenomena. Firstly, a child’s heart beats much faster than an adult’s. Secondly, each age has its own normal heart rate.
Even when the baby is in the womb, the fetal heart rate changes at different stages of pregnancy.
Before the heart contracts, a nerve impulse first originates in the sinus node, which is located in the right atrium. Then the excitation wave propagates through the conduction system to the ventricles. When it reaches them, the myocardium contracts and blood is released into the vessels.
Bradycardia can develop as a result of a slowdown in the formation of nerve impulses or an increase in the time they take to travel through the conduction system of the heart.
This can happen due to the following reasons:
- heart diseases - myocarditis, congenital defects (atrial or ventricular septal defects, arrhythmogenic right ventricular dysplasia, etc.);
- diseases of the endocrine system - the most prominent representative is hypothyroidism (decreased synthesis of thyroid hormones);
- high concentration of potassium in the blood - this can happen, for example, in severe diseases accompanied by renal failure;
- infections – typhoid fever, brucellosis, mumps;
- overdose of certain medications;
- congenital anomalies of the cardiac conduction system.
Bradycardia in the fetus during pregnancy can occur both as a result of developmental defects (for example, heart defects) and as a result of maternal diseases - severe anemia, thrombosis, systemic vasculitis, etc.
There is a phenomenon called “benign bradycardia-asystole in the fetus.” It usually develops in the second trimester of pregnancy. These are short episodes (just a few seconds) of bradycardia and complete cardiac arrest. They are temporary and absolutely safe for the health and life of the child.
Bradycardia in newborns usually indicates a serious condition of the baby (for example, prematurity) and requires urgent resuscitation measures.
Signs and symptoms
The clinical picture directly depends on the degree of bradycardia. With a slight slowdown in heart rate, the child can feel great without experiencing any discomfort.
With a more pronounced decrease in heart rate, the child becomes less energetic, he gets tired quickly, he is constantly sleepy, and his skin becomes pale. His head is spinning and his vision is getting dark. He may even faint.
Sometimes I had to observe children who, due to severe bradycardia, lost consciousness, their heart stopped beating for a while and their breathing stopped, then convulsions began. After a few seconds or a couple of minutes, the child comes to his senses. This resembles an epileptic seizure. This phenomenon is called Morgagni-Adams-Stokes syndrome. It develops when the heartbeat is very slow. Its occurrence is due to severe hypoxia (oxygen starvation) of the brain.
An attack of Morgagni-Adams-Stokes syndrome is a very dangerous condition, as it can lead to the rapid death of a child.
In what cases should you immediately consult a doctor?
If your child does not exercise seriously and his heart rate is lower than normal for his age, he should be seen by a cardiologist, but not necessarily right away. It’s another matter if he is lethargic, sleepy all the time, and faints. In this case, a visit to the doctor should not be postponed. And finally, if a child develops an attack of Morgagni-Adams-Stokes syndrome, you need to call an ambulance.
Medical indications
- pallor;
- constant fatigue;
- presence of shortness of breath;
- dizziness that occurs in attacks;
- presence of pain in the chest area;
- fainting or even semi-fainting.
To prevent bradycardia, you need to follow a special diet:
- Drink more fluid 1.5 - 2 liters per day.
- There are many vegetables and fruits. Eat enough carrots and cabbage in particular.
- You should eat lean meat.
- From fruits: apples, bananas and citrus fruits.
- There are fermented milk products.
- Seafood can also be eaten.
In addition to diet, hardening and moderate physical activity are useful.
What bradycardias are most common in children?
Depending on the mechanism of development (slowing the formation or conduction of a nerve impulse), as well as on electrocardiographic signs, the following types of bradyarrhythmia in children are distinguished:
- sinus;
- atrioventricular (atrioventricular) blockades of II and III degrees;
- intraventricular blockades (bundle branch blocks);
- sick sinus syndrome.
There are also intraatrial blocks, but they are rarely accompanied by a slow heartbeat. You can find out more about what it is and how to act correctly here.
Attacks of Morgagni-Adams-Stokes syndrome occur with atrioventricular blockade and sick sinus syndrome
The most common of all forms is sinus bradycardia.
Sinus bradyarrhythmia
Unlike other types, with sinus bradycardia the heartbeat is slow but rhythmic. It poses the least danger to the health and life of the child, i.e. is the most benign of arrhythmias,
I also want to note that sinus bradycardia is not always a pathology. For example, sinus bradyarrhythmia in a child can be observed during sleep. Children who play sports intensively and regularly perform intense physical exercise also often experience a similar phenomenon, which is the absolute norm. The issue of heart rate slowing in athletes is well discussed here.
Symptoms of cardiac arrhythmia in a child
The symptoms of heart rhythm disturbances have different specifics and differ in children of different age groups.
Arrhythmia in a newborn baby can manifest itself through:
- pale, bluish skin;
- baby anxiety for no apparent reason;
- refusal to eat, breastfeed, or bottle;
- shortness of breath;
- slight or no weight gain;
- problems sleeping, crying.
Arrhythmia in a child aged 6 years and older very often has no symptoms. In such cases, pathology is detected during a routine medical examination. Only sometimes do children exhibit characteristic symptoms of the disease:
- excessive fatigue;
- poor body response to physical activity;
- causeless fainting, dizziness;
- pale skin;
- apathy or increased excitability;
- poor appetite;
- pain in the heart area.
What tests should your child undergo and when?
As the first method of examination, I prescribe electrocardiography. This allows you to determine the type of bradycardia.
ECG signs of sinus bradycardia:
- a decrease in heart rate in the form of an increase in the distance between the R waves;
- correct sinus rhythm - the same distance between the R waves and the presence of positive P waves that have a normal shape in leads II, III and aVF.
ECG signs of atrioventricular block:
- II degree – increase in the PQ interval, periodic loss of the QRS complex;
- III degree – complete inconsistency of atrial and ventricular rhythms, i.e. different number of P waves and QRS complexes.
ECG signs of sick sinus syndrome:
- a decrease in heart rate in the form of an increase in the distance between the R waves;
- attacks of paroxysmal supraventricular tachycardia and atrial fibrillation may occur.
Sometimes bradyarrhythmias can occur in attacks. Therefore, I additionally prescribe Holter (24-hour) ECG monitoring. I also perform echocardiography if a congenital heart defect is suspected.
If, based on the cardiogram data, I suspect that the child has sick sinus syndrome, then to confirm it, I prescribe an electrophysiological study of the heart.
Sinus bradycardia
With bradycardia, the heart rate slows down and becomes less than 60 beats per minute. More often, the cause of bradycardia in adolescents is a violation of extracardiac innervation in the direction of the predominance of the influence of the parasympathetic part of the nervous system on the automatic function of the heart; this may not depend on the degree of physical training (bradycardia of athletes).
Sinus bradycardia, sometimes significant (less than 40 beats per minute), is combined with sinus arrhythmia, which once again confirms its neurogenic genesis, since with myogenic bradycardia the arrhythmia is almost not expressed.
Observations of adolescents with rheumatic heart disease show that sinus bradycardia is rare in this disease; more often, on the contrary, there is a tendency to tachycardia. However, in any case of severe sinus bradycardia, it is necessary to exclude not only rheumatism, but also various brain diseases, endocrine disorders, liver diseases, etc.
A great help in differentiating the neurogenic form of bradycardia from the myogenic one is a test with atropine. In the first case, after subcutaneous administration of atropine, a normal rhythm is established relatively quickly, and then tachycardia occurs. With myogenic bradycardia, a test with atropine causes almost no reaction.
Along with this, it should be noted that in patients with myogenic bradycardia, the electrocardiogram usually shows signs of myocardial damage. It should be remembered that neurogenic sinus bradycardia can be combined with a slowdown in atrioventricular conduction due to an increase in the inhibitory function of the Aschoff-Tavara node.
In addition, in adolescents with symptoms of vagotonia, other signs are observed, expressed in a tendency to hypotension, increased sweating, a tendency to constipation, often increased secretory function of the stomach, etc.
“Clinic of diseases, physiology and hygiene in adolescence”, G.N. Serdyukovskaya
If anyone can, please advise!
My son (16 years old) went for examination at the direction of the military registration and enlistment office.
So far they have only done an ECG. After reading the result, they called the ambulance for me.
Sinus pacemaker, bradyarrhythmia, heart rate 5668 bpm. Normosystole, avg. Heart rate=60, RR: 0.88 - 1.09. Vertical position of the electrical axis of the heart. Shift the transition zone to the left. Incomplete blockade of the right leg. SRRJ. Rotate the heart clockwise.
History: constant headaches, registered with a neurologist, treated by an osteopath. Heredity on both sides (on the maternal side (heart) - complete chaos :()
Should I do something, wait for it to outgrow or something else?
Treatment
Not all bradycardia requires special treatment. If the decrease in heart rate is insignificant and is not accompanied by any clinical symptoms, therapy is not needed.
The type of bradyarrhythmia also matters. If your child has significant sinus bradycardia (below 25-40% of normal for age) and does not exercise, the first step is to evaluate him for a possible cause of the slow heart rate. This involves checking the blood concentration of thyroid hormones, potassium, measuring intracranial pressure, etc.
Often, eliminating the causative factors is quite enough to normalize the heartbeat.
Unfortunately, there is no effective medicine for the permanent treatment of bradyarrhythmia. To improve the child’s condition only briefly, I use the following drugs - anticholinergics (Atropine) and beta-adrenergic agonists (Isadrin). They allow you to increase your heart rate for a short time.
The most effective treatment for severe bradycardia today is pacing - temporary or permanent.
Temporary pacemaker involves delivering a weak electrical current through the skin of the chest or through the esophagus. In most cases, this allows for normalization of heart rate. Transesophageal stimulation is especially effective for relieving bradycardia in infants and children under 2 years of age.
If it is unsuccessful, then a permanent pacemaker is installed. This is a small device that ensures a normal heart rate. It is sewn under the skin in the subclavian area. Wires from it go through large vessels directly to the heart.
Which sport is suitable
- Swimming. Strengthens the heart muscle and increases endurance.
- Golf. It has a beneficial effect on the body and intellect of the child.
- Race walking. Most of the training takes place in the fresh air, there is no heavy strain on the heart.
- Volleyball. Tempers the body, improves blood circulation.
- Rowing. The concentration of oxygen in the blood increases.
- Classic cross-country skiing. More oxygen enters the blood.
For children with this disease, it is best to engage in sports that do not put too much strain on the child’s heart, and also enrich the blood with oxygen, and at the same time, it is best if the training takes place in the fresh air.
Expert advice
If your child suffers from any cardiac disease and is prescribed drugs such as beta-blockers (Bisoprolol, Metoprolol) and calcium channel blockers (Verapamil, Diltiazem) for treatment, you need to remember that the pulse may slow down while taking them. A decrease in heart rate by approximately 5-10 beats from the lower limit of the age norm is not dangerous. But, if the child’s heart rate decreases more, the cardiologist must be informed about this so that he can adjust the dosage.
“Only the heart of a sick person beats like a clock” James Mackenzie, 2010. “With the help of the pulse one can recognize the existence of a disease in the body and foresee future ones.” Herophilus of Chalcedon, c. 335 BC In my opinion, every parent should be able to count the pulse (the number of heart beats in 1 minute). This can be done by pressing large vessels, usually with the index, middle, and sometimes ring fingers. The pulse can be examined in the shoulder, femur, popliteal region, on the back of the foot, and on the temples. But it is most convenient on the radial artery - on the lateral side of the wrist.
In emergency situations, carotid pulse examination is often used: on the carotid artery, located in the neck, below the hyoid bone and outward from the thyroid cartilage (see picture).
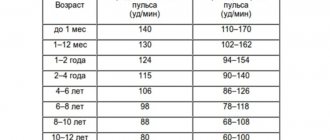
With this measurement method, the artery should be gently palpated while the person being examined is sitting or lying down. Excessive compression of the carotid arteries can lead to fainting or cerebral ischemia. You cannot palpate both carotid arteries at the same time! You can learn to count your heart rate through a phonendoscope, but in this case you will most likely need to consult a specialist, since two tones are heard and you need to distinguish which one is the first, according to which the heart rate itself is calculated. The number of vascular oscillations is calculated in 15 seconds and multiplied by 4, or in 10 seconds and multiplied by 6. So, we will assume that you already know how to count your baby’s pulse. Increased heart rate (tachycardia). Due to the elasticity of the chest and the thin subcutaneous fat layer in a child, even with a slight increase in heart rate, you can see vibration of the anterior chest wall, synchronous with the contraction of the heart, which sometimes frightens parents. A growing body requires intense metabolism and a high need for oxygen. Therefore, the younger the child, the higher his heart rate. Everyone knows this. But where is the limit, exceeding which is no longer the norm? This is an important question that causes concern among many parents. Heart rate norms at rest and after exercise are different. The stress for an infant is feeding, crying, and physical activity. For older people – walking, running, strong emotions (both positive and negative).
Heart rate norms in children at rest.
Table N1 shows the percentile distribution of heart rate by age - from 25‰ to 75‰ - this is the norm. From 75‰ to 98‰ – tachycardia, above 98‰ – severe tachycardia, which, as a rule, is always pathological. Heart rate after exercise is determined by the formula: (220-age) x 0.85. For example, for a 3-year-old child this is (220-3)x0.85 = 184 beats per minute (for comparison, up to 137 is allowed at rest). For the most meticulous parents: if you have calculated and received a figure that exceeds the specified standards by 1-5 strokes, do not worry. In addition, you could have made a mistake; it makes sense to measure several times. All standards are average values and a small deviation is quite acceptable. In addition to the number you received when calculating the pulse, the general condition of the child must be taken into account: if he is active, cheerful, with a normal skin color, there is most likely no reason for concern. In addition to the pulse rate, many parents pay attention to its rhythm. An irregular pulse in a child associated with breathing is normal. If you can ask your baby to hold his breath for a while, the pulse immediately becomes more rhythmic.
NB! If the pulse significantly (by 10-20 or more beats) exceeds the norm, if its irregularity is not associated with breathing, the child is pale, lethargic, the nasolabial triangle is gray, shortness of breath is a reason to consult a doctor. Registration of a pathologically rapid pulse is not necessarily associated with problems of the cardiovascular system, but also with pathology of other internal organs, especially the gastrointestinal tract and endocrine system. In routine practice, most often, this is the debut of some acute infectious disease that has not yet manifested itself. Decrease in heart rate (bradycardia). As a practicing pediatrician and cardiologist, I can say that over the past 10 years the number of children with a pulse lower than average has increased significantly. There is no evidence base for this phenomenon in the medical literature available to me, so I can only assume that this may be the result of widespread physical inactivity and a passion for gadgets, which we will talk about in a separate conversation. If a rare pulse is detected, this is a reason to contact a pediatric cardiologist. But don’t be surprised if the doctor, instead of the treatment you expected, advises you to move more, stay outdoors and control this situation.? Sometimes medications are prescribed, but their effectiveness has not been proven. Considering that with age the pulse should physiologically become less frequent, a child with bradycardia may experience a pathological decrease in pulse rate, which should not be missed.
Children with a low pulse often experience headaches, dizziness, increased fatigue, and poor tolerance to physical activity. The boundaries of moderate and severe bradycardia are presented in Table N2. NB! : Fainting (syncope) or presyncope (presyncope) is a reason to immediately seek medical help. Most of these situations, especially in adolescence, are not dangerous, but there are a number of pathological conditions that require immediate treatment.
Table N2. Interpretation of changes in heart rate (beats/min) in children 5-18 years old (protocol TsSSSA FMBA of Russia) A few words about the modern capabilities of instrumental pulse recording: 1. The standard ECG, known to everyone, is limited to 30-40 seconds of recording, but due to the simplicity and accessibility is indispensable in this matter. 2. Daily (Holter) monitoring (HM) ECG provides information about each heartbeat during the day, its variability during sleep and wakefulness, stress and rest. At the same time, an observation diary is kept and, if it is sufficiently informative, it is possible to prove or reject the connection of complaints with changes in the ECG. This is the “gold standard” for diagnosing heart rhythm and conduction disorders at any age, starting from birth. It is very important to know that the norms determined at rest differ significantly from the norms for daily monitoring, since a larger range of changes is allowed per day. I will not cite them, since they are the domain of specialists. 3. External monitors, so-called Event recorders, can be attached to the surface of the body for 7 to 28 days, and to register an ECG it is necessary to press a button when there are symptoms. 4. Reveal - a device implanted under the skin, resembling a flash drive - is used if there are threatening symptoms, but nothing can be registered on the HM ECG. Such a device can remain under the skin for up to two years.
When recording a rare pulse on an ECG, it is useful to conduct a test with physical activity, when the ECG is recorded at rest (lying down), after a load of 30 squats for 20 seconds) and 3 minutes after the load. A simple but very informative test: if the pulse increases adequately to the load, is restored in a timely manner and there are no pathological changes on the ECG, then, as a rule, there is no cause for concern. The load test can also be carried out using special devices - treadmill test, bicycle ergometer, etc.
The article was prepared by medical cardiologist N.N. Konopko.
Case from practice
I will give an example from my own experience.
A mother and her 14-year-old child came to see me. Recently, the mother noticed that her daughter became slow, sleepy and lethargic, and began to gain weight, despite her poor appetite. When I began to examine the girl, I discovered a decrease in heart rate to 52 beats per minute, swelling of the face, legs and arms, and an enlargement of the thyroid gland. I ordered an electrocardiogram, an analysis of thyroid hormones, antibodies and an ultrasound examination of the thyroid gland. The results showed sinus bradycardia, increased levels of TSH and thyroglobulin antibodies, and decreased free thyroxine (T4). The diagnosis was made: “Autoimmune thyroiditis (Hashimoto’s), stage of hypothyroidism.” Hormone replacement therapy with L-thyroxine was prescribed. Some time after the start of treatment, the girl became more energetic, swelling disappeared, and her weight and heart rate returned to normal. Recommendations are given to regularly donate blood for thyroid hormones to monitor the effectiveness of therapy.
Clinical picture
Mild bradycardia (45–55 beats per minute), which does not cause significant disturbances in the body, is usually not accompanied by clinical manifestations. Symptoms such as dizziness, weakness and fainting occur when the heart rate drops to 40 beats per minute.
In addition, when the heart rate slows down, you may experience:
- chronic fatigue;
- dyspnea;
- cold sweat;
- chest pain;
- blood pressure surges;
- problems with attention, thinking and memory;
- flashing “flies” before the eyes.
In severe cases, fainting and episodes of loss of consciousness are possible. The severity of bradycardia symptoms depends on the degree of circulatory disorder developing against its background.