What kind of disease is this and what are its causes?
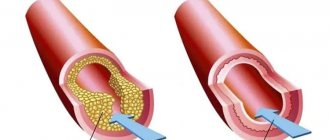
The main etiological cause of the development of acute myocardial infarction is atherosclerotic damage to the intima (inner lining) of the coronary arteries.
As a result of the formation of deposits, the lumen of the vessel narrows, and blood begins to flow in limited quantities. This is how IHD begins with angina attacks. When exposed to provoking factors (physical or emotional stress), the artery is completely blocked and permanent ischemia develops with the formation of an area of necrosis. Other (very rare) causes of heart attack are conditions in which blood flow is disrupted:
- rheumatism;
- vasculitis;
- tumors;
- allergy;
During my practice, I often encountered the fact that many patients do not eliminate bad habits and poor nutrition from their lifestyle. But these risk factors for myocardial infarction often lead to fatal consequences.
Deterioration of the blood supply to the heart occurs more often in the elderly: men after 45 years of age and women after 55 years of age should beware of the disease. Psycho-emotional shocks can provoke an attack - many patients come to our department after the death of loved ones, dismissal from work, divorce.
Only in hospital
Acute coronary syndrome is a collective concept that includes unstable angina and acute myocardial infarction. The treatment strategy for this condition is to quickly restore blood flow, which saves the myocardium and the life of the patient. And such assistance can only be provided in a hospital or vascular center, provided that the patient is delivered within two hours from the moment the vessel is blocked. Statistics confirm this: mortality in hospitals from myocardial infarction is 13–14%, in vascular centers – even lower.
Correct routing of patients and stenting are a real opportunity to reduce mortality from heart attacks, Maria Glezer emphasized. According to her, the introduction of a system of vascular centers made it possible to reduce hospital mortality from acute heart attack in the Moscow region by 60% - an impressive figure. But the problem is that people don't call an ambulance. 40–50% of patients die at home, Maria Glezer laments: “When I ask why they were sitting at home, they answer: they thought it would go away on its own, it would resolve.” So one of the main tasks is the education of the population.
Repeated myocardial infarction is a real threat. It ranges from 10 to 20%. It is very important for people who have suffered it to be told about secondary prevention measures that can prevent rhythm disturbances and the development of such a serious pathology as heart failure, which often leads to death, says Professor Glezer.
“If the patient is lucky and survives the first time, he will not necessarily survive the second or third time,” warns the deputy director for scientific work of the medical research and educational center of Moscow State University. Lomonosov, member of the Presidium of the Russian Cardiological Society, corresponding member of the Russian Academy of Sciences, Professor Simon Matskeplishvili . “But, unfortunately, it very often happens that doctors did everything in their power to save the patient’s life: they performed primary coronary intervention, placed a stent and eliminated the cause of acute coronary syndrome or treated it conservatively. And upon discharge, they gave instructions that were designed to preserve the life and health of the patient. But, after being discharged from the hospital, he goes to the clinic, where his treatment is completely changed.”
It often happens that patients take their own medications off, and instead of really effective drugs prescribed in the hospital, they ask the doctor at the clinic to prescribe drugs from a very limited list of subsidized medications. Or worse, they switch to dietary supplements.
Heart attack is inherited. Why the heart stops in young people Read more
Classification
Classification of myocardial infarction is carried out according to several principles.
Based on the time of occurrence, they are distinguished:
- first appeared (primary);
- recurrent (repeated within 1.5 months after the first);
- repeated (occurring later than 6 weeks after the primary).
The following types of myocardial infarction are determined by location:
- left ventricle (anterior, posterior, lateral and septal walls);
- extensive, affecting several departments at once;
- right ventricle (occurs extremely rarely, often accompanied by damage to other areas of the heart muscle).
According to the degree of prevalence of ischemia and necrosis, there are the following types of acute myocardial infarction:
- intramural (located deep in the wall of the organ);
- subendocardial (develops in the inner layer);
- transmural (passes through all three layers of the heart);
- subepicardial (disorder in the outer part of the organ).
How many heart attacks can a person have?
Almost all patients who have had a heart attack once ask me about the risk of another at their appointment. Understanding their concerns very well, I will still say that no specialist will give a definite answer in this case. It is necessary to take into account the location of the scar, the depth and width of the lesion, and the presence of complications. The degree of restoration of cardiac function depends on the development of collateral circulation (additional vascular pathways). I have seen cases where the patient remained alive after the fifth episode, although death can also occur as a result of a primary heart attack.
Stages of disease development
The clinical course of a heart attack goes through five main periods:
- Subromal or pre-infarction. It can be short (up to several hours or days) or quite long (1-2 weeks or a month). At this time, pain attacks become more frequent and prolonged. The same option includes a heart attack, which manifests itself against the background of sudden and rapidly progressing angina.
- The sharpest. Consists of persistent ischemia followed by the development of necrosis. Lasts from 20-30 minutes to 2 hours (but no more). Anginal pain by this time becomes weaker or completely disappears. Blood pressure drops, signs of heart failure appear or increase.
- Spicy. Necrosis smoothly progresses into melting of the heart tissue (can last from two days to two weeks).
- Subacute (from 1 to 45 days from the onset of the episode). At this stage, the formation of connective tissue in the affected area begins, and the remaining myocardiocytes adapt to continue further work.
- Post-infarction. The scar is completely organized, granulations appear at the site of necrosis. It takes from the beginning of the acute stage from 1.5 months to six months.
I would like to draw your attention to the fact that the provision of qualified assistance during the deterioration of angina pectoris or during the acute period of myocardial infarction helps prevent the development of necrosis. In this case, the process is reversible and the prognosis is favorable.
Read more about what happens and how to act correctly at each of the above stages of a heart attack here.
Early signs of a heart attack
Most of the patients (approximately 60 to 80%) who were observed by me with this diagnosis indicate that the disease did not begin suddenly in them. It was preceded by precursors of a heart attack, or a prodromal period. The most favorable outcome was observed in those patients who sought help or were brought by the team in the first hours of the attack.
I would like to make a small disclaimer - early signs of myocardial infarction do not always occur, it all depends on the pain threshold and the state of the patient’s nervous system.
But in most cases I have seen the following symptoms:
- Pain along the anterior surface of the chest radiating to the left arm, part of the lower jaw, and scapula.
- The unpleasant sensation is not relieved by taking nitro-containing drugs and goes away only after the administration of narcotic analgesics.
- It has a constant, increasing or wave-like character with periods of subsidence and resumption.
- Lasts more than 20-30 minutes.
- The patient begins to sweat and tries to sit down or lie down as high as possible. This position makes the attack a little easier.
- Shortness of breath develops, the skin becomes pale, and the nasolabial triangle turns blue.
- When it comes to the first signs of myocardial infarction, rhythm disturbances cannot be ignored. According to my observations, they are observed in 90% of cases at the stage of ischemia development and before scar formation.
Any suspicion of a heart attack requires an immediate ECG, which will reveal all signs of ischemia, and at a later stage, necrosis and scar formation. Read more about what changes will be visible on film here.
The patient no longer fears a heart attack
“It is very important that the doctor conveys to the patient what myocardial infarction is and why we are so afraid of it,” says senior researcher at the cardiology laboratory of the Federal Scientific and Clinical Center for Physicochemical Medicine of the FMBA, head of the intensive care unit at State Clinical Hospital No. 29 Moscow, Doctor of Medical Sciences Alexey Erlikh . “Myocardial infarction is now treated so skillfully that for many patients it goes unnoticed. Something hurt, they brought you to the hospital, to the linear operating room, they inserted wires in the vessel, five days later you were discharged, and soon you were already at work, forgot about your heart attack.”
Article on the topic
Help yourself. What do you need to know to save yourself from a heart attack?
It is important to understand that myocardial infarction is a disease associated with two large processes that occur in the heart - atherosclerosis and thrombosis: the growth of atherosclerotic plaques and the formation of blood clots on these plaques, says Alexey Erlikh. “After a myocardial infarction, this process, unfortunately, does not stop,” he explains. “We doctors can slow it down with medication, but every patient who has had a myocardial infarction or any coronary event, or has risk factors for it, is very likely to have another attack. Moreover, this does not depend on what kind of heart attack it was. After unstable angina or after a small myocardial infarction, the likelihood of recurrent heart attacks is even higher than after a large heart attack.”
Consequences and complications
In any period from the onset of an acute infarction to its resolution in the form of the formation of a connective tissue scar, the following complications may be observed:
- cardiogenic shock;
- heart failure;
- ventricular fibrillation;
- wall rupture due to myomalacia;
- formation of a parietal thrombus and thromboembolism;
- pericarditis.
The lethal outcome of this disease is recorded in the early stages in approximately 35% of cases. Its cause is rhythm disturbance, cardiogenic shock and acute heart failure. Later death may occur as a result of the formation of an aneurysm with rupture, thromboembolic complications, or acute pericardial tamponade.
After the acute period, the heart muscle adapts to new working conditions, but there remains a high risk of repeated episodes.
Complications of myocardial infarction
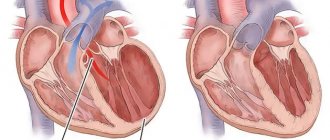
Each coronary artery sends blood to a different part of the heart muscle. The extent of muscle damage depends on the size of the area supplied by the blocked artery and the amount of time between the attack and treatment.
The heart muscle begins to repair itself soon after a heart attack. This takes about 8 weeks. As with skin wounds, a scar forms on the damaged area. But new scar tissue moves differently than healthy tissue. Thus, the heart cannot pump as much blood after a heart attack and heart failure is a complication. The extent to which this ability to pump blood is impaired depends on the size and location of the scar.
In addition, some coronary arteries supply blood to areas of the heart that regulate the heartbeat, so a heart attack sometimes causes potentially fatal abnormal heartbeats called cardiac arrhythmiasSource: Complications of Myocardial Infarction in the Elderly. Khalmukhamedov B.T. Eurasian Journal of Cardiology, 2021. p. 29-30.
Treatment
Treatment of myocardial infarction should be carried out in an intensive care unit with qualified personnel and special equipment. But assistance should begin at the prehospital stage.
This is usually done by the ambulance crew.
After taking an ECG and establishing a presumptive diagnosis, you should:
- put a Nitroglycerin tablet under your tongue;
- give 300 mg of Aspirin to drink;
- administer narcotic analgesics to eliminate pain;
- if necessary, use intravenous antiarrhythmic drugs;
- carry out resuscitation measures in case of cardiac arrest and clinical death.
Read more about how to properly provide emergency care to a patient with a heart attack here.
Drug therapy
After the patient is admitted, my colleagues and I provide care according to the established protocol. All measures are aimed at relieving pain, limiting the area of necrosis, preventing the development of complications, and restoring blood flow through the coronary arteries.
Treatment of myocardial infarction begins with the elimination of pain. Since conventional drugs are ineffective in this case, doctors use intravenous administration of the narcotic analgesics Promedol or Morphine. This helps normalize a person’s emotional state, lower the heart rate and equalize blood pressure. When discomfort is relieved, the likelihood of reflex cardiogenic shock decreases.
Acute myocardial infarction is a coronary thrombosis. Therefore, the patient is administered a direct anticoagulant, thereby performing the procedure of thrombolysis - dissolving the blood clot.
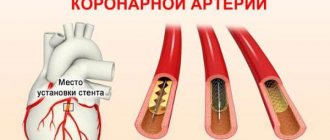
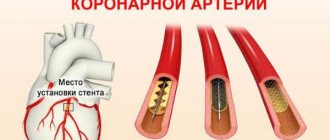
The modern and most effective approach is considered to be a stenting procedure, which allows you to instantly restore blood flow in the affected heart vessel. After this, Clopidogrel with Acetylsalicylic acid is prescribed for 2 years to prevent platelet aggregation and the development of a recurrent attack.
The use of beta blockers can reduce the load on the heart and also prevent the development of arrhythmia. Treatment of myocardial infarction necessarily includes prolonged nitrates (“Kardiket”). They allow, by dilating the coronary vessels, to improve blood flow to the heart and limit the area of necrosis.
An important point is the prescription of high doses of statins (“Rosuvastatin” up to 40 mg, “Atorvastatin” up to 80 mg) - drugs. Their use can reduce the degree of inflammatory reaction.
Symptoms of myocardial infarction and their characteristics are also taken into account during treatment. In case of severe anxiety, the patient is given sedatives; if the pressure remains high, antihypertensive drugs are used.
I would like to note that treatment after a heart attack does not end. The patient will need to take blood thinners and cholesterol-lowering drugs (statins) throughout his life. Read about how to properly undergo rehabilitation after an attack here.
Surgical methods
In the absence of treatment effectiveness and in order to prevent the recurrence of a heart attack in the same area, the following operations are used:
- Coronary artery bypass grafting. It consists of restoring the passage of blood through the heart arteries by creating an artificial anastomosis.
- Balloon angioplasty. A tube with a ball at the end is inserted into the lumen of the vessel. Having reached the point of application, it is inflated and the atherosclerotic plaque is pressed against the wall, restoring normal blood flow.
Myocardial infarction: symptoms and first aid
In the previous article, we talked about what myocardial infarction is and what are the reasons for its occurrence. I also mentioned that timely help can reduce the consequences of an attack to a minimum. And in continuation of the topic, we will dwell in more detail on the main symptoms of myocardial infarction and what should be done first if a misfortune does happen.
How to recognize myocardial infarction
But first, how do you know when it’s time to sound the alarm? It is important not so much to “not confuse” a heart attack with something else, but to realize in time that this could be exactly it. And the main symptom here is pain. It can be different - strong, burning, pressing, cutting, sometimes dull, sometimes (most often in diabetics) very weak. Usually behind the sternum, not in the area of the left nipple, but precisely behind the sternum, radiating to the left arm, neck, jaw.
Already at the prehospital stage, a serious problem can be suspected based on the location and intensity of pain. But sometimes such pain can be masked behind problems in the spine, exacerbations in the stomach. Therefore, it happens that a doctor, instead of recommending that the patient undergo a clinical minimum, which includes electrocardiography, treats pancreatitis. And only then at the autopsy they find an acute extensive myocardial infarction.
Another feature: if angina pain goes away after taking a nitroglycerin tablet under the tongue, then if the myocardium is damaged, it does not stop so easily. And if the pain continues for more than fifteen minutes, you need to urgently call an ambulance!!! Remember the “golden” first hour!
How to save
Before the ambulance arrives, you need to do the following:
1. Lay the victim down, raise the head end of the bed.
2. Give a nitroglycerin tablet under the tongue.
3. Give an aspirin tablet with milk. The victim must chew it first (or try crushing the tablet in advance).
4. In addition, sedative drops will not be superfluous for the patient...
5. ...and, possibly, an anesthetic (analgin, baralgin).
6. After this, call an ambulance as soon as possible!!! Be sure to report the assistance you have already provided.
Harmful advice from a resuscitator
Help is, of course, important and necessary, but you must remember that your lifestyle plays a major role in the development of ischemic damage to the heart muscle. How should you treat your health so as not to end up in a hospital bed and play the game? On this topic, I have prepared for you some special tips that will probably work, only... on the contrary.
Tip 1.
Eat more fatty foods, more hamburgers, only mayonnaise, butter, zhyyyrr!!! And less movement! We need to make sure that the body produces as much low-density cholesterol as possible and does not have time to process it!
Tip 2. Smoke, smoke a lot, two packs a day! So that every cigarette you smoke makes you dizzy, due to the narrowing of all blood vessels in the body. The coronaries also spasm from pleasure. Smoking is nothing better for the heart!
Tip 3.
A glass of red wine only makes your vessels cleaner due to the presence of antioxidants in it - don’t drink it! Drink surrogates, a lot of alcohol surrogates, and then the myocardium will thank you.
Tip 4.
Accumulate negative psychological energy within yourself. Don’t throw it out in sports, save it up, “digest” endlessly difficult thoughts. Constant chronic stress leads to an increase in adrenaline levels and perfectly constricts the coronary vessels!
Tip 5. The pressure is a little off the charts, but you don’t feel it? And to hell with it, live as long as fate has determined, just think - a vessel in the brain will burst, but this is a wonderful sudden death without suffering! Continue, gentlemen of hypertension, in the same spirit!
Tip 6.
Harmful relatives dragged you to the doctor, and he prescribed aspirin? And the doctor also mumbles that the blood needs to be thinned, and meanly hints at your forty-five-year-old age? Don't listen to him, you're still young! Listen to your neighbor, who has an ulcer because he treated the flu with this same aspirin, and it doesn’t matter that the dose of aspirin is tiny. Moreover, in the morning, blood periodically flows from your nose - this is definitely not pressure, this is liquid blood!
And the fact that in some Americas everyone swallows aspirin, let them swallow it, soon all of America will be plunged into darkness due to the explosion of a volcano in the Yellowstone Nature Reserve.
Tip 7. Electrocardiogram? Tests, some kind of cholesterol, high and low density?.. But who needs it! Stand in lines, but what good, and they ask for money, charlatans. And when you don’t know about the disease, you sleep better.
Tip 8.
Everyone recommends eating sea fish, like it contains some kind of polyunsaturated fatty acids. What for? Why do you need this zhyyyyr? You can’t understand these doctors: either eat fat or don’t eat fat... So don’t touch this stinking fish! The best fish is pork in general. Eat it with lard every day!
I hope that after these “tips” you correctly understand what kind of lifestyle you need to lead in order not to meet my colleagues!
Be healthy!
Vladimir Shpinev
Photo thinkstockphotos.com
Products by topic: [product](nitroglycerin), [product](aspirin), [product](analgin), [product](baralgin), [product](tonometer)
Clinical case
A patient was admitted to the hospital with severe chest pain and other typical symptoms of myocardial infarction.
He was sent from the clinic, where a cardiogram was taken, which revealed large-focal necrosis in the acute stage of development along the anterior wall of the left ventricle. He notes that lately there have been warning signs of a heart attack - angina attacks became stronger and were poorly controlled with Nitroglycerin. The patient was referred for percutaneous coronary intervention—stenting. On the second day after the procedure, the patient felt much better, and therefore he was transferred to the general cardiology department. Recommendations were issued: follow a diet with limited fluid and salt, as well as the exclusion of fatty foods and foods high in cholesterol, lifelong use of Aspirin and statins, adequate physical rehabilitation.