Transmural myocardial infarction
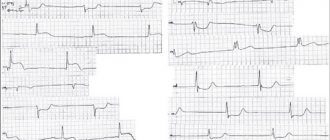
Transmural myocardial infarction means necrosis of all three layers of the heart muscle - the outer (epicardium), middle (myocardium) and inner (endocardium). Therefore, a transmural infarction is called penetrating (translated as “through-the-wall”). On an electrocardiogram with a transmural infarction, a Q-shaped wave is clearly visible. Another name for this type of myocardial infarction is associated with this - Q-infarction.
Transmural infarction is dangerous, first of all, because of its relapses. The small focal form of tissue necrosis, despite its penetrating nature, does not lead to serious complications. However, a repeated heart attack causes extensive symptoms that threaten not only the health, but also the life of a person. Large-focal infarction, in which a significant area of the heart is affected, poses a great danger even at the first attack.
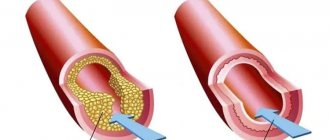
The main cause of transmural myocardial infarction is atherosclerosis of the coronary arteries. With this disease, plaques form in the walls of blood vessels, which narrow the lumen of the blood vessels, impeding blood flow and blood flow to the heart. The situation is aggravated by physical exertion and nervous stress, during which the pulse quickens and blood flow accelerates and intensifies. As a result, blood turbulence occurs at the site of atherosclerotic plaques, red blood cells stick together and blood clots form. These blood clots represent the main danger of developing a transmural infarction. Rupture of an atherosclerotic plaque or detachment of a blood clot leads to blockage of the vessel supplying the heart. Left without blood supply and oxygen supply, muscle tissue cells die - a focus of necrosis is formed.
This process is accompanied by pain in the heart area, which is the stronger the pain at the affected area. Pain during transmural myocardial infarction has a wave-like character - sometimes rolling, then receding, it can last tens of minutes, several hours and even several days. Pain in the heart during transmural infarction is acute, squeezing, radiating under the left shoulder blade, into the left arm, jaw, teeth , ear, accompanied by restlessness, anxiety, excitement, fear of death.
A feature of extensive transmural myocardial infarction is the addition of motor disorders (paralysis of the limbs), dysfunction of internal organs, difficulty speaking and other symptoms associated with impaired blood supply to the body. Other serious complications of transmural infarction are pulmonary edema and cardiac asthma.
Myocardial infarction (heart attack) - symptoms and treatment
A patient with an acute heart attack must be promptly transported to the hospital to prevent complications and increase the chances of survival. The system of care for patients with myocardial infarction includes the following stages:
- Pre-hospital stage. Ambulance teams provide assistance and transport the patient to the hospital.
- Hospital stage. Help is provided in specialized vascular departments.
- Rehabilitation stage. Rehabilitation is carried out in special departments of hospitals or specialized cardiological sanatoriums.
- Dispensary observation and outpatient treatment. Clinical examination in the post-infarction period is carried out in regional or city cardiology centers or in cardiology offices of clinics [6].
At the prehospital stage, the following tasks are solved:
- an accurate diagnosis is established. If this fails, it is permissible to establish a tentative syndromic diagnosis as soon as possible;
- The patient is given a nitroglycerin tablet under the tongue (or use a nitro-containing spray) and 0.25-0.35 g of aspirin;
- pain is relieved by administering painkillers;
- acute circulatory failure and heart rhythm disturbances are eliminated;
- the patient is brought out of the state of cardiogenic shock;
- in case of clinical death, resuscitation measures are performed;
- transport the patient to the hospital as soon as possible.
Further therapy is determined by the stage (period) of myocardial infarction. In the acute and very acute period, the goal of treatment is to prevent an increase in the focus of myocardial necrosis, eliminate pain and other symptoms. It is important to restore blood flow through the heart arteries and relieve pain. The intensity of pain during this period is so great that the patient may die due to cardiac arrest. It is necessary to prevent severe complications. When the disease passes into the subacute stage and in the post-infarction period, the goal of therapy is to reduce the risk of attack recurrence and possible complications.
For the treatment of acute myocardial infarction, drugs from various pharmacological groups are used:
Painkillers. Analgesics from the group of narcotic painkillers (morphine, promedol, omnopon) in combination with analgin, antihistamines (diphenhydramine). Neuroleptanalgesia is most effective when a combination of the analgesic fentanyl with the strong antipsychotic droperidol is used. The effectiveness of these drugs is noticeable within a few minutes. Not only pain disappears, but also fear of death, unmotivated anxiety and psychomotor agitation. Tranquilizers (diazepam) can be used to relieve psychomotor agitation. To reduce hypoxia (decreased oxygen in tissues), oxygen inhalation is used using a nasal catheter.
Thrombolytic therapy. It is important to restore blood flow and dissolve blood clots so that the death of the heart muscle does not spread further. The smaller the area of necrosis, the higher the patient’s chances of successful rehabilitation and the lower the risk of life-threatening complications. Immediate use of drugs (preferably within the first hour after an attack) allows you to achieve maximum effectiveness of treatment. A time limit of three hours is allowed. To dissolve a blood clot, thrombolytic drugs are administered intravenously, for example, streptokinase, urokinase, alteplase. The dose depends on the patient's weight.
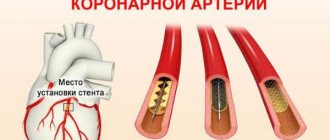
Restoration of coronary blood flow is also possible with the help of surgical treatment - stenting or coronary artery bypass grafting. A balloon catheter is inserted into a narrow section of the artery under fluoroscopic guidance. In this case, the atherosclerotic plaque is “crushed”, and the lumen of the heart artery increases. Then a stent (metal frame) can be installed into the lumen of the vessel.
Antiplatelet agents. Drugs from this group affect blood cells (platelets and red blood cells). The action of antiplatelet agents prevents platelet aggregation, improving blood flow. The main drug used is aspirin (acetylsalicylic acid). Contraindications to the use of aspirin: bleeding from the gastrointestinal tract, exacerbation of gastric or duodenal ulcers.
P2Y12 platelet receptor inhibitors are also used , which block platelet activation. The main blockers are ticagrelor, prasugrel and clopidogrel.
Intravenous/subcutaneous anticoagulants. , unfractionated heparin intravenously, is used to prevent deep vein thrombosis (DVT) and pulmonary embolism (PE) . Enoxaparin , which is also used to prevent venous thromboembolism, is administered subcutaneously.
To limit the area of myocardial ischemia and necrosis, it is necessary, in addition to restoring blood flow in the arteries of the heart, to reduce the hemodynamic load on the heart. Nitrates and beta blockers are used for this purpose.
Nitrates. They have an analgesic effect, reduce myocardial oxygen demand, increase coronary and collateral (bypass) blood flow, reduce the load on the heart muscle, and limit the size of the myocardial lesion. Their combination with beta blockers is especially effective, leading to rapid positive ECG dynamics and reducing the risk of sudden death [10].
Beta-blockers have an antiarrhythmic effect. The purpose of using beta-blockers (propranolol, metoprolol, atenolol) is to reduce the frequency and force of heart contractions, which will help reduce the load on the heart and the myocardial oxygen demand. Beta blockers continue to be used indefinitely in the absence of side effects and contraindications [1].
Myocardial infarction of the posterior wall of the left ventricle
Myocardial infarction of the posterior wall is more difficult to diagnose electrocardiographically than myocardial infarction of the anterior wall.
According to ECG and autopsy comparisons, almost half of these infarctions are not visible on the ECG. The posterior wall of the left ventricle is conventionally divided into 2 parts:
- the diaphragmatic part of the posterior wall, - the basal part of the posterior wall.
Posterior phrenic (posterior) myocardial infarction.
The signs characteristic of such a heart attack are determined in the III standard, aVF and are usually supported by the II standard lead.
The Q wave in leads III and aVF is considered pathological if it exceeds 1/2 of the R wave and is wider than 0.03 s. In transmural infarction, QS is usually recorded in leads III and aVF. The pathological Q wave III, aVF is usually combined with a reduced R in these leads and with characteristic changes in ST and T. Since the Q wave in standard lead III can be present even in healthy people, the pathological Q III during a heart attack is necessarily combined with pathological Q in aVF and a Q wave in the II standard lead, which in it should exceed 10% of the R wave. Myocardial infarction of this localization is also characterized by Q(II)>Q(I) (normally QI>QII). It is also typical for cicatricial infarction that R(aVF)
In the acute stage of a posterior diaphragmatic infarction, reciprocal changes are observed in V1 - V3: ST decreases and a high positive “coronary” T wave appears, and the dynamics of ST and T in the precordial leads occurs faster than in III and aVF. ( See ECG
)
Posterobasal (basal) myocardial infarction.
This high left ventricular myocardial infarction is particularly difficult to diagnose and is often underdiagnosed. This is due to the fact that there are no direct signs in the 12 mandatory leads. For the most part, the diagnosis of posterobasal myocardial infarction is made by reciprocal changes in the electrocardiogram.
Sometimes direct signs of infarction of the basal parts of the posterior wall can be detected in additional chest leads V7 - V9, in the dorsal lead along the Sky. In these leads, a pathological Q wave with typical ST and T dynamics can be recorded. Reciprocal changes are recorded in leads V1 - V3.
The most specific changes are:
— increase in the amplitude of V1 and V2, with R(V1) > S(V1), — decrease in the depth of the teeth S(V1) and S(V2), — R/S ratio in V1, V2 >= 1.0?
- widening of the initial R(V1), when R(V1)>= 0.04 s., - notching of R (V1-2), reminiscent of incomplete blockade of the right bundle branch, - decrease in ST (V1-2) in the acute phase of a heart attack with gradual reverse dynamics - the appearance in the acute phase of high positive “coronary” T waves in V1 - V3-4, and their height gradually increases. ( See ECG
).
Despite numerous indirect signs, all of them may be absent in cases of known basal myocardial infarction.
Often, changes in posterobasal infarction must be differentiated from electrocardiographic signs of right ventricular hypertrophy. Unlike a heart attack, with right ventricular hypertrophy there are characteristic changes in the left precordial leads.
Features of acute myocardial infarction and its symptoms
Acute myocardial infarction is the death of a section of the heart muscle caused by a circulatory disorder. Heart attack is one of the main causes of disability and mortality among adults.
Causes and mechanisms of vascular incompetence of the heart
A heart attack can be considered an acute form of coronary heart disease or its complication.
The peculiarities of the heart - constant contractions of the myocardium - determine a very high level of metabolic processes in its cells, high consumption of oxygen and nutrients. This mode of activity requires an uninterrupted flow of highly oxygenated (oxygen-rich) blood, which is provided by an extensive network of cardiac vessels starting from the aorta in the form of coronary (coronary) arteries.
The downside to the effectiveness of the heart muscle is its high sensitivity to oxygen starvation. If there is a malnutrition in the myocardium, pathological phenomena develop that very quickly become irreversible.
If the lack of blood flow is not critical, reversible ischemia (anemia) of the heart muscle occurs, which is manifested by anginal pain in the chest. When the flow of blood to a certain area is completely stopped, a cascade of pathological processes develops - the accumulation of toxic metabolic products that are not excreted, the transition to an anaerobic (oxygen-free) mode of operation using the internal energy reserves of cells.
The body's own reserves of energy carriers (glucose and ATP) are very quickly (in about 20 minutes) depleted, and the bloodless section of the heart muscle dies. This is myocardial infarction - necrosis, the size of which depends on the level of vessel occlusion (large or small branch), the rate of onset of ischemia (with gradual cessation of blood supply, partial adaptation is possible), the patient’s age and many other factors. For example, acute transmural myocardial infarction (with necrosis of the entire thickness of the heart muscle), which has a very severe course, develops when a large branch of a coronary vessel is occluded (blocked).
Among the causes of impaired blood supply to the myocardium, the most common is a block of the lumen of the vessel by an atherosclerotic plaque or thrombus (these phenomena can be combined) . In addition, a sharp spasm of the coronary arteries is possible under the influence of physical (cold) or chemical (poisons, drugs) factors. Severe anemia, in which there is a sharp decrease in the content of hemoglobin in the blood, and, consequently, its ability to transport oxygen, can also cause myocardial ischemia. Inconsistency of blood supply with increased needs occurs with sudden hypertrophy of the heart muscle - cardiomyopathy.
Predisposing factors for the development of heart attack
Some diseases and pathological conditions are increased risk factors for the development of acute myocardial ischemia. These include:
- Diabetes.
- Hypertonic disease.
- Coronary heart disease (CHD), manifested by attacks of angina (especially its unstable forms).
- Increased levels of cholesterol and some fractions of lipoproteins in the blood.
- Excessive body weight.
- Smoking.
- Alcohol abuse.
- Errors in diet (high consumption of salt, animal fats).
- Cardiac arrhythmia.
- Prolonged stressful situations.
- Age over 60 years (although in recent years there has been a “rejuvenation” of heart attacks).
- Male gender (after 70 years, the number of men and women suffering from a heart attack equalizes).
Classification of ischemic myocardial injury
There are different criteria for classifying a heart attack. Some of them:
- The size of the damage zone is large-focal and small-focal.
- According to the depth of damage to the heart muscle - transmural (throughout the entire thickness of the heart wall), intramural (necrosis in the thickness of the wall), subendocardial (damage to the inner layer), subepicardial (outer layer).
- According to topography - left ventricular (anterior wall, posterior and lateral walls, interventricular septum), right ventricular.
Symptoms of a heart attack
In the development of the pathological process, several periods are distinguished, each of which has its own duration and symptoms.
The pre-infarction period can last from several minutes to months. It is characterized by an increase in the frequency of angina attacks and an increase in their intensity.
The most acute period , in which ischemia and necrosis of the heart muscle develops, lasts up to several hours. It may have a typical or atypical course.
The painful, or anginal, variant is typical (about 90% of all cases). It is characterized by high-intensity pain behind the sternum of a burning or pressing nature, which can radiate (give) to the left limbs, jaw, and neck. There may be fear of death, sweating, pale or reddened facial skin, and shortness of breath. The severity of pain depends on the size of the affected area - large-focal infarction causes more severe symptoms than small-focal infarction. The pain is not relieved by taking nitroglycerin.
Atypical variants can occur in the asthmatic type (have symptoms of an attack of bronchial asthma), abdominal (with symptoms of an acute abdomen), arrhythmic (in the form of an attack of cardiac arrhythmia), cerebral (with impaired consciousness, dizziness, paralysis, visual impairment).
The acute period lasts about 10 days. The necrosis zone is finally formed and delimited, absorption of decay products and scar formation begins. The pain syndrome disappears or decreases. Possible increase in temperature, hypotension and heart failure.
The subacute period (about two months) is the stage of scar formation and thickening. There is no pain syndrome, the condition is gradually improving. Well-being in this period is largely determined by the nature and extent of changes that have occurred in the heart muscle.
The post-infarction period , or rehabilitation (up to six months), is characterized by the absence of clinical and laboratory signs of a heart attack (changes on the ECG remain - they will remain for life), however, in this phase, the development of heart failure, angina pectoris and recurrent heart attack is possible.
Complications of myocardial infarction
Acute myocardial ischemia, being a serious condition in itself, can be further aggravated by the addition of complications.
The most common complications:
- Heart rhythm disturbances (paroxysmal tachycardia, extrasystole, atrial fibrillation). A situation such as the appearance of ventricular fibrillation with the transition to fibrillation can cause the death of the patient.
- Heart failure is associated with a disruption in the activity of the left ventricle in pumping blood through the vessels. It can lead to pulmonary edema, cardiogenic shock and death due to a sharp drop in pressure and cessation of renal filtration.
- Pulmonary embolism can lead to pneumonia, pulmonary infarction, and death.
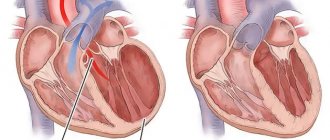
- Cardiac tamponade can occur when the heart muscle ruptures in the area of the infarction and blood leaks into the pericardial cavity. The condition is life-threatening and requires immediate attention.
- Acute cardiac aneurysm is a bulging area of scar tissue with extensive damage to the myocardium. In the future, it can cause the development of heart failure.
- Thromboendocarditis is the deposition of fibrin on the inner surface of the heart. Its separation can cause a stroke, mesenteric thrombosis (closure of a branch of the vessel feeding the intestine) with subsequent necrosis of a section of the intestine, and kidney damage.
- Post-infarction syndrome is the general name for long-term complications (pericarditis, pleurisy, arthralgia).
Diagnosis of heart attack
In the diagnosis of a heart attack, data from anamnesis (circumstances of the course of the disease and previous life, ascertained by interviewing the patient and his relatives), laboratory and instrumental research methods are important.
Anamnesis
Past attacks of chest pain of varying frequency and intensity, as well as risk factors (smoking, stress, chronic diseases) are identified. During examination, it is possible to identify excess weight, indirect signs of high blood pressure (capillary network on the face), etc. Substernal pain lasting more than 20 minutes is considered one of the diagnostic criteria for a heart attack.
Laboratory methods
Laboratory research methods for a heart attack reveal the following changes:
- Blood clinic. Leukocytosis (increased number of leukocytes), increased ESR.
- Biochemistry of blood. Increased activity of the enzymes AlT, AST, LDH, creatine kinase, myoglobin, which is an indicator of damage to the heart muscle. Changes in the level of electrolytes and iron are possible.
Instrumental research methods
- ECG – characteristic signs of a heart attack (negative T wave, pathological QRS complex, etc.). Taking a cardiogram in different leads helps determine the location of the necrotic focus (for example, the anterior or posterior wall of the left ventricle, etc.).
- EchoCG – local (limited) violation of contractility of the affected ventricle.
- Coronary angiography reveals narrowing or blockage of the vessel supplying the myocardium. It should be noted that when carrying out this research method, it can also be used to provide assistance (after supplying a contrast agent through the same catheter, a drug is injected into the vessel or an expander stent is installed).
Treatment of myocardial infarction
Emergency care (performed directly during a painful attack and then in a specialized clinic):
- Providing the patient with complete rest.
- Give sublingual (under the tongue) nitroglycerin and Corvalol orally.
- Immediate transportation for further treatment to the cardiac intensive care unit (preferably on specialized resuscitation transport).
Specialized treatment
- Relief of pain syndrome (narcotic analgesics and antipsychotics are used).
- Dissolution of a blood clot located in a coronary vessel by introducing special thrombolytic agents (streptase, cabinase). The method is very effective, but has a time limit - assistance must be provided within the first hour after the attack; subsequently, the percentage of saved myocardial mass rapidly decreases.
- Antiarrhythmic drugs.
- Improving metabolic processes in the heart muscle.
- Reducing the volume of circulating blood to reduce the load on the heart.
- Surgical methods of treatment - balloon angioplasty of the coronary vessels, insertion of a stent (tubular spacer), coronary artery bypass grafting (providing bypass blood flow by placing a shunt on the damaged vessel).
- Anticoagulants (heparin, aspirin) to reduce blood clotting and prevent thrombosis.
The prognosis for a heart attack is always serious and depends on the volume of the affected myocardium, the localization of the necrotic focus (for example, if the conduction system of the heart is involved in the area of damage, the prognosis worsens), the patient’s age, concomitant diseases, timeliness of treatment, the presence of complications, etc. The percentage of residual effects and occurrence is high. disability.
After passing the acute period, patients are shown rehabilitation with a gradual increase in the level of stress. In the future, medical supervision and prophylactic use of antianginal drugs are necessary.
Prevention of a heart attack is the cessation of bad habits, the fight against excess weight, a balanced diet, work and rest, and timely treatment in case of angina pain.