Antianginal drugs are a group of drugs that are used to treat coronary heart disease - angina and myocardial infarction.
Coronary heart disease (CHD) is a pathological condition associated with oxygen starvation of the heart muscle (myocardium) due to insufficient blood supply to the vessels of the heart.
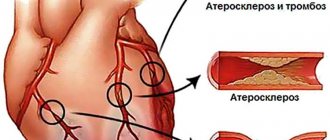
Chronic ischemic heart disease is manifested by angina pectoris. The causes of angina are usually narrowing of the lumen of the coronary (heart) vessels by atherosclerotic plaque (angina pectoris) or vasospasm (vasospastic angina).
Acute coronary heart disease is manifested by unstable angina and myocardial infarction. The cause of acute ischemic heart disease is partial or complete blockage of the lumen of blood vessels by a thrombus.
Unstable angina is considered a pre-infarction condition. Most often, it turns into an acute myocardial infarction, but if quickly recognized and treated, unstable angina can resolve quite safely.
The narrowing of the lumen of the coronary vessels leads to a decrease in the delivery of blood (and with blood, oxygen and nutrients) to the myocardium, which is manifested by oxygen starvation of the heart muscle, pain during physical activity or psycho-emotional stress.
Complete blockage of the lumen of the coronary vessels leads to a sharp lack of oxygen in the areas of the heart fed by these vessels and, in the absence of treatment, their death - necrosis.
Medicines used for angina are called antianginal drugs (from the old Latin name for angina: angina pectoris - angina pectoris).
Difficulties in risk stratification as a factor complicating the choice of therapy
It is well known that the intensity of preventive drug therapy for patients with coronary heart disease (CHD) should be directly determined by the level of cardiovascular risk.
Unfortunately, despite the many scales developed for this purpose, risk assessment for patients with coronary artery disease without a history of acute myocardial infarction (AMI) is today very difficult. In most cases, existing scales underestimate the risk level for patients in the high-risk group and overestimate it in the low-risk group [1]. The most significant practical difficulty here seems to be the impossibility of obtaining real information about the degree of stability of atherosclerotic plaques in the coronary vessels of a patient with coronary artery disease, which has primary prognostic value. Apparently, large atherosclerotic plaques that have a dense fibrous cap rupture less frequently, but at the same time cause pronounced clinical symptoms (in particular, anginal pain). At the same time, when they rupture and release a huge amount of procoagulant tissue factor into the vessel, the development of thrombotic occlusion of a large vessel is likely, the clinical equivalent of which is an extensive myocardial infarction with the formation of a Q wave [2].
Small plaques are less likely to lead to a significant decrease in coronary blood flow, which determines rarer and less intense attacks of anginal pain. But at the same time, small plaques can be much less stable; erosion or rupture of their thin fibrous cap can lead to the development of AMI, as a rule, without the formation of a Q wave (Fig. 1). As an illustrative example, we can cite the medical histories of patients with poorly compensated type 2 diabetes mellitus, who often have a history of several small focal infarctions and episodes of unstable angina.
According to new data, with unstable angina inside the coronary arteries, it is possible to form a kind of dynamic equilibrium, in which for a sufficiently long time small tears occur on the intimal surface or intimal erosions form, but the formation of a blood clot can be avoided due to the activation of the antithrombotic system. The use of methods for direct visualization of the structure of atheromas in vivo, such as optical coherence tomography/spectroscopy, makes it possible to identify such plaques [3].
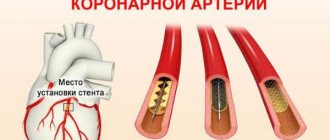
Within the framework of this concept, it is easy to explain the results of the COURAGE study (Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation), in which stenting of the coronary arteries did not lead to an improvement in prognosis, but significantly improved clinical symptoms. In all likelihood, despite the fact that anginal pain in these patients was associated with large, successfully stented plaques, the prognosis in this case was determined by small unstable plaques, the stenting of which, for obvious reasons, was not performed.
Today, assessment of the degree of stability of atherosclerotic plaques and interventions aimed at their stabilization, including through “hardening” the fibrous cap, are becoming a new paradigm in preventive cardiology. In fact, all traditional scales developed for patients with coronary artery disease solve the problem of risk assessment by analyzing factors that indirectly characterize the stability of atheromas.
New non-invasive diagnostic options
One of the main directions in the development of modern cardiology is the search for minimally invasive methods for direct or indirect assessment of the stability of atherosclerotic plaques, which will make it possible to more accurately predict the risk of developing acute coronary syndrome (ACS). Their practical application seems especially important in the management of patients with average risk, for whom the choice of optimal treatment is often difficult. Today in the West, for this purpose, the most widely used integral indicator of the scale of coronary lesions is the calcium index, which is calculated when performing multislice computed tomography (MSCT) [4].
Another approach, which can also be implemented when performing MSCT, is the assessment of the distribution of contrast density in the coronary bed, which makes it possible to determine areas of the coronary arteries with low shear stress, where unstable atheromas can be expected to form [5].
Today, more and more experimental non-invasive techniques are appearing that are designed to specifically determine the state of atherosclerotic plaques.
These include the following diagnostic methods:
• MR imaging using intravascular coils and new contrast agents (eg, ultrasmall iron oxide particles that accumulate in macrophages);
• combined technologies MSCT/MRI (magnetic resonance imaging), PET/CT (positron emission tomography/computed tomography), CT/scintigraphy;
• molecular radiation diagnostics (for example, scintigraphy with 99Tc-annexin 5, 99Tc-IL-2, with labeled platelets and low-density lipoproteins).
Among the promising biochemical markers of instability of atherosclerotic plaques are lipoprotein-associated phospholipase A2, matrix metalloproteinase 9, soluble CD40 ligand, neopterin, as well as highly sensitive C-reactive protein, which is widely available for practical determination [6].
Basic principles of pharmacotherapy
IHD is a chronic “benign” disease, and therefore the main goals of its treatment are to reduce the number, duration and severity of attacks of anginal pain and improve the prognosis, which is determined by the risk of developing cardiovascular complications such as AMI, life-threatening arrhythmias and chronic heart failure (CHF).
Currently, the effect on the prognosis of patients with coronary artery disease has been proven only for statins, angiotensin-converting enzyme inhibitors - ACE inhibitors (ramipril and perindopril), antiplatelet drugs and β-blockers (after AMI). In this review, we will focus on therapies that can primarily alleviate the condition of patients with exertional angina.
Yu.A. Karpov
Institute of Clinical Cardiology named after.
A.L. Myasnikova Federal State Budgetary Institution “Russian Cardiology Research and Production Complex” of the Ministry of Health of the Russian Federation The article discusses the issues of drug treatment of angina pectoris and provides the pharmacological features of the anti-ischemic drug ranolazine. A review of clinical studies is provided that have demonstrated the positive effect of the drug on the course of angina pectoris, good tolerability and a high safety profile.
Key words: ranolazine, exertional angina, coronary artery disease, clinical studies.
Antianginal and anti-ischemic therapy of chronic ischemic heart disease
Beta-blockers (BABs) are rightfully considered the cornerstone of the treatment of coronary artery disease. In the absence of absolute contraindications, selective β1-blockers should be prescribed without fail to all patients with a history of AMI due to their ability to increase the survival of such patients and reduce the incidence of recurrent AMI.
Cardioselective beta blockers serve as the main tool for the treatment of angina pectoris, and antianginal drugs of other groups should be used only after the potential of the beta blocker is maximally used [7].
It is extremely important to achieve target heart rate values (HR, 55–60 beats per minute), without which antianginal therapy cannot be considered optimal. If, while using beta blockers, a patient with stable angina continues to experience attacks of anginal pain, an attempt should be made to reduce the heart rate to 50 beats per minute, unless atrioventricular (AV) block develops against this background [7]. In this case, heart rate should be measured in the morning before taking the next dose of the drug.
Today, one can often find patients taking large doses of nitrates due to severe anginal pain, but not receiving optimal beta blocker therapy.
In most cases this is due to the following factors:
• unjustified fears regarding the development of side effects, which are rare (primarily various blockades and broncho-obstructive syndrome);
• the desire to prescribe a low dose of beta blocker as part of combination antianginal therapy (the real effectiveness of which may be significantly inferior to full-dose beta blocker therapy);
• difficulties in comparing dosages of different beta blockers (today doctors often use bisoprolol at a dose of 10 mg, but avoid using metoprolol at doses above 150 mg/day, and therefore patients receiving metoprolol often have a higher heart rate);
• difficulties associated with titrating beta blockers (this especially applies to the lipophilic carvedilol, which has a difficult to predict relationship between dosage and effectiveness);
In case of intolerance to beta blockers, they can be replaced with calcium channel blockers (CCBs). It should be especially noted that none of the controlled studies of CCBs showed their effect on the survival of patients with angina pectoris.
In patients with bronchial asthma, extended-release verapamil, which has a pulse-sparing effect, can be considered the drug of choice. It should be remembered that, compared with beta blockers, its use in elderly patients is associated with a higher risk of developing AV block of II–III degrees. If a significant slowdown in AV conduction occurs during the use of verapamil, Holter ECG monitoring is justified, including to exclude second-degree AV block at night.
Dihydroperidine CCBs have a weaker antianginal effect than non-dihydroperidine CCBs, but can be successfully used by patients with conduction disorders. In a number of patients, these drugs can lead to the development of subendocardial ischemia [7].
If there are contraindications to the administration of beta blockers, primarily in the presence of AV conduction blockade of the 1st degree or bronchial asthma, the If-channel inhibitor ivabradine can be used as a pulse-lowering drug. The antianginal effect of ivabradine is realized only due to a decrease in heart rate, which is why it is “in strength” inferior to beta blockers, which have a multifaceted mechanism of anti-ischemic and cardioprotective actions. It should be noted that in a large clinical trial that included more than 10 thousand patients with coronary artery disease and heart failure, ivabradine did not show an effect on cardiovascular mortality and the frequency of hospitalizations caused by AMI and heart failure [8].
results
The formed 2 groups of patients turned out to be well balanced according to a number of indicators (Table 1).
Table 1. Baseline demographics, clinical characteristics, and FN results of patients randomized to trimetazidine or ivabradine. Note. Here and in the table. 2: data are presented as M±SD or absolute number of patients (%). ACE - angiotensin-converting enzyme; ARBs—angiotensin II receptor blockers; BP - blood pressure.
The mean doses of ivabradine that achieved target resting heart rate when added to low-dose bisoprolol were 6.2 ± 1.8 and 6.0 ± 2.2 mg in the trimetazidine and ivabradine groups, respectively.
After 6 months of three-component AAT, there was a significant improvement in exercise tolerance in patients of both groups. Thus, the total duration of the load increased by 65.4±102.7 s ( p
<0.001) in the trimetazidine group and by 60.3±98.9 s (
p
<0.001) in the ranolazine group, the time before the onset of angina pectoris - by 63.8±105.5 (
p
<0.001) and 61.7±103, 0 (
p
<0.001) s, time to depression
of ST
by 1 mm - by 77.0 ± 111.8 (
p
<0.001) and 74.2 ± 108.5 (
p
<0.001) s, respectively (differences between groups are not significant ). The frequency of angina attacks was significantly reduced from 2.2 ± 3.5 to 0.8 ± 2.4 attacks per week when using a combination of drugs that included trimetazidine, and from 2.0 ± 2.4 to 0.9 ± 2.3 - combination that included ranolazine (the difference between the groups was not significant). Moreover, the addition of trimetazidine or ranolazine to therapy was not accompanied by significant changes in resting heart rate and blood pressure.
The dynamics of the main indicators of HM-ECG, EchoCG, photoplethysmography and QoL against the background of compared triple AAT regimens are presented in Table. 2.
Table 2. Dynamics of indicators of HM-ECG, EchoCG, photoplethysmography and QOL during 6 months of AAT Note. ECG - electrocardiogram; LA - anteroposterior diameter of the left atrium; LA IR—left atrium volume index; EDA—LV end-diastolic size; LVEF—left ventricular ejection fraction; E/A is the ratio of the maximum speed of early diastolic filling of the LV and its filling in atrial systole; IVRT—LV isovolumic relaxation time; DT — time of slowing down of blood flow of early diastolic filling of the LV; e' is the maximum velocity of diastolic rise of the LV base in early diastole; * — p<0.05 when compared with the initial value of the indicator.
ST segment decline
decreased by more than 1 mm during the day under the influence of therapy, which included both trimetazidine and ranolazine, but to a significantly greater extent with the first method of therapy (
p
<0.001). This advantage of trimetazidine is of practical importance, since it can positively influence the prognosis of patients [9].
In both groups, there was a comparable improvement in systolic and diastolic function of the left ventricle, the structural and functional state of large arteries. Both methods of AAT provided similar statistically significant improvements in QoL on all scales of the Seattle Questionnaire.
During 6 months of controlled therapy, no deaths or development of acute coronary syndromes were registered. Visual symptoms (photopsia) associated with ivabradine were observed in 2 patients in each group. Treatment with trimetazidine was accompanied by periodic discomfort in the gastrointestinal tract (usually a feeling of heartburn) in 3 patients. Ranolazine caused dizziness in 3 and nausea in 1 patient. In no case did this drug prolong the corrected QT
more than 450 ms. All side effects of the drugs used were mild, transient in nature, and did not lead to refusal to take them.
Combined antianginal therapy
The presence of complaints of anginal pain in patients with coronary artery disease receiving first-line therapy dictates the need to add additional anti-ischemic drugs. The algorithm for their application is presented in Fig. 2.
Before initiating combination antianginal therapy, it is necessary to ensure that the target heart rate is achieved with the use of beta blockers. In case of intolerance to beta blockers, not associated with the presence of blockades, an attempt should be made to prescribe verapamil or diltiazem in monotherapy.
Adding ivabradine to a beta blocker is justified only if the heart rate with the maximum dose of beta blocker (20 mg bispoprolol or 400 mg metoprolol) exceeds 70 beats per minute or if titration of the beta blocker dose is impossible (for example, due to chronic obstructive pulmonary disease or clinically significant vascular atherosclerosis lower extremities). The use of ivabradine together with small doses of beta blockers to reduce heart rate in patients who tolerate beta blockers well, due to the lack of evidence, should be considered irrational.
If, against the background of the target heart rate, the patient continues to be bothered by anginal pain, it is optimal to prescribe a CCB as a “second” drug [11]. In some cases, long-acting nitrates/NO donors or nicorandil can also be used.
Complaints about the presence of anginal pain in patients with coronary artery disease receiving therapy with two antianginal drugs serve as a direct indication for coronary angiography with subsequent decision on the tactics of revascularization. Currently, daily combination therapy with three or more antianginal drugs can be considered justified only for those patients in whom revascularization is not possible for any reason.
Management of patients with refractory angina when revascularization is impossible
The concept of refractory angina includes the following three factors:
1. Myocardial ischemia;
2. Anginal pain;
3. Impossibility of revascularization [12].
The following categories of patients are usually considered “inappropriate” candidates for revascularization [12]:
• patients with vasospastic angina;
• patients with suspected microvascular dysfunction (with objective signs of myocardial ischemia in the absence of significant coronary artery stenosis or with normally functioning bypass grafts);
• patients with a small volume of ischemic myocardium, when it is impossible to perform angioplasty (for example, with a hemodynamically significant symptom-related distal single-vessel lesion), stratified into the low-risk group;
• patients with diffuse, “thread-like” coronary atherosclerosis (typically damage to two or more coronary arteries, involving the distal bed with arteries < 1 mm in diameter);
• persons with a very high perioperative risk (due to severe concomitant diseases, this group often includes elderly people with multi-vessel disease).
It must be emphasized that the conclusion about the impossibility of revascularization should be made by a multidisciplinary team and this status can be revised taking into account changes in the patient’s condition and the possibility of attracting an experienced surgical team capable of operating on high-risk patients.
Next, we will consider drugs that can be used in “maximized” antianginal therapy regimens for such patients.
One of the highly effective antianginal drugs is nicorandil, an activator of ATP-dependent potassium channels in the plasma and mitochondrial membranes with nitrate-like properties. Usually, nicorandil is used in cases of intolerance to beta blockers and cCBs, but it can also be used as part of combination therapy. In a double-blind study involving patients with stable angina, nicorandil was shown to lead to a significant increase in exercise capacity, time to onset of anginal pain and ST depression ≥ 1 mm [13]. In the IONA randomized clinical trial (RCT), which included more than 5000 patients with chronic ischemic heart disease, nicorandil, prescribed at a dose of 20 mg twice daily, demonstrated superiority over placebo in terms of its effect on the incidence of hospitalization, which was regarded as a reduction in the risk of developing unstable angina. In approximately a third of cases, a headache may occur in the first days after taking nicorandil [13], and there is also a risk of developing tolerance to its action.
Another promising drug is ranolazine, which partially inhibits fatty acid oxidation and blocks late sodium channels (operating in diastole). Ranolazine is able to neutralize ischemia-induced sodium and calcium “overload” of cardiomyocytes, improving perfusion and diastolic function of the myocardium. In addition, it has an antiarrhythmic effect and is able to reduce the level of glycosylated hemoglobin in patients with a combination of coronary artery disease and diabetes.
Several randomized, double-blind studies (MARISA, ERICA, CARISA) have shown that ranolazine reduces the frequency of angina episodes, nitrate intake and increases exercise tolerance without clinically significant effects on heart rate and blood pressure [14]. However, in the MERLIN TIMI 36 (Metabolic Efficiency With Ranolazine for Less Ischemia in Non-ST Elevation Acute Coronary Syndromes) study, in which patients with ACS were observed for a year, ranolazine did not show an effect on the risk of AMI and cardiovascular mortality. When treating angina in people with microvascular dysfunction, it is also possible to use drugs with analgesic properties, such as the phosphodiesterase inhibitor aminophylline, the antidepressant imipramine. Methods of psychotherapy and cardiac rehabilitation can also be used [15].
Non-drug methods that can alleviate the condition of some patients with refractory angina include enhanced external counterpulsation, shock wave therapy and electrical stimulation of the spinal cord [16]. An invasive procedure such as transmyocardial laser revascularization, according to a meta-analysis of 7 studies (n = 1137), cannot be recognized as an effective treatment for refractory angina [17].
Currently, the effectiveness of such experimental methods for treating resistant angina is being clarified, such as cell therapy and the use of growth factors that activate angiogenesis, including granulocyte-macrophage colony-stimulating factor, which can “mobilize” bone marrow stem cells to participate in coronary angiogenesis.
Literature
1. VNOK. Diagnosis and treatment of stable angina. Russian recommendations (second revision). Cardiovascular therapy and prevention (Appendix 4). 2008. 2. The Task Force on the Management of Stable Angina Pectoris of the European Society of Cardiology. Guidelines on the management of stable angina pectoris: executive summary. Eur Heart J 2006; 27: 1341–81. 3. Karpov Yu.A., Sorokin E.V. Stable coronary artery disease: strategy and tactics of treatment. 3rd ed. M.: MIA, 2012. 4. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the Diagnosis and Management of Patients with Stable Ischemic Heart Disease. Circulation 2012; 126:e354–e471. 5. Aslam S, Gray D. Ranolazine (Ranexa) in the treatment of chronic stable angina. Adv Ther 2010; 27 (4): 193–201. 6. Letienne R, Vie B, Puech A et al. Evidence that ranolazine behaves as a weak b1- and b2-adrenoceptor antagonist in the cat cardiovascular system. Naunyn Schmiedebergs. Arch Pharmacol 2001; 363(4):464–71. 7. Allely MC, Brown CM, Kenny BA et al. Modulation of alpha 1-adrenoceptors in rat left ventricle by ischaemia and acyl carnitines: Protection by ranolazine. J Cardiovasc Pharmacol 1993; 21 (6): 869–73. 8. Zhao G, Walsh E, Shryock JC et al. Antiadrenergic and hemodynamic effects of ranolazine in conscious dogs. J Cardiovasc Pharmacol 2011; 57 (6): 639–47. 9. Chaitman BR, Schettino SL, Parker JO et al. Anti-ischemic effects and long-term survival during ranolazine monotherapy in patients with chronic severe angina. J Am Coll Cardiol 2004; 43(8):1375–82. 10. Estacion M, Waxman SG, Dib-Hajj SD. Effects of ranolazine on wild-type and mutant hNav1.7 channels and on DRG neuron excitability. Mol Pain 2010; 6: 35. 11. Melloni C, Newby LK. Metabolic efficiency with ranolazine for less ischemia in non-ST elevation acute coronary syndromes (MERLIN TIMI-36) study. Expert Rev Cardiovasc Ther 2008; 6 (1): 9–16. 12. Dobesh PP, Trujillo TC. Ranolazine: A new option in the management of chronic stable angina. Pharmacotherapy 2007; 27 (12): 1659–76. 13. Siddiqui MA, Keam SJ. Ranolazine: A review of its use in chronic stable angina pectoris. Drugs 2006; 66(5):693–710. 14. Chaitman BR, Pepine CJ, Parker JO et al. Effects of ranolazine with atenolol, amlodipine, or diltiazem on exercise tolerance and angina frequency in patients with severe chronic angina: A randomized controlled trial. JAMA 2004; 291(3):309–16. 15. US Food and Drug Administration. Available from: https://www.fda. gov/ohrms/dockets/ac/03/briefing/4012B2_01_Action%20Letter.pdf. Accessed April 4, 2007. 16. Stone PH, Gratsiansky NA, Blokhin A et al. Antianginal efficacy of ranolazine when added to treatment with amlodipine: The ERICA (Efficacy of Ranolazine in Chronic Angina) trial. J Am Coll Cardiol 2006; 48(3):566–75. 17. Morrow DA, Scirica BM, Karwatowska-Prokopczuk E et al. Evaluation of a novel anti-ischemic agent in acute coronary syndromes: Design and rationale for the Metabolic Efficiency with Ranolazine for Less Ischemia in Non-ST-elevation acute coronary syndromes (MERLIN)-TIMI 36 trial. Am Heart J 2006; 151(6):e1181–e1189. 18. Arnold SV, Morrow DA, Lei Y et al. Economic impact of angina after an acute coronary syndrome: Insights from the MERLIN-TIMI 36 trial. Circ Cardiovasc Qual Outcomes 2009; 2 (4): 344–53. 19. Arnold SV, Morrow DA, Wang K et al. Effects of ranolazine on disease-specific health status and quality of life among patients with acute coronary syndromes: Results from the MERLIN-TIMI 36 randomized trial. Circ Cardiovasc Qual Outcomes 2008; 1 (2): 107–15.
Metabolic and antioxidant therapy
“Antioxidant therapy” fits harmoniously into traditional treatment regimens for coronary heart disease thanks to the use of drugs such as statins, ACE inhibitors, and carvedilol, which have a pronounced antioxidant effect. At the same time, the beneficial anti-ischemic, cardioprotective and anti-atherosclerotic effects of “pure” antioxidants (bioflavonoids, polyphenols, vitamins, glutathione, emoxypine, ethylmethylhydroxypyridine), shown in various biological models, have not currently been demonstrated in any large clinical study. Several prospective placebo-controlled RCTs have shown neutral and even negative effects of vitamins [18]. It was recently discovered that a number of experiments in which the positive effects of quercetin were shown were carried out with gross violations of biomedical ethics [19]. Thus, the use of antioxidants by patients with coronary artery disease, including as part of dietary supplements, is not justified.
Metabolic drugs also have a rather poor evidence base. In this regard, the European Agency for the Evaluation of Medicines has reduced the range of indications for the use of the drug trimetazidine, which can only be used as an additional antianginal agent in case of intolerance or insufficient effectiveness of first-line therapy [20]. Angina caused by microvascular dysfunction can be indicated as an area of rational use of trimetazidine as part of complex antianginal therapy.
In Russia, the drug meldonium, an analogue of γ-butyrobetaine, is also used in the treatment of patients with coronary artery disease. Meldonium inhibits the enzyme γ-butyrobetaine hydroxylase, which leads to a slowdown in the biosynthesis of carnitine and the transport of long-chain fatty acids across the mitochondrial membrane in vitro (at the same time, β-oxidation of fatty acids slows down, and intracellular metabolism “switches” to glycolysis). The drug L-carnitine has the opposite effect, accelerating the transport of long-chain fatty acids into mitochondria, the β-oxidation of which is much more energetically beneficial, but also requires larger amounts of oxygen. The question of which of these strategies can be considered optimal in clinical practice, when long-term chronic myocardial ischemia can give way to acute with the development of ACS, remains open.
Drugs with metabolic effects (Fig. 5)
Of the drugs of this class available in the world, studied in authoritative studies (trimetazidine, ranolazine, perhexiline), only the first is available in our country (preference is given to the retard (MR) form). Trimetazidine inhibits fatty acid oxidation and switches myocardial metabolism to glucose oxidation, increasing ATP production by approximately 30%.
Optimizing energy metabolism under conditions of oxygen deficiency has a beneficial effect on cardiomyocyte metabolism, improving myocardial functions (primarily contractile). In a number of studies, trimetazidine had an effect in reducing the severity of anginal syndrome and improving exercise tolerance in patients with stable angina. The anti-ischemic efficacy of trimetazidine in small studies was comparable to that of beta blockers. The effect of trimetazidine on prognosis has not been studied in large randomized controlled trials; in several relatively small studies, data on the positive effect of trimetazidine on prognosis in chronic ischemic heart disease, as well as in chronic heart failure, have been quite convincingly demonstrated.
One interesting approach is the use of trimetazidine as an antianginal drug instead of nitrates in those patients who are taking phosphodiesterase-5 inhibitors to treat concomitant erectile dysfunction or pulmonary hypertension (nitrates are strictly contraindicated in such patients).
The antianginal effect of trimetazidine persists as long as the patient takes treatment; discontinuation of the drug leads to the disappearance of the anti-ischemic effect and positive effect on metabolic processes in the cardiomyocyte. In order to achieve stable control of angina pectoris, long-term use of trimetazidine MR is justified .
Thus, to treat a patient with stable angina, a doctor today has a fairly wide selection of modern effective medications (if necessary, most of them can be used in various combinations). Their qualified use in many cases allows for adequate control of anginal syndrome.