Coronary heart disease (CHD), along with cancer, is not only a medical, but also a social problem. Massive studies of the 20th century made it possible to identify risk factors for coronary artery disease. These include heredity, age, excess body weight, physical inactivity, hypertension, diabetes and male gender. Among all the risk factors, there are avoidable ones, such as smoking, and irreparable ones.
Prevention of coronary heart disease can be primary and secondary. Primary prevention of coronary heart disease refers to the prevention of the occurrence and development of risk factors for diseases in people without clinical manifestations. Secondary prevention is aimed at eliminating risk factors that, under certain conditions, can lead to exacerbation or relapse of existing ischemic heart disease.
When to start prevention of coronary artery disease
Reasons for development
diseases can be divided into three categories.
Persons included in at least one of these groups should especially carefully monitor their health
and regularly see a doctor.
Risk factors for developing coronary artery disease
- Biological: elderly and advanced age, gender of the person (men are more predisposed to ischemia).
- Biochemical and physiological: dyslipidemia (impaired fat metabolism), hypertension, obesity, diabetes mellitus and impaired glucose tolerance.
- Behavioral: smoking, addiction to alcohol, poor diet, physical inactivity, exposure to stress.
Most often, early ischemic
changes in blood vessels appear due to behavioral factors - poor nutrition, bad habits and physical inactivity (decreased physical activity).
Therefore, the earlier a set of
special preventive measures is started, the greater the likelihood of reducing the risk of serious pathology of the heart and blood vessels to a minimum.
The most reliable prevention of ischemia is a healthy lifestyle
Primary prevention of coronary artery disease
is a list of rules, the totality of which is called a healthy lifestyle. They are recommended to be followed not only by people at risk, but by any person. These are simple and effective measures to help avoid problems with the heart and blood vessels.
Secondary
called
prevention
, which is aimed at reducing the risk of
developing
complications of an existing disease. These measures should be implemented from the moment of diagnosis, regardless of age.
Particularly carefully and to the primary
, and
secondary prevention
should be applied to people over 40 years of age - as part of monitoring the condition of the cardiovascular system.
PREVENTION OF CORONARY HEART DISEASE, RECOMMENDATIONS FOR THE PATIENT
In recent years, there has been a cessation of growth and even a slight decrease in the mortality rate of the Russian population, but in general its level continues to remain one of the highest in Europe and still significantly exceeds the mortality rate in Russia in the early 90s.
Of particular concern is the increase in premature mortality among the working age population . There has been a significant increase in mortality from cardiovascular diseases (CVD), the share of which in the structure of premature mortality increased in men from 53 to 61%, and in women from 61 to 70%. According to experts, the main reason for such a significant increase in these indicators remains coronary heart disease (CHD) and cerebrovascular accidents. Positive changes in the current situation can only be expected if the system of disease prevention and health promotion is activated.
Features of medical prevention of diseases
In the complex of government and medical measures aimed at the primary prevention of CVD, special emphasis should be placed on a component that is closely dependent on medical measures.
It is necessary to distinguish medical preventive intervention when carrying out a set of measures for primary prevention from therapeutic measures ; it is necessary to attract the attention of the “patient” to his health as much as possible, without developing in him a fear of the disease.
Drug prevention of cardiovascular diseases is usually carried out in addition to the maximum possible number of non-drug measures. As a rule, drug prevention means:
- Antihypertensive therapy (use of drugs aimed at achieving target (optimal) blood pressure values - correction of arterial hypertension );
- Lipid-lowering therapy (reducing the level of total blood cholesterol and its fractions in case of an increase in their number - correction of hypercholesterolemia );
- Antiplatelet and anticoagulant therapy (the use of drugs aimed at reducing the risk of thromboembolic complications in individuals at high risk of the latter);
- Anti-ischemic therapy (aimed at improving blood supply and metabolic processes in the heart muscle, in areas at risk of developing damage, including recurrent damage);
- Hypoglycemic therapy (aimed at reducing to target values and monitoring the state of carbohydrate metabolism).
Non-drug prevention of cardiovascular diseases is the first stage of any preventive measures. In English-language literature, synonyms for non-drug prevention are “changes in life habits”, “changes in lifestyle”:
- Complete smoking cessation
- Losing excess weight
- Diet
- Expanding physical activity through dynamic exercise
Each of the listed types of drug treatment has its own strict indications and contraindications and should be prescribed within the framework of developed algorithms, but at the same time strictly individually. Only this approach will ensure the expected effectiveness of preventing cardiovascular diseases and their complications. For example, antihypertensive drugs are prescribed only for arterial hypertension, anti-ischemic drugs are prescribed only for proven coronary artery disease.
The required volume of medical measures for primary prevention of diseases
Primary prevention of diseases is a very difficult matter, both because of its labor intensity and because the result is intangible. Evidence of this can be obtained from the analysis of prevention programs carried out in Russia. Thus, in a program of multifactorial prevention of coronary heart disease, carried out in Moscow on the basis of one of the territorial clinics for five years, it was shown that the effectiveness of risk factor correction in people who did not have symptoms of major CVDs (in particular coronary heart disease) in relation to mortality from these diseases is detected only in the fourth or fifth year. However, the same study showed that a decrease in mortality from CVD was observed only in those individuals who managed to reduce the levels of the main risk factors: convince them to quit smoking, normalize blood pressure and total cholesterol (TC) levels, reduce lipoprotein cholesterol levels low density (LDL cholesterol), etc. That is, the correction of risk factors under the influence of a complex of medical measures for primary prevention was accompanied by a decrease in mortality in this population group.
The most complete identification of patients and persons with risk factors is, of course, only possible through preventive examinations of the population. Thanks to these measures, already at the pre-medical stage, with the help of a short questionnaire about habits, as well as by measuring blood pressure, height and body weight, people with the three main risk factors can be identified.
In addition, additional examination methods, such as blood tests for lipid levels (at least total cholesterol, and most appropriately HDL-C and triglycerides), will more fully identify risk groups for the development of CVD.
According to mass preventive surveys of the working population, it has been established that only about 1/5 of the adult population does not have risk factors.
More than half (56%) of the working age population has certain risk factors, and in half of the people in this group, risk factors occur in various combinations, as a result of which the total risk of the disease increases significantly. This category of people needs not only general information on a healthy lifestyle, but also individual advice from a doctor.
The importance of primary disease prevention increases in individuals with a hereditary predisposition to hereditary non-communicable diseases, especially in those who have risk factors.
1. Arterial hypertension.
WHO recommendations contain a detailed division by blood pressure levels:
- normal blood pressure - systolic blood pressure (SBP) below 140 and/or diastolic blood pressure (DBP) below 90 mmHg. Art.;
- optimal blood pressure is SBP 120/80 mm Hg. Art.;
- high normal blood pressure - SBP 140-160 and/or DBP 90-95 mm Hg. Art.;
- moderate and severe hypertension - SBP above 180 and/or DBP above 105 mmHg. Art.;
- isolated systolic hypertension - SBP above 140 and DBP below 90 mm Hg. Art.;
- borderline isolated hypertension - SBP 140-160 and DBP below 90 mm Hg. Art.
What should be the specific activities for primary disease prevention and promotion?
As already noted, the risk of developing coronary artery disease increases in proportion to the number of risk factors, but among several dozen, three main risk factors are distinguished: arterial hypertension, smoking and hypercholesterolemia (lipid metabolism disorder). A special place is occupied by arterial hypertension, which is important not only as a risk factor for coronary artery disease, but also as an independent pathological condition that is life-threatening.
Based on the recommendations of the working group of the European Society of Cardiology, the Society for the Fight against Atherosclerosis and Hypertension, differentiated tactics should be followed in relation to the value of blood pressure:
If at the first measurement the blood pressure level is below 140/90 mmHg. Art., then in case of a high total risk of CVD, it is recommended to repeat the blood pressure measurement once a year; if the total risk of CVD is low, repeat blood pressure measurements once every three years;
If, with two measurements, the blood pressure level reaches 140-180 and/or 90-105 mm Hg. Art. - repeat measurements at least twice within four weeks. If blood pressure remains at the same level, treat with non-drug methods. If these measures are unsuccessful during the first three months, begin treatment with medications.
If, with two measurements taken at different times, blood pressure reaches 180 and/or 105 mmHg. Art. and above, treatment should be started with both medicinal and non-medicinal methods.
Middle-aged patients in whom hypertension is detected during a preventive examination, in most cases, can be diagnosed using methods available in the clinic, and in people over 40 years of age, the overwhelming majority of the cause of increased blood pressure is hypertension (for example, in men 40-59 years old, the cause of increased blood pressure 86% had hypertension, 7% had symptomatic hypertension).
| Preventive intervention needs to begin: If even once the blood pressure reaches 160/95 mm Hg. Art. and higher, or a history of arterial hypertension is detected in persons taking antihypertensive drugs at the time of examination, regardless of the recorded blood pressure level If Quetelet’s body mass index is 29.9 or more (Body mass index (BMI) = body weight (kg) / height (m) 2, 18.5 – 24.9 is normal, 25 – 29.9 is pre-obese, over 30.0 – obesity) If the level of total fasting blood cholesterol is 250 mg/dl or 6.5 mmol/l or more; triglyceride (TG) levels reach 200 mg/dL or 2.3 mmol/L or more; HDL cholesterol levels fall to 39 mg/dL or 1 mmol/L or lower in men and 43 mg/dL or 1.1 mmol/L or lower in women With regular smoking, even one cigarette per day With low physical activity - that is, when more than half of the working time is spent sitting, and at leisure walking, lifting weights, etc. take less than 10 hours a week |
In patients with hypertension, excess body weight is three times more common than among healthy people, and dyslipoproteinemia (hyperlipidemia) is twice as common.
2. Hypercholesterolemia
According to the level, hypercholesterolemia is divided into: mild - 5-6.5 mmol/l; moderate - 6.5-8 mmol/l; pronounced - above 8 mmol/l.
(non-drug correction methods are outlined below in the diet therapy section)
Almost half of the patients smoke, many are not physically active enough. Hypertension is more common in people who drink alcohol daily or several times a week.
Non-drug prevention
1. Smoking
The most common RISK FACTOR among the working population, especially among men, is smoking. According to WHO, smokers are more likely to develop cardiovascular, oncological (with damage to the respiratory system), and bronchopulmonary diseases. The severity of the pathology and the frequency of complications are associated not only with the fact of smoking, but also with its intensity. According to WHO experts, there are no “non-hazardous” types of tobacco products, since the range of harmful substances in tobacco smoke is so wide that measures to reduce one or two of them (for example, using special filters, etc.) generally do not reduce the danger of smoking .
The habit of smoking is a complex psychosomatic dependence, often determined by the types of smoking behavior. The doctor must patiently but persistently focus on finding an “alternative” replacement for smoking in each specific case, involving the smoker in “cooperation”, gradually leading him to the idea of the need and real possibility of quitting smoking. It is necessary to create a positive motivation for the smoker to give up this habit and convince him that quitting smoking immediately is always preferable. It is recommended to teach the patient the elements of auto-training with the introduction of special formulas (“By stopping smoking, I gave myself five to six years of a fulfilling life,” “By quitting smoking, I felt a surge of health,” etc.). Sometimes it is necessary to resort to sedative and other symptomatic therapy, and in cases of physiological dependence, to specific drug treatment.
Drug therapy for smoking can be divided into aversion and replacement. (The goal of the first is to develop an aversion to tobacco, for which various astringents are used, rinsing the mouth before lighting cigarettes, etc.) Replacement therapy allows you to relieve symptoms of nicotine withdrawal by introducing into the body substances that have an effect on the body similar to nicotine, but are deprived of its harmful properties (lobeline, cytisine), or nicotine (Nicorette chewing gum, patches, records). Auxiliary therapy (sedatives, hypnotics and other psychotropic drugs, as well as rational vitamin therapy) is prescribed to relieve neurotic disorders, sleep disorders and decreased performance, which often accompany smoking cessation.
The method of choice in the treatment of tobacco smoking in recent years is reflexology, which turns out to be very effective not only in relation to immediate smoking cessation, but also in preventing a return to smoking, which is often observed with short-term treatment methods.
Most smokers explain their reluctance to quit smoking by being afraid of gaining weight. Indeed, quitting smoking and the gradual elimination of symptoms of chronic tobacco intoxication are accompanied by an improvement in taste sensitivity, appetite, and normalization of the secretion of the digestive glands, which generally leads to an increase in food intake and, consequently, weight gain. This undesirable phenomenon for many can be avoided if you follow some simple dietary tips: avoid overeating and follow the basics of rational nutrition. A smoker’s physiological balance will be restored faster by consuming foods containing vitamin C (rose hips, black currants, green onions, cabbage, lemons, etc.), vitamin B1 (whole bread, cereals), vitamin B12 (green peas, oranges, melons) , vitamin PP (beans, cereals, yeast, cabbage, dairy products, potatoes), vitamin A (vegetables, especially carrots), vitamin E (whole bread, vegetable oil, green vegetables, wheat germ). Nicotine addiction, which is usually accompanied by “acidification” of the internal environment of the body, is reduced by alkaline drinking - mineral waters, juices, vegetable decoctions.
Particular attention should be paid to complaints that appear immediately after quitting smoking in order to promptly interrupt the patient’s formation of a cause-and-effect relationship between his condition and quitting smoking and remove the reason for returning to this bad habit. This concerns primarily the development of neurotic disorders, withdrawal symptoms, and unwanted weight gain.
A number of smokers, especially long-term smokers, experience an intensified cough with sputum production in the first time after quitting smoking. It is necessary to explain to the patient that this is a natural process, and prescribe expectorants and alkaline drinks.
The patient should be advised to avoid situations that provoke smoking. Psychological support from others and an approving attitude towards non-smoking help to consolidate the cessation of this bad habit.
2. Losing excess weight
Diet (including those aimed at reducing blood cholesterol)
Excess body weight and lipid metabolism disorders, as a rule, are closely related to incorrect habits and nutritional patterns, so their correction involves, first of all, a set of dietary recommendations, which is based on the principle of rational nutrition. People who do not control the calorie content of their diet and increase their consumption of animal fats and carbohydrates are two to three times more likely to develop excess body weight.
The most common approach to weight loss is low-calorie, nutritionally balanced diets. The degree of calorie reduction depends on excess body weight. Patients with excess body weight, when there is no clinical form of obesity yet, already need qualified dietary recommendations using psychotherapeutic approaches, since most often these individuals do not have sufficient motivation to lose weight. For people with severe excess body weight (index 29.9 or more), improving their well-being when losing weight is of greatest importance.
Principles of diet therapy
- Caloric restriction. Successful weight loss is observed under the condition of following a diet - when energy consumption per day is greater than the number of calories received from food.
- Reducing the diet of carbohydrates and fats, especially of animal origin.
- Meals until 18.00.
- Fractional meals (3-4 times a day, in small portions, food should be eaten slowly).
- The diet must be followed by all family members.
Fasting is an unacceptable method of treating obesity!
| Principles of rational nutrition Balance of energy intake and energy expenditure of the body in accordance with gender, age, nature of work Regular excess of the daily calorie content of food over energy expenditure for 200 kcal per day leads to an increase in ballast fat in the body by 10-20 g per day; over a year, body weight can increase by 3-7 kg Providing the physiological needs of the body for essential nutrients: proteins, fats, carbohydrates, vitamins, minerals For normal functioning of the body, the main nutrients must be contained in the diet in the following proportions: protein - 15% of the total calorie content (90-95 g), fat - 35% of the total calorie content (80-100 g), carbohydrates - 50% of the total calorie content (300-350 g) Diet It is advisable to eat food at least four to five times a day, distributing it according to the calorie content of the daily diet approximately as follows: breakfast before work - 30%, second breakfast - 20%, lunch - 40%, dinner - 10%. The last meal should be at least two to three hours before bedtime. The interval between dinner and breakfast should be no more than 10 hours |
Reducing the caloric content of the diet should be reduced to reducing the consumption of carbohydrates and animal fats. Daily caloric intake should be limited to 1800-2000 kcal.
Persons with clinical forms of obesity (body mass index 29.0 and above) require a more significant reduction in caloric intake: up to 1200-1800 kcal per day with the appointment of one or two fasting days (meat, cottage cheese, apple) per week. These days you should eat five to six split meals.
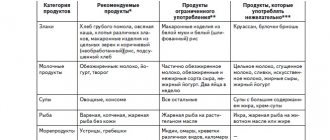
For patients with elevated levels of cholesterol in its fractions and in persons at risk of increasing it (obese, with metabolic disorders, hereditary predisposition), rationalization of nutrition should be supplemented with the following recommendations:
- Do not consume more than three egg yolks per week, including yolks used for cooking;
- limit consumption of offal (liver, kidneys), caviar, shrimp; all types of sausages, fatty hams, butter and ghee, fatty milks and dairy products;
- Replace deep frying of food with animal fats by stewing, boiling, steaming, or in the oven; before cooking, cut off visible fat from pieces of meat, and remove the skin from poultry;
- give preference to fish dishes, seafood, vegetables and risk factors;
- use low-fat varieties of dairy products, cook with vegetable oils.
If following a diet for three to six months does not lead to a decrease in the level of total cholesterol in the blood, drug therapy is recommended. In recent years, reports have appeared that lipid-lowering therapy, helping to reduce the level of atherogenic risk factors, blood lipids and the level of total cholesterol, leads to the stabilization of atherosclerotic plaques.
3. Physical activity
It has been proven that physically active leisure prevents the consequences of a sedentary lifestyle (the development of obesity, arterial hypertension, diseases of the cardiovascular system, metabolic disorders). Physical activity should be accompanied by positive psycho-emotional attitudes and not have any connotation of burden. Before starting independent studies, it is necessary to conduct a medical examination depending on the patient’s age:
- up to 30 years of age, a routine medical examination is sufficient;
- from 30 to 40 years old, a resting ECG must be added to the examination;
- over 40 years of age, it is recommended to begin training under the supervision of an instructor at a medical and physical education clinic with a preliminary test with physical activity.
For people over 40 years of age, physical activity is recommended to begin with measured walking, gradually increasing the pace and distance.
Aerobic physical activity is recommended for obese people - running, swimming, skiing, cycling. However, the most acceptable type of physical activity should be considered walking, which should be regular, moderate intensity, daily. You should start with 10 minutes a day, gradually increasing the duration of exercise to 30-40 minutes, including short (10-15 minutes) episodes of fast walking. It is recommended to devote approximately 60 minutes to physical activity daily. Fast walking is also prescribed for 30 minutes (speed - 4.5 km/h) at least 3 times a week. Short-term loads (short workouts) ensure the consumption of glycogen, and long-term ones – fat reserves. Additional physical activity - take the stairs rather than the elevator, take a 10-15 minute walk after eating. Housework is much more effective than taking a 30-minute walk 6 times a week. The effectiveness of exercise in reducing body weight increases as the duration of walking increases during the day.
Self-monitoring of the load is necessary: it should not lead to an increase in heart rate above the age limit, which is defined as “ 180 - age in years . The appearance of shortness of breath serves as a signal to reduce the intensity of the load. The training effect of the load is manifested in a decrease in heart rate at rest, a reduction in the time of heart rate recovery after a standard load (for example, 20 squats). Deterioration in well-being (sleep, appetite, performance, the appearance of unpleasant sensations) requires a reduction or cessation of exercise.
It must be emphasized that most of the recommended preventive measures are universal in nature and are indicated not only for CVD, but also for a number of chronic non-infectious diseases - chronic obstructive pulmonary diseases, some forms of malignant neoplasms, diabetes mellitus, etc.
The results of complex preventive measures determine the socio-economic and ethical significance of all preventive work. The only thing that matters is its actual implementation, the activation of reserves of practical healthcare services. And finally, it is necessary to create social conditions under which it is beneficial (both materially and morally) for a person to be healthy.
Modern opportunities for primary and secondary prevention of cardiovascular diseases (CVDs), one of the leading causes of disability and mortality in developed countries, are very high. The development of the theoretical and methodological basis of evidence-based medicine over the past decades has provided significant progress in the development and promotion among doctors and patients of scientifically based approaches to the prevention of cardiovascular diseases, as well as in the evaluation of its results
Primary prevention of coronary artery disease
Save your heart
The following rules will help keep your blood vessels healthy:
- Balanced diet. The diet should include daily consumption of fresh vegetables and fruits, as well as limiting the menu of meat products, table salt and glucose. You should completely avoid fatty, fried, smoked foods and baked goods - these products increase the content of low-density lipoproteins ("bad" cholesterol), and also provoke obesity, the constant companions of which are hypertension and atherosclerosis.
The number of thermally unprocessed vegetables and fruits in a healthy menu is not limited
- Enrichment of the diet with microelements, especially B vitamins, magnesium, potassium and iron. They regulate the heart rhythm
, improve
the condition
of blood vessels and myocardium, slow down the progression of
coronary artery disease
. The lack of microelements in the diet can also be compensated for with preparations containing magnesium, vitamins, etc. - Moderate consumption of caffeine-containing drinks - coffee and tea. Caffeine has effects on the body similar to those of adrenaline: it stimulates cardiac activity, increases blood pressure, accelerates the pulse and increases the risk of arrhythmia.
- Physical activity. Physical inactivity leads to weakened contractility hearts
and significantly increases vascular risks: the speed of blood flow in arteries and veins decreases, creating conditions for thrombus formation.
Daily morning exercises and a couple of workouts a week lasting 20-40 minutes will protect the heart
from ischemia. - Complete rest. Stress and lack of sleep deplete the body. Due to overwork and increased adrenaline and cortisol (stress hormones), normal work becomes difficult hearts
, and also increases the risk of hypertension.
- Rejection of bad habits. Smoking increases the likelihood of cardiac ischemia by 57% due to an increase in fibrinogen in the blood, a specific protein that becomes the basis for blood clots. In addition, smoking increases the level of “bad” cholesterol, leading to the development of atherosclerosis - a precursor IHD
.
Alcohol worsens the rheological properties of blood, causing thrombus formation, and also disrupts heart rhythm
and myocardial trophism. - Maintaining normal body weight. Excess weight has an extremely negative effect on the condition of both the heart and blood vessels: fat deposits in the myocardium lead to its atrophy, lipocytes “steal” oxygen from cardiac
muscles, and increased lipid levels thicken the blood and stimulate blood clots.
Primary prevention of IHD is carried out among people without clinical manifestations of the disease, that is, practically healthy. Main directions of primary prevention of coronary heart disease
include:
- organization of rational nutrition,
- lowering cholesterol and blood sugar levels,
- body weight control,
- normalization of blood pressure,
- the fight against smoking and physical inactivity, as well as
- organizing the correct daily routine and alternating work and rest.
That is, prevention is aimed at eliminating modifiable risk factors and is not only a personal, but also a national problem.
The basis of proper nutrition
The principle is that calories consumed correspond to calories burned. The approximate diet of a thirty-year-old mental worker should contain no more than 3000 kcal, with protein should be 10-15%, carbohydrates (mostly complex) - at least 55-60%. As you age, you need to reduce your calorie intake by approximately 100-150 kcal every 10 years.
Healthy eating as a preventive measure for coronary heart disease
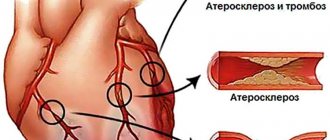
Scientists have long shown that lowering cholesterol levels
blood can lead not only to the prevention of the development of atherosclerosis and ischemic heart disease, but also to some regression of plaques already formed in the vessels.
At the initial stage, hypercholesterolemia must be combated through diet; if there is no effect, medications (statins) may be used. This is especially important for people with irreparable risk factors for developing coronary heart disease. The same goes for
normal blood glucose levels
To monitor body weight, doctors and nutritionists use an indicator called body mass index.
(BMI). This figure is obtained by dividing a person's weight in kilograms by the square of their height in meters. For example, with a height of 170 cm and a weight of 70 kg, the body mass index will be 24. Normal BMI values are in the range of 18.5-25.
Arterial hypertension is an independent risk factor for the development of coronary artery disease, therefore, at the first signs of an increase in pressure more than 140/90 mm Hg. it is necessary to contact a cardiologist to select therapy.
Smoking
- not just a bad habit. It has been established that smoking even 1 cigarette a day leads to a 2-fold increase in the risk of death from coronary heart disease. That is why so many social policy programs are aimed at combating smoking.
It is not so easy to get a young healthy man to give up, say, smoking or eating fatty foods. Not everyone thinks about the future, and IHD, which can develop in 20-30 years, is not the best motivating factor. To make it easier for the doctor to convey information about the primary prevention of coronary heart disease
to the population, special tables of the absolute risk of developing IHD have been developed. These nomograms allow us to determine the risk of developing coronary artery disease now and by age 60 years. If, according to parameters (age, gender, smoking, systolic pressure, blood cholesterol concentration), the risk of developing IHD reaches 20%, then immediate intervention and correction of risk factors is necessary.
Secondary prevention of coronary artery disease
The main areas of secondary prevention are:
- Addressing risk factors that are not necessarily the same as those considered in primary prevention.
- Drug prevention of coronary vascular spasms.
- Treatment and prevention of arrhythmias.
- Rehabilitation of patients with the help of physical training and medications.
- Surgical care for patients, if the need arises.
All of these measures are aimed at preventing repeated exacerbations of coronary artery disease, increasing the duration and quality of life, increasing working capacity and preventing sudden death of patients.
An important role is played by the patient himself, who must be an active ally of the doctor in the fight to preserve his health.
To do this, the patient is required to strictly comply with all medical recommendations, actively participate in rehabilitation plans, and timely inform the doctor about changes in his well-being. Prevention should begin in childhood
Although the first symptoms of coronary heart disease (CHD) usually appear in middle-aged and older people, atherosclerosis begins to develop in childhood. In addition, most habits, including harmful ones, leading to the emergence of risk factors for coronary artery disease, are formed already in childhood and adolescence. According to WHO, in many countries around the world children first try smoking at the age of 6-11 years. Smoking very quickly becomes a habit: by the age of 15, 40% of boys and girls already smoke, and by the age of 19 - 50%. Sample studies have shown that at the age of 13 years, 7% of boys smoke at least three cigarettes a week, at the age of 14 years - 30% at the age of 15 years. - 36% and at the age of 16 years - 41.2%, i.e. these figures practically do not differ from those given by WHO. Moreover, in recent years, there has been a trend towards an increase in the number of girls smoking throughout the world.
Eating habits that contribute to obesity and lipid metabolism disorders are also established in childhood. Moreover, it was found that the elevated level of cholesterol in the blood detected in children persists quite persistently in their subsequent years.
High blood pressure also occurs in adolescence. Of course, not all children with high blood pressure will later become persistently hypertensive, but their risk is undoubtedly higher than that of children with normal blood pressure. According to epidemiological studies, in different countries, increased blood pressure is detected in 6-8% of adolescents. Moreover, according to observational data, in 42% of children who were found to have high blood pressure at the age of 13 years, it remained elevated at the age of 18 years, i.e. these are already real candidates for hypertension.
Currently, in various countries of the world, including Russia, programs are being carried out aimed at combating risk factors for cardiovascular diseases, starting from childhood. Preliminary results show that by teaching the basics of a healthy lifestyle and promoting the cessation of bad habits, the prevalence of risk factors for cardiovascular disease can be reduced. Promotion of a healthy lifestyle should be carried out in the family, school and by teenagers themselves. The example of parents plays an important role: children of smoking parents smoke more often; children of parents leading a sedentary lifestyle are also physically inactive. Eating habits also largely depend on parents. Teenagers, especially those who have authority among their peers, can successfully promote a healthy lifestyle. Moreover, often the example of a friend and the desire to be like him have a stronger influence on the behavior of a teenager than the recommendations of parents.
At the same time, children can positively influence the habits of their parents, being promoters of a healthy lifestyle. Teenagers themselves can actively influence the bad habits of their friends, helping to get rid of them. This is one of the most effective methods of influence.
Thus, the basis of primary prevention of cardiovascular diseases is the fight against risk factors for these diseases. It's better, of course, to avoid the habits that create these risk factors, but at the same time, it's never too late to try to give them up.
If we analyze the essence of the recommended healthy lifestyle, then there is nothing in it that is very difficult to live without. To keep your heart healthy, you need to eat rationally (a diet containing moderate amounts of calories, salt, fat, cholesterol), monitor your body weight, exercise regularly, stop smoking and drinking alcohol, and regularly monitor your blood pressure. As you can see, there is nothing fundamentally new or impossible. Following these simple recommendations will help you avoid many diseases without any restrictions on your active and enjoyable lifestyle.
Secondary prevention of coronary artery disease
Patients with an established diagnosis of ischemic
heart disease must especially carefully observe measures to prevent the further
development
of the pathology and its complications - unstable angina, chronic heart failure, myocardial infarction.
A set of secondary prevention measures
- Avoiding any nervous tension or learning self-control techniques that will help reduce the risks of stress spasm of the coronary arteries.
- Therapeutic physical education (therapeutic physical education). The initial level of activity and the dynamics of its growth are determined by the doctor based on body weight, level of fitness, age and severity diseases
.
- Reception appointments medications
.
After assessing the severity condition
, the cardiologist prescribes statins (lowering low-density lipoprotein levels), antiarrhythmics, antihypertensives and blood thinners. - Surgical treatment methods in cases where the disease progresses rapidly despite the implementation of the above measures prevention
.
Risk factors for coronary heart disease
All risk factors for coronary heart disease can be divided into removable (modifiable) and irreducible (non-modifiable).
Unavoidable risk factors include:
- Age (men over 45 years old, women over 55 years old);
- Gender (male);
- Hereditary predisposition.
Other risk factors can be minimized. They include:
- Smoking;
- Lipid metabolism disorders (hypercholesterolemia);
- Physical inactivity and stress;
- Excessive nutrition;
- Diabetes;
- Arterial hypertension.
If a person has at least one risk factor, then the likelihood of developing IHD increases by 2-3 times. When several factors are combined, the risk of death from coronary heart disease increases up to 15 times. prevention of coronary artery disease is so important .
Risk factors for circulatory system diseases and their prevention
Risk factors for circulatory system diseases and their prevention
1. Biological (non-modifiable) factors:
- elderly age,
- male gender,
- genetic factors contributing to the occurrence
- - dyslipidemia,
- - hypertension,
- - glucose tolerance,
- - diabetes mellitus
- - obesity
2. Anatomical, physiological and metabolic features:
- arterial hypertension,
- dyslipidemia,
- obesity and the pattern of fat distribution in the body,
- diabetes
3. Behavioral factors:
- eating habits,
- smoking,
- physical activity,
- alcohol consumption,
- exposure to stress.
The presence of even one of the risk factors increases the mortality rate of men aged 50-69 years by 3.5 times, and the combined effect of several factors - by 5-7 times.
Currently, a distinction is made between primary, secondary and tertiary prevention of diseases of the circulatory system (hereinafter referred to as CVD). The first two types of prevention are consistent with previously put forward provisions, namely: primary prevention of coronary heart disease (hereinafter referred to as IHD) is the prevention of the development of the disease in healthy individuals and persons burdened with various risk factors, and secondary prevention is the prevention of the progression of the disease and the development of complications of the course of CHD. in people who already have this disease.
Tertiary prevention refers to the implementation of actions aimed at delaying the progression of heart failure (hereinafter referred to as HF). In heart failure, the relationship between traditional risk factors and disease outcome breaks down. The functional state of the left ventricle plays a decisive role. The onset of left ventricular remodeling is the starting point for tertiary prevention.
The main components of primary prevention are population strategy and individual prevention (high-risk strategy).
The population strategy, or mass prevention strategy, is to create a healthy lifestyle, which primarily involves reducing tobacco smoking, establishing a balanced diet, increasing physical activity for the entire population and improving the environment. These are, as a rule, government events that involve the involvement of not only and not so much the Ministry of Health, but other ministries and departments (Ministry of Sports and Tourism, Ministry of Agriculture, Ministry of Information, etc.).
Individual prevention (High-risk strategy) is the identification of individuals with high levels of risk factors (smoking, arterial hypertension, hypercholesterolemia, excess weight, low physical activity, etc.) and their correction.
The current recommendations “Prevention of Coronary Heart Disease in Clinical Practice”, developed by the working group of the European Society of Cardiology, the European Atherosclerotic Society and the European Society of Hypertension, emphasize the importance of assessing overall cardiovascular risk.
The priority for primary prevention, according to European guidelines, is healthy individuals who are at high risk of developing coronary artery disease or other atherosclerotic diseases due to a combination of risk factors, including smoking, high blood pressure and lipid levels (increased total cholesterol and low-lying lipoproteins). density (LDL), low high-density lipoprotein and high triglycerides, elevated blood glucose, family history of premature coronary disease or high hypercholesterolemia and other forms of dyslipidemia, hypertension or diabetes.
Secondary prevention should also include lifestyle changes (stop smoking, avoid second-hand smoke, eat rationally to lose weight, reduce blood pressure and cholesterol levels, control blood glucose, increase physical activity). If active lifestyle changes fail to achieve target levels of risk factors, drug therapy should be added. Patients with angina pectoris and those who have had a myocardial infarction should give preference to beta-blockers, and if they are not tolerated, long-acting calcium channel blockers.
ACE inhibitors should be prescribed to patients with significant left ventricular systolic dysfunction. Almost all patients are prescribed antiplatelet drugs such as aspirin 75 mg per day, etc. Simultaneous administration of aspirin and ACE inhibitors is undesirable.
If, with lifestyle changes, target cholesterol and LDL cholesterol levels are not achieved, lipid-normalizing drugs, primarily statins, must be prescribed. It is also necessary to correct high blood pressure and glucose levels.
The most unfavorable combination of risk factors is the so-called metabolic syndrome (MS), which is a complex of interrelated disorders of carbohydrate and fat metabolism, as well as the mechanisms of regulation of blood pressure and endothelial function. The basis of these disorders is a decrease in tissue sensitivity to insulin - insulin resistance. The main components of MS are abdominal-visceral obesity, hypertriglyceridemia, hyperinsulinemia and arterial hypertension. When these factors are combined, atherosclerosis develops at an accelerated rate.
Due to the particular aggressiveness of MS, it is called “deadly quartet”, “deadly sextet”, “syndrome X”, “insulin resistance syndrome”.
To diagnose MS, they most often resort to measuring waist circumference, determining the level of triglycerides in the blood serum and fasting insulin, and monitoring blood pressure.
When MS is detected, preventive and therapeutic measures should be aimed at the entire set of risk factors and include weight loss, adequate control of glycemia and dyslipidemia, and normalization of blood pressure. The management tactics for patients with hypertension and MS have a number of features:
- immediate initiation of treatment with antihypertensive drugs in combination with non-pharmacological measures (diet, physical activity);
- focus on achieving optimal or normal blood pressure (below 130/85 mm Hg), since it has been proven that stabilizing blood pressure at this level and below gives a real organoprotective effect;
- more frequent use of combinations of antihypertensive drugs, which is due to greater resistance to reducing high blood pressure in such patients.
If general measures fail to normalize carbohydrate metabolism, it is necessary to resort to medication to increase tissue sensitivity to insulin by using biguanides (metformin), β-glycosidase inhibitors (acarbose, miglitol), thiazolindiones (cyclitazone, engystol, pioglitazone, troglitazone). Sensitivity can also be increased by increasing tissue blood flow with the help of ACE inhibitors, β-blockers (doxazosin) and other drugs. The same should be done for hypertriglyceridemia: prescribe fibrates, nicotinic acid preparations, etc.
Tertiary prevention should be targeted specifically from the onset of left ventricular remodeling. This is the most important part of all preventive measures for CSD, since almost half of the hospitalizations of patients with cardiovascular pathology are for heart failure. The rate of re-hospitalization among patients with CHF within 3 months after discharge reaches 47%, within 6 months - 54%. The costs of treating patients with CHF exceed the costs of treating patients with the most common forms of cancer and myocardial infarction. Left ventricular function in such patients has a primary influence on the outcome of the disease. Low or normal blood pressure, elevated cholesterol and brain natriuretic peptide levels increase the risk of heart failure and are associated with increased mortality.
It has been proven that the main drugs that protect the myocardium are ACE inhibitors and beta blockers. It has now been practically established that aspirin has an adverse effect in the treatment of patients with CHF. Nothing is known yet about the safety and effectiveness of statins in patients with HF.
Currently, a multidisciplinary approach to the treatment of heart failure is generally accepted, the essence of which is to unite doctors and representatives of other specialties to comprehensively address the many medical, psycho-social, behavioral and financial problems faced by patients with heart failure and the doctors treating them.
One of the organized forms for the practical application of a multidisciplinary approach to the treatment of CHF is the heart failure clinic. It can be presented both as an inpatient unit and as a day hospital at an outpatient clinic facility, which has at its disposal the means for diagnosis, monitoring and the ability to provide adequate treatment.
The team that will be involved in the treatment of patients with CHF in heart failure clinics, according to LR Erhardt, should include a cardiologist or heart failure specialist, a specially trained nurse, a gerontologist, a social worker, a physiotherapist, a general practitioner, a psychologist, a nutritionist and clinical pharmacologist.
What goals need to be achieved in the fight against risk factors?
According to WHO, three main risk factors make the greatest contribution to the risk of sudden death: hypertension, hypercholesterolemia (dyslipidemia) and smoking.
Arterial hypertension (HTN) is often called the “mysterious and silent killer.” Mysterious - because in most cases the causes of the disease remain unknown, silent - because in many patients the disease is asymptomatic and they do not know about the presence of high blood pressure (BP) until any complication develops. In order to correctly determine the risk of developing arterial hypertension and, as a result, coronary artery disease, you need to know and control your blood pressure level, and, if necessary, undergo an examination that will help clarify disorders of carbohydrate and fat metabolism and the degree of damage to target organs (vessels, heart, kidneys) , brain).
Analysis of the study results showed that to diagnose target organ damage in our country, examination methods such as ultrasound of the brachiocephalic arteries (in 9% of patients, versus 24.1% in other countries), determination of microalbuminuria (in 0.7% of patients versus 10% in other countries), and 24-hour blood pressure monitoring is performed less frequently (in 8.9% of patients, versus 24.5% in European countries).
An analysis of prescribed antihypertensive therapy showed that treatment of patients with hypertension in the Republic of Belarus is carried out with modern drugs, in 80.4% combination therapy is prescribed, which is comparable to the results of treatment in other European countries. In our country, as well as in comparison countries, there is a low effectiveness of treatment of patients with hypertension with concomitant diabetes mellitus (the target level is achieved in only 10% of patients).
Dyslipidemia is an imbalance in the content of “bad” and “good” fat fractions in the blood towards an increase in “bad” and/or a decrease in “good” fats. “Bad” fats, an increased amount of which greatly increases the risk of developing atherosclerosis and coronary artery disease, include cholesterol, low- and very low-density lipids, and triglycerides. To the “good” fats, i.e. Preventing the development of CVD include high-density lipids. With the exception of a small number of people with hereditary hypercholesterolemia, cholesterol levels are generally associated with poor diet. A balanced diet requires eating plenty of fruits and vegetables, healthy breads, lean meats, fish and legumes, along with low- or no-fat foods.
Soft margarine, sunflower, corn, rapeseed or olive oil should be used. The total fat content should not exceed 30% of the total energy composition, and the saturated fat content should not exceed 1/3 of all fat consumed. Many years of clinical experience indicate the unique properties of omega-3 polyunsaturated fatty acids, which help reduce the risk of CVD and its complications. More than 30 years ago, a group of Danish researchers suggested that the low incidence of cardiovascular pathology among the Greenland Eskimos was associated with their high consumption of deep-sea fish and seafood.
In epidemiological comparative, prospective and clinical studies, it has been shown that the intake of omega-3 polyunsaturated fatty acids at a dose of 2-4 g per day, both with increased amounts of fish consumed and in the form of encapsulated fish oil, leads to the correction of dyslipidemia and reduces the risk of death in patients who have had myocardial infarction. The presence of dyslipidemia is determined by a doctor based on the results of a biochemical analysis of venous blood. If dyslipidemia is present, its correction begins with diet. If, with the help of diet and balanced nutrition, it is not possible to reduce the lipid spectrum within 3 months, and a person simultaneously has other risk factors, drug therapy is prescribed.
A balanced diet is a balanced, regular (at least 4 times a day) diet with limited salt intake. Research by scientists has shown that if you limit your salt intake, the risk of myocardial infarction and other heart events can be reduced by 25%. It is very useful to increase the consumption of foods containing potassium and magnesium (seaweed, raisins, beets, apricots, zucchini, pumpkin, buckwheat).
Healthy food choices
All individuals should receive professional advice on food choices and follow a diet that is associated with minimal risk of developing CVD.
General recommendations (determined according to cultural traditions):
- food should be varied, energy consumption should be optimal to maintain ideal weight;
- Consumption of the following foods should be encouraged: fruits and vegetables, whole grains and breads, low-fat dairy products, lean meats, fish;
- consume products containing fish oil and w-omega, which have special protective properties;
- the total fat content should not exceed 30% of the total energy composition, and the saturated fat content should not exceed a third of all consumed fats; the amount of cholesterol consumed should be less than 300 mg/day;
- with a low-calorie diet, saturated fats should be replaced partly with carbohydrates, partly with monounsaturated and polyunsaturated fats from vegetables and marine animals.
In the diet, it is recommended to limit the consumption of animal products rich in cholesterol and saturated fats: fatty meats, lard, butter, sour cream, egg yolk, fatty cheese, sausage, sausages, all offal, fish caviar, shrimp, squid. It is recommended to replace animal fat with vegetable fat, since the latter is rich in anti-atherogenic unsaturated fats. Polyunsaturated fats (PUFs) are found in the form of omega-6 linoleic acid in vegetable oil (sunflower, corn, cottonseed) and in the form of omega-3 alpha-linolenic acid in flaxseed and soybean oils. The minimum daily human need for essential linoleic acid is 2-6 g, which is equivalent to 10-15 g of sunflower oil (2-3 teaspoons).
Fish oil is rich in polyunsaturated omega-3 fatty acids (omega-3 PUFAs) - eicosapentaenoic acid and docosahexaenoic acid. Preference should be given to fish from the northern seas that contain a lot of omega-3 PUFAs (mackerel, sardines, tuna, salmon, mackerel, herring, halibut, etc.). It has been established that polyunsaturated fatty acids significantly reduce the level of TG and, to a lesser extent, total cholesterol. Other effects of omega-3 PUFA include its effect on blood pressure levels, suppression of thrombus formation and improvement of endothelial function. It has been established that the likelihood of developing coronary heart disease is reduced by at least 25-30% when eating fish 2-4 times a week.
Over the past decade, hydrogenated vegetable oils have been widely used in the diet. The level of trans isomers (harmful substances) in hard margarines can reach up to 60%. Trans isomers of unsaturated fatty acids are similar to saturated fatty acids in lipid metabolism. It has been proven that their consumption (more than 1%) increases the risk of development and progression of coronary heart disease due to a significant increase in the levels of total cholesterol and LDL cholesterol and a decrease in the concentration of HDL cholesterol. To prevent atherosclerosis, it is recommended to use only soft margarine, produced in tubes (margarine spread) and plastic boxes, with a low content of saturated fat and trans-isomers of fatty acids (FA) (less than 1%). Replacing butter with “soft” margarine reduces the risk of IHD by 10%. However, the amount of soft margarine consumed should be limited, spreading no more than 5 g on bread.
Typically, by limiting dietary cholesterol intake to 300 mg per day over time, it is possible to reduce its blood level by 10-15%, and by reducing total fat intake from 40 to 30% of the total caloric intake - by another 15-20%.
Another important principle of anti-atherogenic nutrition is increasing the consumption of plant-based foods that can bind and remove cholesterol from the body. In this regard, it is recommended to use:
— dietary fiber (at least 30 g per day); they are found in large quantities in fruits (pears, apples, oranges, peaches), berries (raspberries, strawberries, blueberries), vegetables (cauliflower, broccoli, green beans) and legumes (peas, lentils, beans);
- pectins (at least 15 g per day), which are found in fresh fruits (apples, plums, apricots, peaches), berries (black currants) and vegetables (carrots, beets);
— plant stanols (at least 3 g per day); they are contained in soybean and rapeseed oils, pine oil extracts; Recently, sterols/stanols, being plant lipids, have been shown to reduce LDL cholesterol levels in the blood by competitively inhibiting the absorption of cholesterol in the small intestine.
It has been proven that their regular use is accompanied by a decrease in the concentration of LDL cholesterol by 10-15%; Margarines and fermented milk products fortified with sterols/stanols are now available and may be a useful addition to a lipid-lowering (HL) diet or drug treatment for DLP.
To prevent atherosclerosis, it is recommended to eat more fruit - at least 400 g or 5 servings per day: 1 serving = 1 apple / 1 banana / 1 orange / 1 pear / 2 kiwi / 2 plums / 1 tablespoon of dried fruit / 1 large slice of melon or pineapple / 1 glass of juice. The amount of boiled or fresh vegetables in the diet should be at least 400 g (2 cups).
Basic principles of the diet recommended for the prevention of atherosclerosis and DLP:
1. regular consumption of a variety of vegetables and fruits (fresh vegetables for dessert);
2. the ratio between saturated, mono- and polyunsaturated fats should be 1:1:1;
3. moderate consumption of dairy products (skim milk, low-fat cheese and low-fat yogurt);
4. give preference to fish and poultry (without skin) over meat products;
5. from meat products, choose lean meat, without layers of fat;
6. consume no more than 2-3 eggs per week (the consumption of yolks is limited, but not the white, which can be unlimited).
Excess body weight increases the risk of developing coronary artery disease and other diseases associated with atherosclerosis. To estimate your weight, use a simple formula for determining your body mass index (weight (kg) / height (m2) = body mass index). If the body mass index is less than 25, this is the desired body weight; if more than 28 in women and 30 in men, we can talk about obesity. Moreover, the so-called central obesity (male type), when fat is deposited on the abdomen, is more dangerous. The presence of central obesity can be judged by waist circumference and the ratio of waist circumference to hip circumference. The risk of CVD increases in men with a waist circumference greater than 94 cm and, especially, with a circumference greater than 102 cm; in women, greater than 80 cm and 88 cm, respectively. The ratio of waist circumference to hip circumference in men is greater than 1.0 and in women greater than 0. 85 is a more accurate indicator of the central type of obesity. The most common causes of excess weight are family factors (some of which may be genetic, but more often reflect general eating habits), overeating, a diet high in fat and carbohydrates, and lack of physical activity. Overweight is most common among sections of society with lower cultural and educational levels, especially among women due to lack of a balanced diet.
Smoking is one of the main risk factors. Why is smoking dangerous? Because even one cigarette increases blood pressure for 15 minutes, and with constant smoking, vascular tone increases and the effectiveness of medications decreases. If a person smokes 5 cigarettes a day, this increases the risk of death by 40%, if one pack a day - by 400%, that is, the chances of dying are 10 times greater!
According to WHO, 23% of deaths from coronary heart disease are caused by smoking, reducing the life expectancy of smokers aged 35-69 years by an average of 20 years. Sudden death among people who smoke a pack of cigarettes or more per day is 5 times more common than among non-smokers. Smokers not only put their lives at risk, but also the lives of others (passive smoking increases the risk of coronary artery disease by 25-30%). After just 6 weeks of following a healthy lifestyle, dramatic changes in health occur, and among those who quit smoking, the risk of coronary heart disease is significantly reduced and after 5 years it becomes the same as for those who have never smoked.
Low physical activity contributes to the development of CVD 1.5-2 times more often than in people leading a physically active lifestyle. Walking at a brisk pace for half an hour a day can reduce the risk of heart disease by approximately 18% and stroke by 11%. For the prevention of CVD and health promotion, the most suitable physical exercises are those that involve regular rhythmic contractions of large muscle groups: fast walking, jogging, cycling, swimming, skiing, etc. The frequency of physical exercise should be at least 4-5 times a day. week, duration of classes is 30-40 minutes, including a warm-up and cool-down period. When determining the intensity of physical exercise acceptable for a particular patient, they proceed from the maximum heart rate (HR) after physical activity - it should be equal to the difference between the number 220 and the patient’s age in years. For people with a sedentary lifestyle without symptoms of coronary artery disease, it is recommended to choose an intensity of exercise at which the heart rate is 60-75% of the maximum. Recommendations for individuals with CAD should be based on clinical examination and exercise test results.
The Committee of the European Society of Cardiology has developed the main tasks for the prevention of CVD in a healthy person:
- systolic blood pressure below 140 mm Hg;
- no tobacco use;
— total cholesterol level below 5 mmol/l;
— low-density lipoprotein cholesterol below 3 mmol/l;
- walking 3 km a day or 30 minutes of any other moderate physical activity;
- daily use of at least 5 pieces of fruits and vegetables;
- Avoid obesity and diabetes.
The experience of multifactorial prevention of coronary artery disease carried out by the Republican Scientific and Practical Center "Cardiology" since 2000 at the population level in Minsk has shown that a decrease in the levels of risk factors in combination with active measures for secondary prevention is accompanied by a decrease in the incidence of myocardial infarction by 21%, cerebral stroke by 21%. 24%. At the same time, the practical implementation of preventive programs, which involves a set of measures to increase the population’s literacy in matters of a healthy lifestyle and resolve a number of social issues relating to a balanced diet, the organization of physical culture and health activities for the population, etc., requires the widespread involvement of republican and local government bodies.
Thus, to effectively prevent most cardiovascular diseases and their complications, you need to follow only 7 rules:
1. Monitor your blood pressure.
2. Control your cholesterol levels.
3. Eat right.
4. Exercise: A little is better than nothing.
5. Don’t start smoking, and if you smoke, try to quit, no matter how difficult it may seem.
6. Do not abuse alcoholic beverages.
7. Try to avoid prolonged stress.
In conclusion, even small lifestyle changes can slow down the aging of the heart. It's never too late to start living a healthy lifestyle. After a person develops signs of coronary artery disease, risk factors continue to act, contributing to the progression of the disease and worsening the prognosis, so their correction should be an integral part of treatment tactics.
Prevention of cardiovascular diseases
Cardiovascular diseases (CVD) of atherosclerotic origin, especially coronary heart disease (CHD), remain the leading cause of premature death worldwide. According to epidemiological studies, the prevention of CVD is highly effective. A 50% reduction in mortality from coronary artery disease is associated with interventions on risk factors and only 40% with improved treatment.
Prevention of CVD is a coordinated effort at the community and individual levels aimed at eliminating or minimizing the impact of CVD and associated disability. Preventive measures should be carried out throughout life, from birth to old age.
Basic prevention strategies:
Population: changing lifestyle, environmental situation, promoting a healthy lifestyle;
High-risk strategy: preventive measures aimed at reducing the level of CVD risk factors. These areas of prevention should complement each other.
Prevention of CVD can be divided into two groups:
Primary prevention includes a rational regime of work and rest, increasing physical activity, limiting table salt, giving up alcohol and smoking, reducing caloric intake and body weight. In fact, it is primary prevention that allows one to maintain rational conditions for human life. In essence, primary prevention of CVD includes a population strategy and a high-risk strategy. Secondary (drug and non-drug) prevention is carried out differentiatedly with groups of patients with verified CVD in order to prevent relapses of diseases, the development of complications in people with realized risk factors, reduce morbidity and mortality from these diseases, and improve the quality of life of patients. According to WHO, three main risk factors make the greatest contribution to the risk of sudden death: hypertension, hypercholesterolemia (dyslipidemia) and smoking. Classification of CVD risk factors:
Biological (non-modifiable) factors:
— Age, gender, heredity (early development of CVD in relatives), genetic factors contributing to the occurrence of dyslipidemia, hypertension, glucose tolerance, diabetes mellitus and obesity
— Anatomical, physiological and metabolic (biochemical) features: dyslipidemia, obesity and the nature of the distribution of fat in the body, diabetes mellitus.
Behavioral (modifiable) factors:
— Dietary habits, smoking, physical activity, alcohol consumption, exposure to stress.
The presence of even one of the risk factors increases the mortality rate of men aged 50-69 years by 3.5 times, and the combined effect of several factors - by 5-7 times. Thus, to influence CVD risk factors, it is necessary to motivate each individual to form a healthy lifestyle.
Activities that promote a healthy lifestyle and reduce the level of risk factors:
- Stop smoking (non-smokers stay in smoking rooms (passive smoking). If a person smokes 5 cigarettes a day, the risk of death increases by 40%, if one pack a day - by 400%, that is, the chances of dying are 10 times greater In the Republic of Belarus, tobacco smoking is an indirect cause of death in every fifth death of persons over 35 years of age.
- Follow a low-cholesterol diet: reducing saturated fats (reducing the consumption of fatty pork, introducing turkey and rabbit meat with low cholesterol into the diet), focusing on whole grains, vegetables (up to 5 servings per day are recommended), fruits and fish. Soft margarine, sunflower, corn, rapeseed or olive oil should be used. The total fat content should not exceed 30% of the total energy composition, and the saturated fat content should not exceed 1/3 of all fat consumed. 3. Reduce table salt consumption to 5 g/day. Reduce the consumption of foods containing “hidden” salt: smoked and boiled sausages, bread. Research by scientists has shown that if you limit your salt intake, the risk of myocardial infarction and other heart events can be reduced by 25%. It is very useful to increase the consumption of foods containing potassium and magnesium (seaweed, raisins, beets, apricots, zucchini, pumpkin, buckwheat). A balanced diet is a balanced, regular (at least 4 times a day) diet with limited salt intake.
- Reduce excess weight. Excess weight increases the risk of developing coronary artery disease and other diseases associated with atherosclerosis. Noteworthy is the fact that more than 12% of the population does not know their weight at all. The prevalence of overweight increases with age. To estimate your weight, use a simple formula for determining body mass index (BMI) = weight (kg) / height (m 2).
BMI up to 24.9 is normal body weight;
25-29.9 – overweight;
30-34.9 – I degree obesity;
35-39.9 – II degree obesity;
40 or more – III degree obesity.
Moreover, the so-called central obesity (male type), when fat is deposited on the abdomen, is more dangerous. The presence of central obesity can be judged by waist circumference (WC) and the ratio of waist circumference to hip circumference. The risk of CVD increases in men with a WC greater than 94 cm and, especially, with a circumference greater than 102 cm, in women - more than 80 cm and 88 cm, respectively. The ratio of waist circumference to hip circumference in men is more than 1.0 and in women more than 0.85 is a more accurate indicator of the central type of obesity.
For men with WC < 102 cm and women with WC < 88 cm and/or BMI < 30 kg/m2, it is recommended not to gain weight.
For men with WC ≥ 102 cm and women with WC ≥ 88 cm and/or BMI ≥ 30 kg/m2, it is recommended to reduce body weight.
5. Monitor blood pressure. Maintain blood pressure level no higher than 140/90 mm Hg. Art.
6.Increase physical activity. At least 150 minutes per week of moderate aerobic (walking, swimming, cycling) physical activity (30 minutes per day, 5 times per week) or 75 minutes per week of vigorous physical activity, or a combination.
7. Monitor lipid metabolism indicators. In patients with very high CV risk, it is recommended to achieve a target low-density lipoprotein cholesterol (LDL-C) level of <1.8 mmol/L or reduce it by at least 50% if the baseline value was 1.8-3.5 mmol/L (ESC, 2016). For patients with high cardiovascular risk, it is recommended to achieve a target LDL-C level of <2.6 mmol/l or reduce it by at least 50% if the initial value was 2.6-5.1 mmol/l. In the remaining patients, the target LDL-C level is <3.0 mmol/l.
8. Limit alcohol intake. Less than 2 standard drinks (1 dose - 12 g/18 ml ethanol) per day for men and less than 1 standard dose for women per day, which is approximately equal to 330 ml of beer, or 150 ml of wine, or 45 ml of spirits.
9.Control glycemia. Glycated hemoglobin level < 6-6.5%.
10. Avoid prolonged stressful situations.
Even small lifestyle changes can slow down premature aging of the heart and blood vessels. It's never too late to start living a healthy lifestyle. After a person develops signs of coronary artery disease, risk factors continue to act, contributing to the progression of the disease and worsening the prognosis, so their correction should be an integral part of treatment tactics.