Defects in the development of cardiac structures are encountered in the practice of medical specialists in the vast majority of cases.
Relatively rarely (25-30% of all recorded situations) they are congenital. Most often acquired. Many could have been avoided if the patient had consulted a doctor earlier.
Left atrium hypertrophy is an increase in its volume as a result of overload and thickening of the muscle layer. The pathology is associated with a minimal clinical picture in the early stages of development.
As the symptoms progress, they become obvious, but even in this case, only diagnostics can answer the question of the origin of the phenomenon.
Mortality is relatively low and amounts to 3-5% over a period of almost 8 years (data from European associations of cardiology). This does not mean that treatment should be taken lightly. The development of the condition is associated with an increase in the risk of death at a rapid pace.
Hypertrophy is not primary. In the sense that it always develops as a result of a third-party disease: the heart, endocrine, nervous system, blood vessels. Recovery is about eliminating the root cause.
Development mechanism
Left atrial hypertrophy (abbreviated as LHA) is an independent pathological process. It is similar in nature and typical features to cardiomyopathy. The development of the defect occurs in two main ways.
Normally, a muscular organ pumps the volume of blood that enters it. Adequate load leads to the complete release of liquid connective tissue from the chambers. Hence the stable operation of the structures.
If a failure occurs, the atria and/or ventricles are filled to capacity, resulting in an inability to discharge normally. Hence the overstretching of all chambers or dilatation, in other words.
This situation is most typical for professional athletes or persons suffering from congenital or acquired defects.
Another possibility is that blood returns to the left atrium from the ventricle due to mitral valve stenosis or prolapse.
The second pathogenetic mechanism concerns overload of the muscle layer - the myocardium. A similar phenomenon occurs as a result of a long course of third-party pathologies.
The main one is hypertension with numbers above 160 by 90 mmHg. The same effect is provoked by diseases of the lungs and excretory system.
Several factors may be influencing at once. Then mixed hypertrophy develops, which is difficult to treat with standard methods.
Classification
Some typifications have clinical significance.
Based on the moment of development
- Congenital appearance. Caused by disorders of the prenatal period or genetic mutations (including spontaneous ones).
In the latter case, a complex violation of anatomical structures occurs. Not only the left atrium is affected, but also the ventricles.
In addition, cosmetic defects, pathologies of the maxillofacial area and others are possible. Depends on the syndrome.
- Acquired type. Occurs more often. Develops in patients who abuse alcohol and smokers. Also during the course of hypertension and third-party defects of cardiac structures. In the early stages it is treatable, but later it becomes difficult. Complete impossibility of therapy in the final phase.
According to anatomical properties
Symmetrical view of the GLP. Left atrial hypertrophy is characterized by thickening of the myocardium at the affected sites. Moreover, along the entire length of the structure, the increase may be different.
The nature of the deviation is assessed using the so-called asymmetry index. In this case, the growth of the muscle layer is uniform, the indicator is within 1.3.
The treatment is standard and consists of stopping the root cause, that is, the main pathology. Symptoms are minimal, making early diagnosis difficult.
Asymmetrical type. The index of the same name is over 1.3, which indicates uneven growth of the myocardium within the atrium. Evidence in favor of a possible congenital developmental disorder.
By stages of formation
- Enlargement of the left atrium in compensation. The first phase of the development of the disease. Symptoms are completely absent; the echocardiogram shows minor or no abnormalities.
No recovery required. Dynamic observation under the supervision of a specialized specialist is indicated.
- Subcompensation. Second stage. It develops as a result of a long course of the main pathological process. At the same time, the deviation itself is minimally expressed.
Symptoms are present, but they are nonspecific: chest pain, rare episodes of tachycardia, fatigue, increased fatigue, short periods of shortness of breath after intense physical activity.
Treatment is required; inpatient therapy is possible at this stage. There is no longer any need to wait for independent regression.
- Decompensation. In some classifications it is the final stage, which is not entirely true. The clinical picture is pronounced. Accompanied by cardiac symptoms, as well as manifestations from the cerebral structures and excretory tract.
Treatment is urgent, in a hospital. The process is accompanied by severe heart failure, death can occur at any time, the risks are high.
- Terminal phase. Extreme degree of violation. Cannot be corrected in principle. The approximate period from the beginning of myocardial growth to the formation of the final state is 3-10 years. It happens more, depending on the endurance of the body. Palliative care, for relief. The count goes on for weeks, rarely months.
Classifications, especially staging, are used to develop therapeutic tactics and determine the diagnostic vector.
Treatment
When HLP appears, heavy physical activity is contraindicated. It is necessary to give up smoking and drinking alcohol, as well as strong tea, coffee, and tonic drinks. Dietary restrictions on salt and saturated fat are recommended. It will not be superfluous to eat foods rich in potassium (dried apricots, bananas, baked potatoes). You can also use folk remedies to maintain myocardial metabolism: the fruits of hawthorn, rowan, viburnum, honey. Walking in the fresh air helps improve the functional state of the myocardium. To reduce anxiety and stress, your doctor may recommend taking herbal sedatives. GLP has no specific treatment. Treatment is carried out for the disease that was its cause. For heart defects, surgical treatment is possible. Hypertension and coronary heart disease are treated according to appropriate standards. Treatment for pulmonary hypertension includes medications and inhaled nitric oxide. In cases of severe heart failure, heart transplantation may be indicated.
Causes
Development factors are mainly pathological. There is one exception to the rule.
Intense physical activity
This is not about simple activity, but about activity at the limit of the body’s capabilities. These are mostly professional athletes, fanatically enthusiastic amateurs.
If the left atrium is enlarged (this happens sooner or later), dynamic monitoring under the supervision of a cardiologist is indicated. Rapid progression is grounds for lifelong withdrawal from sports.
What happens when you overexert yourself? Muscles require an intensive supply of oxygen and nutrients. The body intensifies its work. The chambers are overflowing with blood. Hence the dilatation, expansion of the atrium.
On the other hand, the myocardium is forced to function faster, contract more often and more strongly. Hypertrophy - building muscle mass. This is an adaptive mechanism.
Chronic obstructive disease, bronchitis, asthma
And other respiratory pathologies. Associated with impaired supply of cardiac structures with oxygen and nutrients. The result is ischemia.
False growth of the myocardium is possible, when in fact it is not new muscle tissue that is formed, but scar tissue.
Therapy is very difficult. The described pathologies are in principle incurable. The only chance is to transfer them into a state of long-term high-quality remission, but this also requires a lot of effort.
Renal failure in the decompensation phase
Also pyelonephritis and other conditions that provoke an increase in blood pressure.
In this regard, malignant hypertension is the most aggressive. It quickly “shrinks” the heart, as well as the brain, deprives the patient of vision, and leads to the destruction of blood vessels.
Restoration is urgent. In the specialized department of the hospital. In the later stages, pathologies are poorly eliminated. Therefore, it is recommended to attend to early diagnosis and treatment by a nephrologist.
Read more about what other kidney pathologies increase or decrease blood pressure here.
Arterial hypertension
An extremely complex pathology. It is often very difficult to detect the origin factor of the disease. Because we can talk about a group of reasons.
In some situations, doctors are forced to diagnose the idiopathic form (if the cause remains unclear).
The condition does not require delay in terms of treatment. Relatively quickly, the pathological process stops responding to exposure and becomes resistant to drugs.
The prospects for eliminating left atrial hypertrophy directly depend on success in the fight against hypertension.
Narrowing of the aortic lumen
As a result of a malfunction of the corresponding valve or a congenital defect (coarctation).
Recovery is carried out surgically. Prosthetics or stenting (artificial expansion of the lumen) is possible.
Success depends on the extent of the affected area and the stage of the hypertrophic process. If anatomical disorders are persistent, they cannot be reversed. In the early stages this is not required.
Mitral valve defects
According to the type of prolapse (retraction of the valves into the previous chamber of the heart), also stenosis (up to complete fusion, when blood is not able to move to the left ventricle).
More often it has an acquired origin. Develops after infectious and inflammatory diseases and connective tissue pathologies. Treatment is strictly surgical, using prostheses.
Success depends on the stage of the pathological process. The sooner action is taken, the higher the likelihood of full recovery. It makes sense to act early.
An indirect effect is caused by lipid metabolism disorders. Obesity is considered a consequence, but not a cause. Therefore, calling increased body weight a factor in the development of cardiac problems does not make sense. This is false information.
Causes of pathology
The myocardium is a muscle that tends to hypertrophy. But if in the case of ordinary muscle tissue this is not dangerous, then with cardiac tissue the opposite is true. Left atrium enlargement is a pathological condition that requires treatment.
Hypertrophy can be true or false. The first type is caused by hyperplasia, that is, the proliferation of certain cells. It is the result of high stress on an organ or system. This species is also called a worker. People who deal with high physical activity are often susceptible to true hypertrophy.
The false type of enlargement is the progressive proliferation of fat cells, which leads to this type of hypertrophy. This form of the disease is most often observed in people with a sedentary lifestyle.
The mechanism of the hypertrophy process is as follows: the human heart has 2 halves (right and left). Each of them is divided into a ventricle and an atrium, which are connected by openings. The lumen of these holes is also equipped with valves. On the left it has two doors, and on the right - three.
Thanks to them, the heart regulates blood circulation through systematic contraction and release of blood portions into nearby vessels. During heavy physical activity, the body's cells' need for oxygen increases, causing the heart to work faster. To do this, you need more muscle tissue, which is formed during such overloads.
Such changes are fraught with consequences, the most unfavorable of which is death. In addition to heavy physical activity, there are also a large number of factors that can lead to hypertrophy. You need to know them and try to avoid them.
Hypertrophy of any part of the heart can be congenital or acquired. This pathology can affect several heart chambers at once, but the left atrium is more often affected. It is the increase in the size of this section that does not act as a separate disease, but is only a symptom that indicates concomitant pathological processes.
There are many reasons for increased thickness of the walls of the left atrium. The main ones can be called:
- excess weight, especially in young people;
- cardiovascular pathologies;
- narrowing of the mitral valve in the cavity of the left atrium;
- high blood pressure;
- insufficiency of the valve apparatus;
- frequent stressful situations and depression;
- acute renal failure;
- diabetes;
- respiratory diseases;
- constant physical activity;
- playing sports;
- the presence of muscular dystrophies;
- presence of bad habits;
- severe genetic inheritance.
Narrowing of the mitral valve is a heart defect. Its essence lies in stenosis of the fissure, which is a connecting channel for the atrium and ventricle.
This syndrome is often accompanied by severe insufficiency of this valve, which is characterized by the process of regurgitation. Some of the blood flows back from the ventricle into the atrium, and the valve is unable to prevent this.
Sports can also be a cause of this cardiac pathology if the loads do not correspond to the person’s capabilities. With frequent and high tension, the heart muscle cannot cope with the influx of a large amount of blood; it needs additional strength to push it out. As a result, an increase in cardiac muscle tissue can be observed to compensate for this process. Before choosing the type and amount of sports activity, you should first consult with specialists and find out about training and possible regimes.
Ignoring heart problems is very dangerous. To protect yourself from possible malfunctions of the main organ, you need to lead a healthy lifestyle, moderately engage in physical activity and sports, and also consult doctors more often for the timely detection of various concomitant diseases.
Symptoms
Signs of left atrial hypertrophy are varied. But they manifest themselves in later stages, starting with subcompensated and further aggravating until the patient is completely disabled.
- Chest pain. Usually of low intensity even in the most pronounced phase of the pathological process. They are detected after physical exertion, stress, an attack of suffocation against the background of pulmonary problems. The nature of the sensation is pressing, pulling or burning.
- Disturbance of normal heart rhythm. According to the type of paroxysms of tachycardia. Attacks occur spontaneously, last from 2 to 20 minutes or more, depending on the form and persistence of changes in the muscle layer of the organ.
Other arrhythmias occur in parallel. Like atrial fibrillation, and then ventricular fibrillation. These are alarm bells and may lead to death.
- Dyspnea. After intense physical activity. The threshold for symptoms to appear in the early stages is high.
As the disease progresses, the condition accompanies the patient constantly, and does not weaken even in complete rest.
The patient is unable to walk or climb stairs; everyday responsibilities fall on his shoulders as a heavy, exorbitant burden. The question of assigning a disability group is raised.
- Impaired consciousness such as frequent, short-duration fainting. Also a worrying sign. It speaks of involvement of the brain and the onset of ischemia of nerve tissue.
- Fast fatiguability. A small incentive is enough. Not necessarily physical. Mental stress is also difficult to bear.
- Cyanosis of the nasolabial triangle. Especially at the time of tachycardia or an attack of acute pain in the chest.
- Paleness of the skin and mucous membranes.
In addition to purely cardiac symptoms, manifestations of the underlying pathological process are added.
A motley clinical picture is emerging that needs to be analyzed point by point. This requires time and sufficient qualifications.
The patient is recommended to consult a doctor if at least one symptom is present.
What examinations are necessary to confirm the diagnosis?
The doctor may suspect cardiac hypertrophy or a disease that can lead to it when interviewing and examining the patient.
The survey takes into account the nature of the complaints and the conditions under which they arise (rest or physical activity, wakefulness or night time, etc.).
characteristic blush during hypertrophy due to mitral stenosis
During the examination, special attention is paid to the skin. With mitral stenosis, a so-called “mitral” blush on the cheeks of a violet-pink color may be observed, with insufficiency - pallor and looseness of the skin with a bluish coloration of the nails, tip of the nose, and ears. This is due to a decrease in oxygen content in the blood in chronic heart failure. The severity and localization of edema is also assessed (in severe stages, edema from the legs and feet spreads higher, involving the external genitalia, thighs, and abdomen).
The diagnosis can be clarified by auscultation (listening) of the heart and lungs. In severe stages of heart failure, dry or moist rales are heard in the lungs in the lower sections. With hypertension, the patient hears an accent of the second tone at the point of listening to the aorta (in the second intercostal space to the right of the sternum), and with mitral stenosis, a rough noise is heard in the projection of the mitral valve (under the left nipple in the fifth intercostal space). With mitral valve insufficiency, a systolic murmur can be heard at the same point.
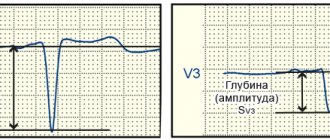
Any patient with cardiac complaints must undergo an ECG. On the cardiogram it is easy to see signs of left atrial hypertrophy. Due to the fact that conduction through the atria is reflected by the P wave (the ascending part characterizes the excitation of the right atrium, and the descending part characterizes the excitation of the left atrium), then with hypertrophy of the left atrium on the ECG, the descending part of the P wave increases and lengthens in duration. The tooth takes on an M-shape and is called P-mitrale, in contrast to P-pulmonale with hypertrophy of the right atrium.
Pictures: ECG signs of left atrial hypertrophy
In addition to an ECG, a patient with a heart murmur must undergo a cardiac ultrasound. During ultrasound examination, signs of left atrium hypertrophy are parameters exceeding the following indicators: 1.85-3.3 cm and a size index of more than 1.45-2.9 cm/m2.
An examination method such as chest x-ray allows not only to detect congestion of blood in the lungs (and in severe cases, congestive pneumonia or pulmonary edema), but also to determine the degree of enlargement of the heart. With mitral defects with pronounced thickening of the walls of the left atrium, the heart acquires the so-called mitral configuration - smoothing of the waist of the heart.
GLP on X-ray
As prescribed by the doctor, other diagnostic methods may be prescribed - ultrasound of internal organs and kidneys, biochemical blood tests, exercise tests to determine the functional class of CHF.
Diagnostics
It is carried out under the supervision of a cardiologist. As necessary, third-party specialists are involved (pulmonologist and others).
The examination takes place on an outpatient basis, excluding acute conditions:
- Oral questioning of the patient and collection of anamnestic data. Allows you to decide on the further course of action.
- Measurement of blood pressure, heart rate. Both are above the norm. In the acute period, the deviation is especially noticeable.
- Auscultation. Listening to sound. A distinct noise is detected.
Routine techniques provide the necessary vector for further diagnosis:
- Daily monitoring using an automatic tonometer. Records vital signs within 24 hours. The value of the method lies in the possibility of constant monitoring, while the patient is in natural conditions, is not nervous, and is engaged in usual activities.
- Electrocardiography. Assessment of the functional state of cardiac structures. Left atrial hypertrophy has typical features.
- Echocardiography. The main way to identify a pathological process. Visualization makes it possible to determine the stage and nature of the defect.
- MRI if necessary.
Other studies: general blood test, biochemical and hormonal tests, assessment of neurological status, EEG and others. The list may be expanded at the discretion of third-party specialists.
Signs on ECG
There are several typical features:
- Changes in the height, shape (“bihump”), and width of the P wave.
- Widening of the QRS complex.
The contraction frequency is normal or increased if the registration of indicators is carried out at the time of an attack of tachycardia.
Other elements are determined by the doctor. In total, there are about 10-15 characteristic features that are difficult for independent perception, much less deciphering.
Signs of left atrial hypertrophy on the ECG are determined by predominant changes in the P wave.
What symptoms can be used to recognize an enlarged left atrium?
There are no strictly specific clinical manifestations of left atrial hypertrophy itself. However, any patient will have those signs that are most characteristic of the causative disease that caused hypertrophy.
Thus, mitral stenosis is characterized by hemoptysis, attacks of dry obsessive cough and shortness of breath with exertion, which increases in the supine position. With mitral valve insufficiency, shortness of breath gradually increases and sensations of interruptions in the work of the heart or rapid heartbeat occur, caused by paroxysmal types of tachycardia (atrial fibrillation, supraventricular tachycardia, frequent ventricular extrasystole). As chronic heart failure progresses, shortness of breath is observed even at rest and with minimal household activity, and swelling of the legs and feet also increases.
A slight increase in the left atrium, caused by arterial hypertension, is accompanied by frequent deterioration with very high blood pressure numbers (180-200 mmHg and above), with frequent crises, difficult to treat with antihypertensive drugs.
If there are any complaints from the cardiovascular system, a consultation with a cardiologist or therapist is necessary for further examination, and the diagnosis of left atrium enlargement is established based on the results obtained.
Treatment methods
Depends on the root cause of the pathological condition. The point is to eliminate the factor of origin. Symptomatic measures are taken in parallel, but do not replace etiotropic effects.
- Arterial hypertension is treated with a group of pharmaceuticals. ACE inhibitors (Perindopril), calcium antagonists (Diltiazem, Verapamil), centrally acting drugs (Moxonidine), beta blockers (Carvedilol, Anaprilin), and diuretics (Veroshpiron).
They are used in combinations, but proper selection is required. Using the wrong regimen will lead to early kidney or heart failure.
- Defects of the aorta or heart valves. Surgery is indicated. Prosthetics, shunting and other methods are most widely used.
- Lung pathologies are eliminated by the use of short courses of corticosteroids, as well as bronchodilators. But with caution. Both of them affect the heart.
Symptomatic therapy:
- Antiarrhythmics to restore an adequate rhythm. Amiodarone. It is also possible to use Anapralin to relieve acute attacks of tachycardia.
- Diuretics for edema of the lower extremities and face.
- Cardioprotectors. Mildronate.
- Nitroglycerin to relieve pain.
Quitting smoking and drinking alcohol in any quantity is mandatory. Don't overexert yourself physically and emotionally.
Diet according to indications. It makes no sense to strictly limit your diet. If there are problems with lipid metabolism, statins are indicated. Sports in case of hypertrophy are contraindicated.
Can left atrial hypertrophy be cured?
The correct treatment strategy is to eliminate the causes that led to thickening of the atrium.
For mitral valve stenosis, cardiac surgery is performed to cut adhesions or replace the valve with a bioprosthesis from a pig heart or, more often, a mechanical prosthesis. In case of isolated valve insufficiency, plasty is performed with suturing of the valve ring. Due to the fact that most often the same patient has a combined defect (both stenosis and insufficiency), it is advisable to treat it by performing an operation to replace an artificial heart valve.
If the cause of hypertrophy is arterial hypertension, the patient is advised to regularly take antihypertensive drugs, and if there is a persistent increase in blood pressure, a combination of drugs from groups with different mechanisms of action is indicated. The most optimal combinations are achieved by constant intake of ACE inhibitors (Prestarium, Diroton, Noliprel) and any of the following groups - diuretics (indapamide, veroshpiron, torsemide) or beta-blockers (carvedilol, concor, coronal) or calcium channel antagonists (amlodipine, verapamil).
Even in the absence of hypertension, a patient with heart disease must take a drug from the group of ACE inhibitors or beta-blockers, since the first group achieves a cardioprotective effect, and the drugs of the second reduce the heart rate, so that the heart muscle experiences less stress.
Complications
Consequences develop in the absence of treatment or with an inappropriate regimen.
- Heart failure. Often the ambulance is powerless to help the patient.
- Heart attack. Acute death or necrosis of cardiac structures. Leads to tissue scarring; at best, it ends in disability or minor limitations in life.
- Cardiac asthma. Formation of effusion in bronchopulmonary structures.
- Dangerous types of arrhythmias and, as a result, cardiac arrest.
- Stroke.
- Respiratory failure.
Forecast
Determined by the root cause of hypertrophy. Without connection with severe pathologies, death is unlikely and accounts for up to 3-5% of the total mass of clinical cases.
The recovery has good prospects. Without therapy, especially against the background of anatomical changes, the risks grow rapidly. Mortality is determined at 25-40%. The terminal phase guarantees a fatal outcome.
In general, the prognosis is better in the early stages, and the primary pathological process is also taken into account. The possibility of radical treatment and the success of surgery are associated with a better prognosis.
Overload of the left atrium is the main factor of hypertrophy. There are many reasons, the distinction is made within the framework of diagnosis.
Therapy is supervised by a group of specialists. Prospects are not determined immediately; the response to the impact, how long ago the condition is, and other factors play a role.