© Author: Sazykina Oksana Yuryevna, cardiologist, especially for SosudInfo.ru (about the authors)
Due to the active introduction of echocardioscopy (ultrasound of the heart) into the examination of the general population, the majority of heart diseases do not have a single chance to remain undetected. This is because even minor changes in the internal structure of the heart can be detected using ultrasound. Therefore, recently more and more patients are hearing from doctors that they have fibrosis of the heart valves, although there are still no clinical manifestations of the disease. This is, of course, good, because the earlier fibrosis, for example, of the mitral or aortic valve is detected, the greater the chance of preventing the development of adverse consequences.
Fibrosis of the heart valves is nothing more than the formation of excess connective tissue in the place where thin, elastic and smooth valve leaflets should be located in a normal heart (each valve has its own number of leaflets). Fibrosis can affect not only the valves themselves, but also the valve ring, to which the valves are attached on one side, and even the muscle tissue around the valve ring.
What happens with fibrosis of the leaflets?
fibrosis of the aortic heart valve
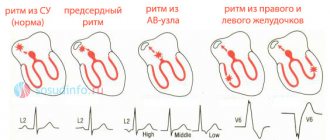
Normally, the leaflets of all four heart valves contain loose connective tissue. Its fibers are ordered, and the nutrition of cellular structures is carried out by the smallest blood vessels from the muscle tissue of the heart. When pathological factors influence the valve, as well as due to age-related characteristics, the connective tissue is replaced by coarser tissue, which is not able to maintain the elasticity and flexibility of the valves. The number of capillaries in the valves decreases, the valve tissue receives less nutrients, and some of the cells simply die off, being replaced by fibrous tissue. In fact, valve fibrosis resembles a scar at the site of exposure to a negative factor on delicate connective tissue. Often the concept of fibrosis is identified with sclerosis, which is also true. But sclerosis is more typical for the heart muscle itself, for example, post-infarction or post-myocardial cardiosclerosis. Although often in the conclusion of echocardioscopy you can read about sclerosis of the aortic root, or sclerosis of the mitral valve leaflets.
As fibrous tissue grows, the function of the valve leaflets becomes impaired. They are no longer able to close tightly when blood is expelled from the ventricle, for example, and then some of the blood “leaks” back into the atrium, gradually overstretching it and leading to further hemodynamic disturbances. Or, conversely, fibrous tissue from the valve ring grows towards the valves, leading to their fusion with each other, which sooner or later will provoke the formation of stenosis (narrowing) of the valve opening.
Fibrosis classification
Each form of pathology has its own characteristics.
- The focal form is the basic one. It is characterized by moderate fragmented damage to the structure of the valve apparatus.
- The diffuse type is characterized by a large area of damage (cusps and subvalvular space). It is detected at advanced stages of fibrosis development.
- The cystic form is perceived as a separate pathology. It manifests itself as serious disruptions in metabolic processes and leads to the formation of cysts.
If the cusps of the mitral valve are sealed, then it is not at all necessary that this is a heart defect. Fibrosis is only a pathological change that occurs under the influence of other factors, and not a diagnosis. Because of it, stenosis and valve insufficiency can develop. The appearance of voiced pathologies requires urgent medical intervention. The proliferation of fibrous tissue can be perceived as a substrate for the formation of cardiac muscle defects. However, it is unlikely to predict its development in advance. The chances of timely identification of the problem increase through regular examination.
How is fibrosis different from heart disease?
It must be remembered that the concept of cardiac fibrosis as such is not a diagnosis. That is, these are anatomical and morphological changes that can cause stenosis (in particular, mitral stenosis, aortic stenosis) or valve insufficiency. The last two concepts are precisely diagnoses that require certain additional examination and treatment.
Fibrosis, sclerosis or calcification is just a substrate for the development of a heart defect, and whether a defect will develop or not cannot be predicted in advance. But you can regularly see a doctor, and in case of the slightest signs of a defect or chronic heart failure, receive timely treatment. Here we are talking about the fact that the earlier risk factors for the development of heart disease are identified in a patient, the more often he will perform an ultrasound of the heart, and, accordingly, time will not be lost.
Causes of cardiac fibrosis
the mitral valve is most commonly affected . In second place in frequency is the aortic valve . Infection, inflammation, calcium deposition, congenital features, etc. can lead to the replacement of normal valve tissue with fibrous tissue.
Most often, fibrosis of the heart valves is caused by the following conditions and diseases:
- Age-related changes in valve leaflets. Thus, in patients over 60 years of age, due to age-related changes in collagen and elastic fibers, the number of vessels feeding the latter decreases. As a result, the fibers in the heart valves acquire a coarse fibrous structure, which affects the function of the valves.
- Previous acute rheumatic fever, especially with repeated attacks (previously called rheumatism). When the valve is affected by bacteria (usually streptococci, hemolytic, viridans, etc.), infective endocarditis develops with an inflammatory process on the valves. When the valve is influenced by antibodies to this group of bacteria (usually GABHS - group A beta-hemolytic streptococcus), an inflammatory process on the valve is also formed, but of an autoimmune nature. People most often affected by rheumatism are those who often suffer from sore throats, tonsillitis, caries, chronic diseases of the ENT organs and those who have had scarlet fever. Infective endocarditis also develops in this category of patients, but it is more common in injection drug users.
rheumatic vegetations on the mitral valve
- Congenital features, for example, connective tissue dysplasia, Marfan syndrome, mitral valve prolapse. With these anomalies, initially the connective tissue in other organs differs from normal, and often leads to loss of function by the organ. For example, with Marfan syndrome, there is a disturbance in the anatomical and functional structure of other internal organs, including the heart. Mitral valve prolapse causes the leaflets to “sag” into the lumen of the heart chamber, and if linear fibrosis develops on such leaflets, the patient is likely to experience disturbances in intracardiac hemodynamics.
- Atherosclerosis of the aorta. The deposition of cholesterol plaques, in addition to harm to the coronary arteries and, in connection with this, a high risk of myocardial infarction, poses another danger. This is a lesion of the aortic root with subsequent deposition of calcium in the plaque. In addition to the wall of the aorta itself, its valves are affected, and aortic fibrosis develops.
- Previous myocardial infarction and acute inflammation of the heart muscle (myocarditis). Necrosis (cell death) or inflammation near the valve ring leads to the proliferation of sclerotic tissue in place of dead cardiomyocytes - a “scar on the heart” is formed. If in place of this tissue there were tiny vessels feeding the valve leaflets, naturally, they can no longer perform their function. Due to chronic hypoxia, fibrous tissue forms directly in the valve leaflets.
Diagnostic methods
Doing an ECG of the heart
The correct actions of a cardiologist when suspecting and diagnosing this disease will be approximately as follows. First, the doctor talks with the patient about his well-being and symptoms that alarm the patient.
Next, he will carefully study his medical history and the results of laboratory tests (general urine test, complete blood count, blood test for sugar and cholesterol). Then the doctor will draw a conclusion about the necessary methods for further diagnosing the disease.
He may prescribe a chest X-ray for the patient to see the extent of changes in the heart and throughout the cardiovascular system, and echocardiography, which will show the exact location and degree of development of the scars that have appeared on the valve.
Also effective methods for determining this disease are catheterization and ECG.
These diagnostic measures reveal not only the degree of development of fibrosis, but also the presence in the body of a sick person of inflammatory processes and viral infections, which can complicate the course of the underlying disease, and which must be taken into account when prescribing treatment.
How does heart valve fibrosis manifest?
Due to the fact that the mitral and aortic valves are most often susceptible to the growth of fibrous tissue, it makes sense to dwell in more detail on the clinical manifestations of these valves.
Fibrosis of each valve may not be clinically evident if the valve ring is narrowed slightly (so-called non-critical valve stenosis). If fibrosis leads to valve insufficiency, regurgitation is formed - a reverse flow of blood into the atrium (with damage to the mitral valve) or into the left ventricle (with fibrosis of the leaflets or aortic root). Regurgitation can be moderate or significant, and depending on this, the patient may experience certain symptoms.
Signs of mitral valve fibrosis
fibrosis, calcification and stenosis of the mitral valve
In most cases, fibrosis of the mitral valve leaflets occurs over several years, during which the patient feels satisfactorily, without noting any subjective complaints from the heart. Subsequently, with further involvement of the connective tissue of the valve in the fibrotic process, the patient develops the following symptoms:
- Increased fatigue during normal physical activity, previously well tolerated by the patient,
- The occurrence of attacks of shortness of breath, suffocation, a feeling of lack of air, periodically or constantly noted at rest,
- Feelings of interruptions in the work of the heart (usually like extrasystole or atrial fibrillation),
- Pain in the chest, reminiscent of angina pectoris,
- Periodically occurring swelling of the lower extremities, especially in the morning, after a long horizontal position of the body.
aortic valve fibrosis
What happens with aortic valve fibrosis?
Damage to the aortic valve, whether it is stenosis of the leaflets or aortic root due to fibrosis of the aortic valve, or insufficiency of its leaflets, causes less than normal flow of arterial blood to other organs, including the brain. This provokes general severe weakness, attacks of loss of consciousness, attacks of angina pectoris due to depletion of coronary blood flow, and can also lead to the development of pulmonary edema.
Fibrosis of the mitral valve leaflets
Fibrosis of the mitral valve leaflets is a rather dangerous and serious condition. The reasons for its occurrence are very diverse. It is worth considering them in more detail.
Causes
Quite often, this disease appears after the patient has suffered a myocardial infarction. A common cause is age-related changes in the human body. Over the years, tissues and organs wear out. Heart tissue and urinary tract can be damaged due to hormonal changes, rapid slowdown of metabolism, etc.
- Life against the tide. Mitral valve prolapse and what is behind it
Mitral valve fibrosis can also be caused by the following reasons:
- Hypertension.
- Lung dysfunction.
- Heart defects.
- Infectious or viral infection of the connective tissues of the heart.
- Strong physical activity, etc.
This disease, in the absence of timely intervention by specialists, can develop into myocardial fibrosis. Otherwise it is called myocardiofibrosis.
Diagnosis of heart valve fibrosis
In cases where fibrosis is mild and occurs without significant symptoms, the doctor can rely on these minor manifestations and on examination data to prescribe a specific follow-up plan for the patient. Routine diagnostics (blood tests, urine tests, ECG) and instrumental research methods are usually prescribed. These include the following:
- Ultrasound of the heart is the most informative study, as it allows you to visualize the smallest internal structures in the heart and reliably assess the degree of fibrosis, the degree of narrowing of the valve ring or the degree of regurgitation. The contractile function of the left ventricle and the ejection fraction are also assessed, that is, the amount of blood that actually enters the aorta, and how much it differs from the proper amount.
- X-ray of the chest organs. Informative in case of venous congestion in the pulmonary tissue, when the configuration of the heart changes, for example, with an enlargement of the atrium or ventricle. An experienced radiologist can always tell which camera is supposedly expanding the cardiac shadow in the image.
- Coronary angiography (CAG, or the so-called “coronary angiography”) is not performed on all patients, but only on those who are planned for surgical treatment for valve replacement. In addition, CAG is indicated for patients with concomitant ischemic heart disease, but the corresponding indications are identified.
Any of the research methods is prescribed by a doctor based on the results of an in-person examination. It happens that a patient notes characteristic complaints of weakness, fatigue, shortness of breath, etc., and the doctor does not see any indication for examination, since such symptoms can be caused by anything, from chronic fatigue syndrome and overload at work to pathology nervous system. In this case, the patient can perform an electrocardiogram and ultrasound of the heart at his own expense in paid clinics, even if only for self-soothing, since there will definitely be no harm from these techniques.
Fibrosis and CHF. Controversial issues
00:00
Vladimir Trofimovich Ivashkin, Academician of the Russian Academy of Medical Sciences, Doctor of Medical Sciences:
— Now we move on to the next message. Oksana Mikhailovna Drapkina will report on the connection between fibrosis and diastolic chronic heart failure.
Oksana Mikhailovna Drapkina , professor, doctor of medical sciences:
— Thank you very much, Vladimir Trofimovich. I will begin my lecture with a clinical observation. Using the clinical example of a patient, I will try to analyze whether this ligament exists at all (fibrosis and impaired diastole), or whether it is still necessary to look for some other ways and other mechanisms for the development of these two conditions.
(Slide show).
A patient who is in the cardiology department. She is 56 years old. She complains of increased blood pressure to 200 and 100 mmHg. Art., pain in the heart, shortness of breath when walking, decreased exercise tolerance and numbness in the tips of the fingers and toes.
From the anamnesis. The key points are that she suffers from both diabetes and hypertension. Moreover, she has a long history of suffering from arterial hypertension and diabetes mellitus. She controls glycemic levels with insulin and Amaryl. She had already undergone surgery for stenosis of the left coronary artery. The deterioration of the condition is observed within three months.
(Slide show).
This patient is obese. She has abdominal obesity. Body mass index exceeds 30 kg/m?. An objective examination reveals that she is a hypertensive patient with experience, since the boundaries of the relative dullness of the heart are shifted. The accent of the 2nd tone is pronounced over the aorta.
At the time of admission, the pressure is 190 and 110 mmHg. Art. Just by the level of blood pressure, we can see that this is a very high-risk patient. She definitely has stage 3 hypertension.
(Slide show).
Electrocardiographic examination showed sinus rhythm. There are signs of increased atrial activity. We see a P that is both tall and somewhat broad. For example, in V1 we see a negative phase of the P wave, which suggests that this patient also has atrial overload.
(Slide show).
We perform an echocardiographic study. I deliberately left a little bit of her clinical and biochemical blood tests as a snack.
Let me remind you that this is a woman. Her main complaints are shortness of breath and increased blood pressure. She has low exercise tolerance. Before doing the echocardiographic examination, we performed a 6-minute walk test. It doesn't reach 550 meters. This classifies her as heart failure of functional class 3 according to the New York classification.
An echocardiographic study reveals a normal ejection fraction. Severe left ventricular hypertrophy: interventricular septum and posterior wall 1.2 and 1.3. Increased pressure in the pulmonary artery. High or threshold (even above threshold) volumes of the left atrium and right atrium.
Signs that indicate that there is impaired diastole. For example, according to the latest European algorithm, E/e = 10, which places the patient in the gray zone of patients with a presumptive diagnosis of diastolic heart failure. Her natriuretic peptide levels are higher than normal.
04:03
What else is important when analyzing an echocardiogram? The left atrial function index, that is, the contractile function of the left atrium (which we can also determine), is reduced in her. We now determine the fibrosis fraction for almost all of these patients. 26% fibrosis fraction, which is determined by the most echogenic areas. We identified epicardial fat in such a patient. Its thickness is 9 mm.
(Slide show).
Having analyzed everything that we know at that time, we can say that this patient:
- preserved ejection fraction;
- left ventricular hypertrophy;
- signs of fibrosis, which we identified using video densitometry;
- epicardial fat 9 mm thick.
Let's dwell on each of these points.
05:00
We are talking about a patient with so-called heart failure with preserved ejection fraction. With some discretion, I will call it diastolic heart failure.
Its prevalence is great. According to some studies, it accounts for up to 2/3 of all cases of chronic heart failure.
(Slide show).
Previously, it was believed that diastole remains in the shadow of its more successful friend systole, and all clinical manifestations in a patient of heart failure are characterized by the fact that systole is impaired. Many studies prove that this is not entirely true.
If we look at days and compare the survival of patients with reduced ejection fraction versus preserved ejection fraction, there is of course a significant benefit to normal preserved ejection fraction. When the count goes over the years, there is an almost identical prognosis in patients with normal and reduced left ventricular ejection fraction.
(Slide show).
The New England Journal of Medical published data that suggests that we have become quite good at treating and developing treatment algorithms for patients with systolic heart failure. The prognosis has improved over the years. The analysis has been carried out since 1987. The last period is from 1997 to 2001. The prognosis is improved in patients with reduced left ventricular ejection fraction during treatment.
This is not observed in patients with preserved ejection fraction. Apparently, the point is that we have not yet completely figured out how to treat patients with diastolic heart failure.
06:54
(Slide show).
If we recall a little pathophysiology and once again return to the pressure/volume “curve” in the left ventricle (this is the norm), then we can say that the systole phase begins with the closure of the mitral valve. But it still takes some time before the aortic valve opens.
This characterizes the time of isovolumic contraction. Here the volume is fixed, it does not change, but the pressure increases sharply. The pressure reaches a critical value. This causes the aortic valve to open, forcing blood into the aorta. At the same time, the pressure in the left ventricle continues to increase, but not so rapidly - we see the expulsion phase.
With the closure of the aortic valve, the very phase or cycle that interests us most today begins - this is the diastole phase. The earliest part of this phase is represented by the isovolumic relaxation phase.
Hypodynamically, the change in pressure in the cavity of the left ventricle occurs at a fixed volume. And biochemically (if we go a little deeper), this phase is represented by the active relaxation of cardiomyocytes.
The timing of the isovolumic relaxation phase, the so-called “TAU,” is very important here. This is the time during which pressure in the left ventricle decreases during isovolumic relaxation.
The graph is two-dimensional, so we cannot show the value of "TAU", but it is absolutely and definitely possible to say that this value is extremely important.
Then the filling phase begins. It is represented by passive relaxation of the left ventricle and atrial systole. This all happens before the mitral valve closes. It is very important that the end of diastole occurs at a slightly positive end-diastolic pressure.
(Slide show).
With systolic dysfunction, the “curve” shifts downward and to the right, reflecting a decrease in left ventricular ejection fraction. And in our patient, about whom we started talking, a slightly different modification of the pressure/volume “curve” occurs. It all starts with an increase in end-diastolic pressure.
This graph shifts slightly to the left: the ejection fraction is preserved, the stroke volume is changed. Thus, it is not a simple shift of the “curve” that occurs, but the “TAU” time during which the pressure decreases increases.
09:49
(Slide show).
The second point that we saw in this patient was left ventricular hypertrophy. Left ventricular hypertrophy is well known. Most often this is symmetrical hypertrophy of the left ventricle. Our patient has almost the same. The interventricular septum is 13 mm, the posterior wall of the left ventricle is 12 mm.
The molecular pathways of left ventricular hypertrophy are also schematically presented on this slide. If we dive inside, right into the cardiomyocytes, we see very familiar characters: angiotensin II, tumor necrosis factor alpha, endothelin. As well as mechanical stretching, which we divided into weak and strong.
Angiotensin II, tumor necrosis factor alpha, endothelin and other agents, slight mechanical stretch lead to the activation of NADPH oxidase. It, through a kinase cascade, leads to the activation of protein synthesis, which contributes to the thickening of sarcomeres, and, most importantly, an effect on the calcium pump, which leads to to the fact that calcium is removed from the cell.
This is the efficiency of diastole. The better calcium is removed from the cell, the greater the ability of the myocardium to relax - the filling of the myocardium will be greater.
If the mechanical stretch is very strong (for example, with aortic valve insufficiency, when volume overload occurs), then beta-I receptors are activated. This leads to the activation of free radical damage and the release of cytochrome C. In turn, not the kinase, but the caspase cascade is activated. This leads to apoptosis of cardiomyocytes.
This is also hypertrophy, but eccentric hypertrophy. We observe such hypertrophy, for example, after myogenic dilatation, myocardial infarction or dilated cardiomyopathy.
It is paradoxical, but it is a fact that cardiomyocytes in patients with severe hypertrophy occupy less volume. A larger volume begins to fall on the role and destiny of the extracellular matrix.
(Slide show).
This occurs in such a way that the relationship between the extracellular matrix and the cardiomyocyte changes. First of all, the activity and ratio of matrix metalloproteinases and their inhibitors change.
12:43
The next point is the fibrosis fraction. In this patient, using video densitometry, it is higher than normal. This suggests that we should say a few words and raise the issue of fibrosis.
What it is.
(Slide show).
The definition can be given at two levels. This slide outlines the pathological and molecular definitions.
Let's start with the first one. What is meant by fibrosis? This is a compaction of connective tissue with the appearance of scar changes in various organs, usually resulting from chronic inflammation. Or we can say that it is an excessive accumulation of fibroblasts and extracellular matrix proteins in tissues.
(Slide show).
The main characters on the slide. These are fibroblasts. These are collagens, and here greater importance is given to collagen types I and III. These are components of the extracellular matrix: proteoglycans and various other agents.
Relationship between matrix metalloproteinases and their inhibitors. The profibrotic (the most important, in my opinion) active component is the growth factor TGF beta. It is by influencing it that many fibrotic processes are carried out.
14:06
(Slide show).
One of the main agents is collagen. Collagen is an extremely strong protein. It is so strong that its strength is even comparable to that of steel. It is a triple helix, which is formed by three elongated protein chains, and makes up almost 1/3 of all proteins in the human body.
Accordingly, collagen is needed. We know some diseases that are also characterized by pronounced and severe rhythm disturbances. Refers to connective tissue dysplasia syndrome, when the synthesis of collagen types I and III is disrupted. On the other hand, fibrosis is the predominance of collagen synthesis over its breakdown.
(Slide show).
Here is a diagram. It is not simply the mechanical predominance of collagen synthesis over its breakdown that matters. The process of collagen structuring is very important here. It is normal structural collagen that will influence fibrosis processes.
(Slide show).
We know the different types of fibrosis. Here on the first slide is reactive fibrosis and reparative fibrosis. Let's return to our patient again - she certainly has reactive fibrosis.
Cardiomyocytes are located side to side. Fields of fibrous tissue are marked in gray. Fields of fibrous tissue form and grow between them.
Reparative fibrosis (where apoptosis of cardiomyocytes plays a greater role) - we see a mosaic arrangement of fibrous tissue. It mainly replaces apoptotic, non-functioning cardiomyocytes.
(Slide show).
This is how it looks morphologically. We see interstitial fibrosis and perivascular fibrosis. I can guess (of course, this is just a guess), all the time relating to our patient, that most likely this patient has fibrosis of both.
(Slide show).
Familiar characters again. What we saw with left ventricular hypertrophy is the molecular mechanisms underlying its formation. The same agents are here - angiotensin II, TGF beta, aldosterone. It is not for nothing that we use all drugs that act on these systems in the treatment of patients with heart failure.
Inhibitors. I really want to pay attention not only to the well-known nitric oxide and prostaglandins, but also to bradykinin. We can only get it when we influence or treat our patient with angiotensin-converting enzyme inhibitors, and not with angiotensin receptor blockers.
The benefit here is double. It is clear that bradykinin is to blame for our patient’s cough. But bradykinin has many other positive qualities, which can sometimes overshadow a slight dry cough that does not interfere with the patient’s quality of life.
17:24
(Slide show).
This slide presents summary data about the main hormones and their effect on the process of fibroformation. These are growth hormone, thyroxine, angiotensin II and aldosterone.
It is the process of collagen accumulation that is largely influenced by angiotensin II. It promotes collagen synthesis and prevents collagen degradation. In this case, collagen accumulation occurs to a greater extent. Consequently, such patients are increasingly likely to develop fibrosis.
Aldosterone is also in second place. All drugs that reduce the level of aldosterone and spironolactone (we are now well aware of the emergence of mineralocorticoid inhibitor drugs) also have antifibrotic activity.
Thyroxine has no effect on collagen accumulation at all.
(Slide show).
This profibrotic coupling (angiotensin II and TGF beta) works well in cardiomyocytes. It is the effect of angiotensin II on TGF beta I that leads to the activation of fibroblasts, collagen and other proteins of the intercellular matrix, and fibrosis occurs. On the other hand, mechanical stretching works almost the same.
19:00
(Slide show).
But the liver tissue is also penetrated by blood vessels. The process of fibrosis in the liver also begins with nothing, namely with the vascular component, with the so-called capillarization of sinusoids. The basement membrane with the spaces of Disse loses its sinusoidal fenestrations. It is from this moment that fibrosis also occurs.
This means that in the liver there is something to act on for agents that reduce the activity of the renin-angiotensin-aldosterone system.
(Slide show).
Thus, today the key role of angiotensin II in the regulation of fibrogenesis in liver tissue has already been completely proven. Today, the potential of angiotensin-converting enzyme inhibitors and ARBs is being very seriously studied in terms of their antifibrotic effect.
Much more is known about these effects in the myocardium. I will give just a few of them:
? decreased production of extracellular matrix proteins. This has been proven in patients with arterial hypertension, coronary heart disease, and chronic heart failure;
? decreased production of TGF beta and increased tissue inhibitors of type I metalloproteinases, in particular;
? increasing coronary reserve by reducing the degree of media fibrosis and perivascular fibrosis.
(Slide show).
The last thing about this patient, in her analysis of cardiac affairs, cardiac problems. Epicardial fat. Whether it matters or not.
Yes, it is important. It is a new surrogate marker for cardiovascular disease. Many researchers have been and are evaluating it.
Let's return to our patient again. We remember that her epicardial fat layer is 9 mm. It falls under the last box. This patient clearly has insulin resistance, metabolic syndrome, and is many times more likely to develop cardiovascular complications, namely acute coronary syndrome.
21:05
There are many parallels in the development of fibrosis of both the liver and heart. The connecting point is fat in the heart, fat in the liver. Please note, dear colleagues, that the clinical predictors of the development of liver fibrosis and cardiac fibrosis are the same. These are age, increased body mass index, diabetes mellitus, pro-inflammatory agents (like C-reactive protein) and altered lipid profile.
Thus, today, with a certain degree of assumption, we can talk about a new predictor of cardiovascular diseases, namely non-alcoholic fatty liver disease. It increases the risk of carotid atherosclerosis. It, regardless of the presence of metabolic syndrome and diabetes mellitus, promotes thrombosis, which serves as a predictor of cardiovascular diseases in both men and women.
Let's return to our patient and look at her blood test. The blood test shows atherogenic dyslipidemia and an increase in transaminase levels above three normal levels. This patient needs statins. They are required.
High risk patient. She has a 30% plaque at the bifurcation of the right common carotid artery. Her intima-media complex thickness is also greater than normal (1.1 mm). Thus, statins are needed.
What to do with her transaminases? Nothing to do. We need to make sure they fit three times the size. Then, statins are not only contraindicated for such a patient. The liver of such a patient needs protection with statins. There are convincing facts about this.
Which statin to choose. Probably safe, studied. In general, in my opinion, there are practically no dangerous statins. However, if you take the position of evidence-based medicine, the hydrophilic statin Rosuvastatin immediately comes to mind. It showed its complete safety in the CORONA study (these are very elderly patients) and in the JUPITER study.
(Slide show).
There are high-quality generics. We are now gaining experience in using these drugs. In particular, the drug "Mertenil", which is very well tolerated by patients with such a tangle of problems.
(Slide show).
We have developed an algorithm for the treatment of dyslipidemia in patients who come to us with a high risk of cardiovascular complications and at the same time have transaminase levels greater than three norms.
We give such patients Ursodeoxycholic acid (UDCA) for three weeks and carefully follow the dietary recommendations.
As a rule, the level of transaminases is included in the three-normal reserve. Then we have every reason to give such patients Rosuvastatin.
with UDCA. This patient has the antifibrotic and hypocholesterolemic effect of Ursosan.
will also be “on hand”.
24:25
(Slide show).
The latest publication in 2012 showed that the potential of UDCA is very interesting and does not only fall within the framework of improving liver parameters. For example, against the background of Ursosan, an improvement in blood flow by 18% was noted using plethysmography.
(Slide show).
Thus, the patient is very high risk. Such a patient should immediately begin with combination therapy. Combined antihypertensive therapy:
• ACE inhibitor potassium blocker drug “Equator” (well known) was prescribed;
• “Veroshpiron” is an antifibrotic drug that is essential in the treatment of heart failure;
• "Ursosan";
• when the level of transaminases reached, allowing statins to be given, Mertinil was prescribed (we gave 10 mg, no more);
• antiplatelet agents.
What remains beyond the scope of today’s discussion is that vascular fibrosis in this patient also needs to be discussed.
This patient naturally has perivascular fibrosis secondary to diabetes mellitus. This is a separate very interesting topic. We often find normal, clear coronary arteries in patients with diabetes, and anginal pain may be associated with extravasal compression of the coronary arteries.
The prospects are interesting. The hypothesis about the use of relaxin is currently being tested. Regarding statins, I think we will meet again. There are very different data on the effect of statins on fibrosis.
Protein cross-link disruptor alagebrium.yu Phospholipase D inhibitor and genetic therapy are now used. Probably, taking into account all those perspectives, this tale is about the little humpbacked horse, when the question of the elixir of youth was first raised. And fibrosis or the absence of fibrosis and normal blood vessels - it seems to me that this formula for the elixir of youth will come true.
How to treat cardiac fibrosis and can it be cured completely?
If the fibrosis of the valves is not so severe as to lead to significant stenosis or regurgitation, the patient does not require treatment. Annual monitoring by a cardiologist with regular echocardioscopy is sufficient. But if the patient has other diseases of the heart and blood vessels - arterial hypertension, atrial fibrillation, myocardial ischemia, selection of therapy is required according to the nature of the disease.
If the fibrosis is significant and has led to the development of severe heart failure, in most cases it is necessary to take cardiac glycosides and diuretics (diuretics). Digoxin is usually prescribed at a dosage of 0.25 mg, 1/2 tablet twice a day, five days a week (two days off) continuously or until the clinical situation improves. Of the diuretics, preference is given to indapamide (1.5 or 2.5 mg in the morning), and in more pronounced stages - veroshpiron (25 or 50 mg in the morning), diuver (5 or 10 mg in the morning) and furosemide (20-80 mg in the morning).
When a patient has significant fibrosis leading to grade 2, 3 and 4 valve ring stenosis, valve replacement surgery or surgical dissection of adhesions (commissurotomy) is necessary. Currently, operations can be performed both on the open heart using a heart-lung machine, and through intravascular access, through large peripheral arteries (inguinal, femoral, etc.). Typically, modern mechanical prostheses made of synthetic materials are used. Biological prostheses (from pig valves) are used less frequently. When valve leaflet insufficiency develops, either surgical valve repair with suturing of non-closing leaflets or valve replacement is indicated.
Unfortunately, fibrosis of the heart valves cannot be cured permanently with medications, since it is almost impossible to treat scar tissue with medications. The consequences of fibrosis can be eliminated surgically, but the indications for surgery must be determined strictly individually. In the case where the patient has minor fibrosis that does not lead to stenosis or insufficiency, it is recommended to lead a healthy lifestyle, eat well, regularly see a cardiologist (or cardiac surgeon) and take all prescribed medications, and then it is likely that the operation will be successful. won't be needed for the next few years.
Are there possible consequences?
Yes, with cardiac fibrosis, there is a high probability of adverse consequences sooner or later. The likelihood of their occurrence is determined by the reason why fibrosis initially occurred. Thus, the formation of heart defects after rheumatism is more common than the formation of failure or stenosis due to myocardial ischemia and a heart attack. Again, atherosclerosis of the aortic walls with the deposition of calcium in them more often leads to the formation of non-rheumatic heart disease than previous myocarditis, for example. Therefore, it is possible to predict whether valve stenosis or insufficiency will develop after a particular disease, but with great caution.
Prevention of the development of defects in valve fibrosis is the correct and timely treatment of the underlying disease that led to fibrosis or cardiosclerosis.
Forecast
The prognostic value of valve fibrosis is determined primarily by the presence or absence of consequences. Thus, fibrosis without pronounced stenosis or without regurgitation has a favorable prognosis, while hemodynamically significant heart defects resulting from fibrosis and leading to severe heart failure have an unfavorable prognosis. In the latter case, everything depends on the timeliness of the operation - if the operation is performed on time, and the surgeon has caught that fine line when the operation is already indicated, but not yet contraindicated - the duration and quality of life of the patient increases.