Liver diseases + high blood pressure
Many hypertensive patients with liver disease try to take as few pills as possible in order to “spare the diseased liver.” But hypertension is a disease no less dangerous than hepatitis or fatty liver.
Article on the topic How to help the liver after a vacation? Suitable treatment can be found. You just need to carefully develop a tactic together with an experienced doctor. Now there are a number of drugs for hypertension that have virtually no effect on the liver.
Hypertensive patients must also take hepatoprotectors in courses. This class of drugs protects the liver from drug load.
See also: Medicine for the liver →
With this combination of diseases, herbal medicine is useful. Raisins, chokeberries, cherries, black currants, dried apricots, and watermelons will be useful both for the liver and for normalizing blood pressure. Instead of regular tea and coffee, it is advisable to drink decoctions of rose hips, hawthorn, as well as teas from peppermint and lemon balm leaves.
Why does liver failure occur?
In case of liver failure, it is important to carry out treatment aimed at its cause. Therefore, the doctor must conduct a thorough examination and figure out what led to liver dysfunction in the patient.
The most common cause of liver failure is cirrhosis, a condition in which normal liver tissue dies and is replaced by fibrous tissue. The most common causes of cirrhosis include viral hepatitis B and C and chronic excessive alcohol consumption. The cause of liver failure can be non-alcoholic fatty liver disease (NAFLD) - excessive accumulation of fats in the organ tissue. NAFLD often accompanies diabetes mellitus and metabolic syndrome (high blood pressure, obesity, elevated levels of glucose and cholesterol in the blood). According to experts, 1.46 billion adults currently suffer from this pathology worldwide.
The most common causes of acute liver failure:
- Viral hepatitis.
- Taking certain medications: antifungals, anticonvulsants, antibiotics, synthetic hormone analogues, antidepressants, using acetaminophen (paracetamol) frequently or in large doses.
- Taking certain substances and dietary supplements, such as green tea extract.
- Autoimmune hepatitis is a disease in which the immune system is disrupted and antibodies against liver cells ( hepatocytes
) begin to be produced. As a result, chronic inflammation develops in the liver tissue. - Wilson's disease is a congenital disease in which copper metabolism is disrupted and severe damage to the central nervous system, liver and other internal organs develops.
- Other diseases associated with metabolic disorders and damage to blood vessels.
Liver disease + gallstones
| Important | |
When combining liver diseases with any other ailments, you should adhere to the following recommendations:
| |
Gallstone disease is a direct threat to liver health. After all, if a small pebble moves out of place and clogs the duct, the bile will have nowhere to go. Jaundice will appear, and liver cells will begin to quickly deteriorate. So you shouldn’t delay deciding on surgery to remove stones.
In some cases, the problem can be dealt with without the help of a surgeon. In recent years, drugs with dual action have appeared. They dilute bile, dissolving sand in the gallbladder, and at the same time protect the liver from damage.
In addition, when hepatitis is combined with cholelithiasis, it is advisable to avoid herbal preparations with a choleretic effect. They force the liver to work with redoubled force, producing bile. But overloading liver cells can lead to their death, and the likelihood of small pebbles getting into the ducts also increases.
Article on the topic
Alcohol, drugs or overeating? What leads to fatty liver With this combination of diseases, proper nutrition is very important. You need to eat often, 4–6 times a day. Dinner should be light - no more than 20% of the total food. All products are best consumed warm. It is undesirable to eat fatty pork, caviar, goose and duck meat, egg yolk and fatty dairy products. Buckwheat, oatmeal and other porridges, low-fat cottage cheese and kefir are useful both for the liver and for the composition of bile.
Arterial hypertension (AH) in the Russian Federation (RF), as in all countries with developed economies, is one of the pressing medical and social problems. This is due to its high prevalence, high risk of complications and insufficient control on a population scale. The prevalence of hypertension among the adult population is approximately 40%, which determines a high incidence of cardiovascular complications (CVC), including deaths [1, 2]. Arterial hypertension is a leading factor in the high mortality rate of the population from diseases of the cardiovascular system, increasing the risk of developing coronary heart disease (CHD) and stroke by 3–4 times [3, 4].
According to the results of a study conducted within the framework of the targeted federal program “Prevention and Treatment of Arterial Hypertension in the Russian Federation,” the prevalence of hypertension among the population in 2009 was 40.8% (in men – 36.6%, in women – 42.9% ). Awareness of patients with hypertension about the presence of their disease is 83.9–87.1%. 69.5% of patients with hypertension take antihypertensive drugs (AHD), of which 27.3% are effectively treated, and blood pressure (BP) is controlled at the target level in 23.2% [5].
The main goal of treating patients with hypertension is to minimize the risk of developing cardiovascular complications and death from them. Achieving this goal requires reducing blood pressure to the target level, correcting all modifiable risk factors (smoking, lipid metabolism disorders, hyperglycemia, obesity), preventing, slowing the rate of progression and/or reducing target organ damage, as well as treating associated and concomitant diseases ( IHD, diabetes mellitus – DM, etc.).
The recommendations of the All-Russian Scientific Society of Cardiology [6] note that the target blood pressure level should be less than 140/90 mm Hg. Art., and if the prescribed therapy is well tolerated, it is advisable to reduce blood pressure to lower values.
Patients with a high and very high risk of cardiovascular disease need to reduce blood pressure to 140/90 mmHg. Art. or less within 4 weeks. If well tolerated, a further reduction in blood pressure to 130–139/80–89 mmHg is recommended. Art. When carrying out antihypertensive therapy, it should be borne in mind that it may be difficult for patients with diabetes, elderly patients and people who already have cardiovascular disease to achieve a systolic blood pressure level < 140 mmHg. Art. If blood pressure reduction is poorly tolerated, it is recommended to achieve the target blood pressure level in several stages. At each stage, blood pressure is reduced by 10–15% of the initial level over 2–4 weeks, followed by a break to allow the patient to adapt to lower blood pressure values. The next stage of lowering blood pressure and, accordingly, increasing antihypertensive therapy (namely increasing the dose and/or number of drugs taken) is possible only if the already achieved blood pressure values are well tolerated. If moving to the next stage causes the patient's condition to worsen, it is advisable to return to the previous level for some more time.
Thus, a decrease in blood pressure to the target level occurs in several stages, the number of which is individual and depends on both the initial blood pressure level and the tolerability of antihypertensive therapy. The use of such a step-by-step scheme for lowering blood pressure, taking into account individual tolerance, especially in patients with a high and very high risk of cardiovascular disease, allows one to achieve the target blood pressure level and avoid episodes of hypotension, which are associated with an increased risk of myocardial infarction and stroke. When achieving the target blood pressure level, it is necessary to take into account the lower limit of reducing SBP to 110–115 and DBP to 70–75 mm Hg. Art., and also ensure that during treatment there is no increase in pulse blood pressure in elderly patients, which occurs mainly due to a decrease in DBP [6].
Currently, five main classes of antihypertensive drugs are recommended for the treatment of hypertension: angiotensin-converting enzyme inhibitors (ACEIs), angiotensin II receptor antagonists (ARAs), calcium channel blockers (CCBs), β-blockers (β-blockers), diuretics (see table). Alpha-blockers, imidazoline receptor agonists, and direct renin inhibitors can be used as additional classes of combination therapy.
When choosing a drug, the doctor must take into account many factors, the most important of which are the presence of risk factors in the patient; target organ damage; associated clinical conditions, kidney damage, MS, diabetes and other concomitant diseases that limit the use of antihypertensive drugs:
- the patient’s previous individual reactions to drugs of various classes;
- the likelihood of interaction with medications prescribed to the patient for other reasons;
- socioeconomic factors, including the cost of treatment.
When choosing an antihypertensive, it is first necessary to evaluate the effectiveness, likelihood of side effects and benefits of the drug in a specific clinical situation. From the results of multicenter randomized trials, it follows that none of the main classes of antihypertensive drugs has a significant advantage in terms of both lowering blood pressure and the effectiveness of reducing the risk of cardiovascular events and death from them. When prescribing any of the main classes of antihypertensive drugs, there are pros and cons.
In each specific clinical situation, it is necessary to take into account the peculiarities of the action of antihypertensive drugs of various classes, discovered during randomized studies. The choice of one or another antihypertensive should be based on the results of large clinical studies, which have proven the high effectiveness and safety of patients using this particular drug in a similar clinical situation.
However, recommended standards and programs for the treatment of hypertension do not always take into account the state of the digestive organs, although the metabolism of many drugs begins and occurs there. According to the TsNIIG data for three years (1999–2001), 1200 patients with liver cirrhosis (LC) were examined and treated in hepatology departments, among them, hypertension stages I–III occurred among 18.4% of patients (almost every 5th patient CP had hypertension).
All groups of drugs used in the treatment of hypertension have different effects on the digestive organs. These can be positive effects. For example, the use of β-AB for the prevention of bleeding from varicose veins of the esophagus in cirrhosis, BCC in achalasia cardia. The negative effects of cardiac drugs are also known: erosive and ulcerative lesions of the stomach when using acetylsalicylic acid, increased manifestations of gastroesophageal reflux disease when taking CCBs (a group of dihydropyridines). In this regard, rational pharmaco- and sometimes multi-target monotherapy is necessary (the ability to use the systemic effects of one drug to simultaneously correct the impaired functions of several organs or systems).
In patients with chronic liver diseases, fat-soluble drugs can accumulate, causing undesirable effects, while the concentration of water-soluble drugs in patients without hepatorenal syndrome remains close to the standard [7–9]. In case of liver diseases, prodrugs in recommended doses cannot provide a sufficient hypotensive effect in patients with hypertension, and to achieve the target blood pressure level, an increase in single and daily doses of the drug is required. Therefore, when treating hypertension in people with pathologies of the digestive organs, it is necessary to take into account all the pharmacological features of antihypertensive drugs of various groups.
Thiazide and thiazide-like diuretics are divided into two generations. The first includes benzothiadiazine derivatives (hydrochlorothiazide) and chlorthalidone, the second generation includes chlorobenzamide derivatives (indapamide). Thiazide diuretics are poorly metabolized in the liver and are almost completely excreted unchanged by the kidneys. Unlike thiazide diuretics, indapamide is metabolized in the liver, so it should be used with caution in the treatment of hypertensive patients with liver pathology. Strict control is indicated for patients with cirrhosis, especially with edema or ascites, since the risk of developing metabolic alkalosis increases and the manifestations of hepatic encephalopathy may increase.
On the other hand, long-term use of diuretics by patients with magnesium deficiency due to impaired magnesium absorption (vomiting, diarrhea, alcoholic liver damage, intestinal resection) can lead to hypomagnesemia, in which the level of magnesium in the blood serum drops below 0.75 mmol/l. In this regard, when treating with diuretics, it is necessary to control the level of magnesium in the blood for these concomitant diseases.
The second group of antihypertensive drugs includes CCBs, which are indirect vasodilators. The general property of CCBs is lipophilicity, which explains their good absorption (90–100%) in the gastrointestinal tract (GIT), and the only route of elimination from the body is metabolism in the liver. In the liver, CCBs are completely metabolized to inactive metabolites, which are excreted through the kidneys and gastrointestinal tract. These general pharmacokinetic properties of CCBs explain the slowdown in their elimination from the body with age, with liver dysfunction, but practically does not change with renal failure. Therefore, for persons over 60–65 years of age and patients with cirrhosis, it is recommended to reduce the single dose or frequency of taking CCBs.
On the other hand, CCBs reduce the tone of the lower esophageal sphincter [10, 11]. If the function of the lower esophageal sphincter is impaired, there is no complete barrier to the reflux of acidic stomach contents into the esophagus, which can lead to the development of esophagitis. Since the reflux of acidic gastric contents into the esophagus can cause bleeding from varicose veins (gastroesophageal reflux is especially dangerous for patients with cirrhosis), the use of dihydropyridines is undesirable for cirrhosis complicated by esophageal varices [12].
The third group of antihypertensives includes β-ABs, which, depending on their solubility in fats and water, are divided into fat-soluble (or lipophilic), water-soluble (hydrophilic) and fat-soluble. Lipophilic β-AB (betaxolol, carvedilol, metoprolol, propranolol, timolol, nebivolol, etc.) are quickly and completely (more than 90%) absorbed from the gastrointestinal tract and are usually metabolized in the liver (80–100%) [13–15].
In the liver, they undergo metabolism by hydroxylation and conjugation, turning into metabolites that are excreted by the kidneys after conversion to water-soluble substances. In patients with cirrhosis with reduced hepatic blood flow and hepatocellular failure, these drugs are capable of accumulation in the body, since they remain in the blood for a longer time due to a decrease in the activity of liver enzymes, causing a higher frequency of side effects [16–20]. For this reason, single doses or frequency of administration of lipophilic β-blockers should be reduced for persons with reduced hepatic blood flow (i.e., for elderly persons, patients with heart failure or cirrhosis).
Hydrophilic β-AB (atenolol, nadolol, sotalol, etc.) are incompletely (30–70%) and unevenly absorbed in the gastrointestinal tract and are usually slightly (0–20%) metabolized in the liver, and therefore do not require dose changes and can therefore be used for the treatment of hypertensive patients with liver pathology. When using metoprolol in patients with cirrhosis, it is necessary to reduce the dose of the drug to avoid cumulative effects and associated side effects. The use of hydrophilic atenolol does not require dose adjustment [21].
Some drugs are soluble in both fat and water (acebutolol, bisoprolol, pindolol) and have two elimination routes - hepatic metabolism and renal excretion. This balanced clearance of these β-ABs ensures safety in the treatment of hypertensive patients with concomitant liver pathology and a low likelihood of their interaction with drugs that inhibit the activity of microsomal liver enzymes.
On the other hand, β-ABs can have a variety of effects on the functions of the digestive organs.
In particular, they reduce blood flow through the hepatic and mesenteric arteries, increase the tone of the lower esophageal sphincter, and increase peristalsis of the esophagus, stomach and intestines. The basis for the use of β-AB for gastroesophageal reflux and hiatal hernia is their ability to increase the tone of the lower esophageal sphincter and thereby prevent gastroesophageal reflux, as well as stimulate esophageal motility and reduce the incidence of reflux esophagitis. Back in 1980
D. Lebrec et al. reported that long-term use of propranolol at a dose that reduces heart rate by 25% reduces the risk of rebleeding from esophageal varices in patients with portal hypertension. According to summary data from various studies, long-term use of β-AB in patients with cirrhosis leads to a reduction in the number of episodes of first or recurrent bleeding by an average of 44% (compared to the control group), a reduction in mortality from bleeding by 42% and overall mortality by 24%. .
Preventive effectiveness (in particular, propranolol and nadolol) does not depend on the etiology and severity of cirrhosis. One of the proposed mechanisms for reducing pressure in the portal venous system may be a decrease in blood flow through the hepatic and mesenteric arteries as a result of decreased cardiac output (β1-blockade) and vasoconstriction (β2-blockade).
Other possible mechanisms include the following:
- increased tone of the lower esophageal sphincter, which leads, on the one hand, to a decrease in gastroesophageal reflux, and on the other, to compression of the collateral vessels supplying blood to the varicose veins;
- suppression of the activity of the renin-angiotensin system and the associated secretion of aldosterone, usually increased in cirrhosis, especially in the presence of ascites [22].
Therefore, β-ABs can be used to prevent bleeding from varicose veins of the esophagus. When the pressure in the portal vein is more than 12 mm Hg. Art. Beta-blocker therapy should be started regardless of the degree of venous dilatation, aiming to maintain the pressure at no higher than 12 mmHg. Art. [23].
Based on the above, we can draw the following conclusion: hydrophilic β-ABs are the drugs of choice for patients with hypertension and liver pathology.
The quadruple group of antihypertensive drugs includes ACE inhibitors. Despite the common mechanism of action, ACE inhibitors differ in chemical structure, the presence of additional functional groups in the molecule, the nature of the prodrug, activity and pharmacokinetic profile, which is very important to consider when treating patients with various pathologies of the digestive organs [24].
Currently, the most well-known ACEIs are: captopril, enalapril, benazepril, fosinopril, lisinopril, moexipril, perindopril, quinapril, ramipril and trandolapril [25, 26]. In gastroenterological practice, the greatest interest is in the classification, which takes into account data on the physicochemical properties and pharmacokinetic characteristics of ACE inhibitors. The liver is the main site of biotransformation of inactive ACE inhibitors into active diacid metabolites. Therefore, severe liver disease may have a significant impact on the pharmacokinetics of inactive inhibitors. For example, in patients with cirrhosis, the maximum concentration of quinapril is reduced by 70%. Theoretically, the safest drugs for cirrhosis are quinapril and lisinopril, which are not metabolized in the liver. In this regard, the use of antihypertensive drugs that are not metabolized in the liver and can provide patients with hypertension and gastrointestinal pathology with adequate blood pressure control within 24 hours becomes especially relevant [27].
In severe liver diseases, not only the biotransformation of inactive ACE inhibitors decreases, but also the conversion of their active diacid metabolites into inactive compounds. Therefore, it is difficult to predict changes in plasma concentrations of active diacid metabolites of various inactive ACE inhibitors in patients with cirrhosis. For example, in contrast to quinapril, plasma concentrations of trandolapril's diacid metabolite, trandolaprilat, are higher in patients with liver pathology than in healthy individuals. Therefore, in patients with cirrhosis, it is recommended to increase the dose of quinapril, but reduce the dose of trandolapril.
Lipophilic ACE inhibitors (captopril) have independent pharmacological activity, but undergo further transformations in the liver to form pharmacologically active disulfides, which are eliminated by renal excretion. Lipophilic prodrugs (pharmacologically inactive) become active diacid metabolites after metabolism in the liver, then are transformed into inactive compounds [28]. In individuals with liver pathology, both of these processes are impaired, and with a decrease in blood flow in the liver, there is a delay in the conversion of the prodrug to its active form during the first passage through it [29]. Accordingly, in liver diseases, drugs that require transformation to acquire activity have a weaker effect [30].
ACE inhibitors of this class are divided into three subgroups depending on the predominant route of elimination of their active diacid metabolites:
- subclass A – drugs with predominantly renal elimination;
- subclass B – drugs with two main elimination routes;
- subclass C – drugs with predominantly hepatic elimination.
Hydrophilic drugs (lisinopril) are not metabolized in the patient’s body, circulate in the blood in a form not bound to plasma proteins, and are eliminated unchanged through the kidneys. Their concentration in the blood plasma is determined by the dose taken, as well as the rate of absorption and the rate of excretion through the kidneys [31–33]. Lisinopril, being an active substance that does not require biotransformation in the liver, is the drug of choice for patients with liver pathology (which is often found in MS) and does not require dose adjustment. It has a prolonged antihypertensive effect. The onset of the antihypertensive effect is observed 1–3 hours after oral administration, the peak of action is after 6 hours, the duration of action is 24 hours with a stable effect after 2–4 weeks of treatment. Pharmacokinetic parameters after taking lisinopril by patients with cirrhosis and without liver pathology do not differ significantly. Thus, CP changes the pharmacokinetics of enalapril and does not affect the non-pharmacokinetic parameters of lisinopril [34, 35].
Some ACE inhibitors (captopril, lisinopril) directly have biological activity. All other ACEIs themselves are inactive substances, or prodrugs, i.e., they manifest their effect after biotransformation in the liver and the formation of active metabolites.
The next group of antigens includes angiotensin II receptor antagonists (ARAs). Depending on the presence of the active metabolite, ARAs are divided into prodrugs (losartan, candesartan, tazosartan), which become active after metabolic transformations in the liver, and active drugs (valsartan, irbesartan, telmisartan and eprosartan), which have pharmacological activity. Accordingly, in the treatment of hypertension in persons with liver pathology, preference is given to active ARAs, which are excreted unchanged. These drugs also do not affect the activity of hepatic cytochrome P450, which determines the low risk of interaction with other drugs (for example, ranitidine).
Thus, in case of pathology of the digestive organs, treatment of patients with hypertension with drugs that undergo hepatic metabolism should be carried out with caution. This is due to the fact that these drugs can remain in the blood of patients for a longer time, which can contribute to the development of adverse events [36, 37]. When treating hypertensive patients with liver pathology, it is important to use antihypertensive drugs that are not metabolized in the liver and do not worsen its functional state [38]. The most important task in the treatment of hypertensive patients with pathology of the digestive organs is the selection of the most effective antihypertensive drug, taking into account the functional state of the gastrointestinal tract.
Conclusion
Thus, according to the principles of rational pharmacotherapy (according to D.R. Lawrence), the doctor should, among many others, ask himself the following questions:
- What should be the drug treatment regimen, taking into account the functional state of the body (primarily the kidneys, liver)?
- Does the possibility of the intended improvement outweigh the likelihood of harm and the risk of side effects from the drug?
Liver diseases + back and joint pain
With exacerbation of arthrosis and osteochondrosis, painkillers from the group of non-steroidal anti-inflammatory drugs are often required.
But these drugs are not safe for the liver. Therefore, the fewer of these painkillers you take orally, the better.
To reduce the use of pain medications, consider physical therapy treatment. Properly selected courses of procedures provide both analgesic and anti-inflammatory effects.
Well, in cases where non-steroidal anti-inflammatory drugs cannot be avoided, take them “under the guise” of tablets to protect the liver - hepatoprotectors.
Instructions for travelers: how to save your liver on vacation >>
Modern approaches to treatment
Treatment for liver failure is aimed at combating the underlying disease, correcting pathological conditions caused by liver dysfunction, and preventing complications. Diet plays an important role.
The liver is often called the body's filter. In fact, this organ not only neutralizes toxic substances, but also performs a number of other important functions. When they are violated, certain symptoms occur:
- Synthesis of blood proteins. If they are not produced enough, then the fluid cannot be retained in the blood vessels, it rushes into the tissues, and edema occurs.
- Synthesis of proteins that take part in hematopoiesis. Violation of this function manifests itself in the form of increased bleeding.
- Bile synthesis and its excretion into the intestines. When liver tissue is damaged and/or bile flow is impaired, jaundice develops: the patient’s skin and whites of the eyes turn yellow.
- Storage of sugar in the form of a polymer - glycogen.
- Breakdown of saturated fats.
What is bile and why is it needed?
Bile is a secretion produced by hepatocytes. The color of bile ranges from light yellow to dark green. Bile contains bile pigments - bilirubin and biliverdin, cholesterol, fatty acids, lecithin, mucin.
Bile is the main participant in digestion. It neutralizes hydrochloric acid that enters the duodenum from the stomach, thereby creating favorable conditions for the action of pancreatic juice and parietal digestion in the jejunum.
Bile acids emulsify fats, allowing them to be absorbed in the intestines.
Bile has a bactericidal effect that prevents the proliferation of pathogenic microflora.
Liver transplantation
Liver transplantation may be indicated for both acute and chronic liver failure. This is the only radical treatment method. But there are a number of restrictions on its use. Firstly, this is a serious surgical intervention that not all patients can endure. Secondly, today there is a shortage of donor organs all over the world, and many patients wait a long time for their turn.
The decision to undergo a liver transplant is made in case of fulminant hepatitis (a rare serious condition in which a significant part of the organ tissue dies - can develop due to viral hepatitis, poisoning, drug overdose), if the patient is under 60 years old and has not previously had liver dysfunction.
Indications for transplantation in acute liver failure can be determined using the King's College Hospital criteria:
| If you overdose on acetaminophen (paracetamol) |
|
| For acute liver failure caused by other causes | Prothrombin time more than 100 s or three criteria from the list:
|
There are other systems of criteria, but they do not always help to fully assess the situation, so in each specific case the decision must be made individually. Statistics show that the average survival rate of patients with liver failure after liver transplantation within a year is 70–80%.
We will call you back
Message sent!
expect a call, we will contact you shortly
Postoperative period
In case of an uncomplicated course of the postoperative period, early activation of the patient is practiced, 3-4 hours after the operation. Eating is allowed on the second day. Discharge from the hospital occurs within 3-4 days, and depends on the individual threshold of pain sensitivity. Removal of sutures is not required, as skin wounds are sutured with cosmetic sutures and absorbable sutures.
A return to normal lifestyle and physical activity is possible within 10–14 days, after complete healing of skin wounds.
Appearance after laparoscopic cholecystectomy:
Ascites as a complication of cirrhosis
Very often, cirrhosis is accompanied by diseases that pose no less danger to life. One of these diseases is ascites or abdominal dropsy. With this disease, there is an excess of fluid in the abdominal cavity. It begins to put a lot of pressure on the organs, and for this reason the diaphragm is pushed aside, and this leads to disruption of normal cardiac activity. Abdominal dropsy is dangerous because it is impossible to absolutely predict when it will appear. Often the disease is diagnosed only when fluid in the body accumulates in such quantities that the abdomen protrudes and it becomes visible to the naked eye.
Ascites also appears in diseases of the digestive system, but if the cause is cirrhosis, then the disease can be activated literally in an instant, and after some time the abdominal cavity will be filled with fluid. If a person is sick with ascites, then he is given three years to live. If the patient takes care of himself and receives treatment, this will prolong his life by another five years. Until now, scientists do not understand how the disease begins to develop at a certain stage of cirrhosis.
How are the bile ducts arranged and how do they work?
The bile ducts are a system of ducts that originate from hepatocytes and gradually gather into interlobular, segmental and right and left lobar ducts, which unite into the common hepatic duct.
One of the stages of bile removal is its accumulation in the reservoir - the gallbladder. The main function of the gallbladder is to concentrate bile and release it into the lumen of the duodenum during digestion. The volume of this organ is about 80 ml.
The gallbladder is located on the lower surface of the liver. It is a hollow muscular organ, externally covered with a serous membrane and internally lined with mucous membrane. The structure of the gallbladder is divided into the bottom, body and neck of the bladder, which passes into the cystic duct.
Survival prognosis
The prognosis for liver failure depends on its type and nature of the course. In case of chronic liver failure during treatment, the condition significantly improves in 80% of patients, and in acute liver failure - only in 20–40%. In acute liver failure, the prognosis is worse in people under 10 and over 40 years of age, with viral hepatitis, and with jaundice that lasts longer than 7 days.
Treatment of liver failure must be comprehensive. The International Clinic Medica24 uses all modern techniques and medicines of the latest generations. The clinic has intensive care wards equipped with high-tech equipment for monitoring vital functions, performing mechanical ventilation and other procedures. Our experienced doctors approach the treatment of each patient individually, taking into account the reasons for the deterioration of liver function, the course of the disease, and disorders that develop in the body. We are ready to help at any time of the day; our clinic operates 24/7.
The material was prepared by a member of the international society of oncological surgeons EESG, candidate of medical sciences Sergeev Petr Sergeevich.
What questions can you ask the doctor at your appointment?
- Do I need surgery?
- Is it possible to dissolve stones?
- Why is it better not to dissolve stones?
- Is it possible to simply remove the stones and leave the bubble?
- How will my life change after cholecystectomy?
- Will there be dietary restrictions?
- Will it hurt after the surgery?
- What kind of anesthesia will it be?
- When can I eat fatty heavy foods and alcohol?
- Are dressings necessary after discharge from the hospital?
You can contact the clinic of coloproctology and minimally invasive surgery for diagnosis and treatment of gallstone disease. Thanks to modern operating rooms and highly qualified staff, the clinic provides all types of treatment for gallstone disease, including robotic surgeries.
Treatment under the compulsory medical insurance policy is possible.
Sign up for a consultation and receive quality treatment as soon as possible.
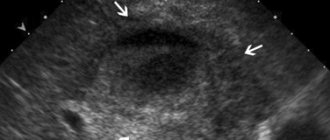
How to diagnose gallstone disease?
The gold standard for diagnosing gallstone disease is ultrasound examination of the abdominal cavity. This method allows you to identify stones in the gallbladder. Assess their size, shape and location. An important indicator is the thickness of the gallbladder wall. Normally, it does not exceed 2-3 mm. Thickening of the wall is an absolute sign of inflammatory changes - acute cholecystitis. An important criterion is the diameter of the common bile duct. If there are stones, its diameter increases from 3 – 6 to 20 mm.
Magnetic resonance imaging allows you to see the intra- and extrahepatic bile ducts, as well as the main pancreatic duct. This diagnostic method is used when there is a suspicion of the presence of stones in the common bile duct. This is necessary for treatment planning.
Multislice computed tomography is indicated for the development of acute biliary pancreatitis. This diagnostic method allows you to identify inflammatory changes in the pancreas and surrounding tissues.
Gastroduodenoscopy - this diagnostic method is especially valuable for complicated cholelithiasis, as it allows not only to evaluate the stomach, duodenum, but the flow of bile through the major duodenal papilla. If necessary, gastroduodenoscopy can easily be transformed from a diagnostic procedure into a therapeutic one. Using special instruments, you can “paint” the bile ducts and remove stones.
In the figure, the arrow indicates a stone in the common bile duct. Using a duodenoscope, a dissection of the sphincter of Oddi was performed in the duodenum. A radiopaque substance was introduced to allow visualization of the calculus. Using a special basket, the stone is captured and removed.