Anterior cerebral artery thrombosis syndromes
The anterior cerebral artery of the brain has two segments:
- precommunal (A1) segment of the circle of Willis, or stem, segment that connects the internal carotid artery with the anterior communicating artery
- postcommunal (A2) segment, originating from the connection of the A1 segment with the anterior communicating artery
Segment A2 of the anterior cerebral artery, through its cortical branches, supplies blood to the anterior 2/3 of the medial surface of the orbital part of the frontal lobe, the pole of the frontal lobe, the strip of cortex along the superomedian border and the anterior 2/3 of the corpus callosum. On the other hand, the A1 segment of the anterior cerebral artery gives off many deep penetrating branches, going mainly to the anterior femur of the internal capsule, the anterior perforated substance, the amygdala, the anterior hypothalamus and the lower part of the head of the caudate nucleus of the brain.
Cerebral infarctions (strokes) in the anterior cerebral artery territory are rare. Blockage (occlusion) of the trunk or segment of the A1 anterior cerebral artery is usually well compensated due to the possibility of collateral blood flow from the opposite side. The most severe disorders occur in cases where both anterior cerebral arteries originate from a single trunk (in the case of a congenital anatomical feature of its structure in the patient), blockage (occlusion) of which leads to the occurrence of an extensive infarction in the anterior cerebral arteries of both hemispheres of the brain.
Clinical manifestations of blockage (occlusion) in the basin of both anterior cerebral arteries include bilateral pyramidal disorders with paraplegia (paralysis of the muscles of the left and right half of the body) and pronounced changes in the psyche due to bilateral damage to the frontal lobes of the brain.
Components of a typical syndrome that develops when the anterior cerebral artery is blocked:
Clinical manifestations | Affected brain structures |
| Contralateral foot and leg paralysis | Motor projection of the leg |
| Less severe contralateral arm paresis | Involvement of the area of the cortical projection of the hand and the fibers coming from it in the corona radiata |
| Cortical lesion leading to loss of sensation in the toes, foot, and leg | Sensory projection of the foot and leg |
| Urinary incontinence | Sensorimotor area of the paracentral lobule |
| Contralateral grasping and sucking reflexes, paratonic rigidity | Inner surface of the posterior part of the frontal lobe - supplementary motor area |
| Abulia (akinetic mutism), slowness, retardation, periodic sudden hesitations, spontaneity, whispered speech, motor inactivity, reflex animation when exposed to visual and sound stimuli | Localization is unclear - probably the cingulate gyrus and the medial parts of the parietal and temporal lobes |
| Impaired walking and standing (gait apraxia) | Frontal cortex near the motor projection of the leg |
| Dyspraxia in the left limbs, left-sided tactile aphasia | Corpus callosum |
Anatomical description of the disease
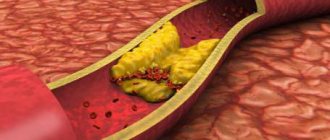
Occlusion of the carotid (carotid) arteries is a partial narrowing or complete occlusion of the large canals supplying the brain. There are episodes of asymptomatic progression, often accompanied by systematic oxygen deprivation of brain areas and arterial strokes. According to medical statistics, ischemia is most often caused by damage to the extracranial parts of the circulatory system. Intracerebral degeneration of vascular tracts is detected four times less frequently. Blockage of the carotid ducts is the cause of ischemic disease of the central nervous system in 56% of cases. A third of all recorded impacts occur as a result of the closure of these channels.
The narrowing of the bloodstream may be partial, then a diagnosis of stenosis is made. When the vessel is completely blocked, a stroke occurs, and sometimes the disease causes sudden death.
Syndromes of thrombosis of the anterior artery of the choroid plexus
The anterior artery of the choroid plexus of the brain begins from the internal carotid artery and supplies blood to the posterior thigh of the internal capsule, as well as the white matter of the brain to the side and behind it, through which part of the optic fibers passes from the lateral geniculate body to the calcarine groove. This area of the brain is also supplied with blood by:
- penetrating vessels coming from the trunk of the middle cerebral artery (arteries of the lenticular nucleus and striatum)
- penetrating branches of the posterior communicating artery
- posterior choroid plexus artery
Therefore, the full clinical syndrome in the form of contralateral hemiplegia (paralysis of the muscles of the body on the opposite side), hemianesthesia (hypoesthesia) and homonymous hemianopsia (loss of half the visual field on the side of the brain lesion) may not develop. Instead, syndromes with minimal severity of neurological focal disorders are observed.
Indeed, in cases of surgical occlusion of the anterior artery of the choroid plexus for the purpose of treating the symptoms of Parkinson's disease, some patients do not show signs of circulatory deficiency in the area of its basin. Patients who initially presented with advanced clinical symptoms often recover fully or partially, apparently due to sufficient levels of collateral arterial blood flow in this part of the brain.
Internal carotid artery thrombosis syndromes
The clinical presentation of cerebral internal carotid artery occlusion varies depending on whether the ischemia is caused by spreading thrombosis, embolism, or low blood flow. Occlusion (blockage) of the internal carotid artery may be asymptomatic. Extensive cerebral infarctions (stroke) involving deep gray and white matter, the cortical surface develop less frequently if the lumen-occluding thrombus extends to the internal carotid artery and penetrates the trunk of the middle cerebral artery and the anterior cerebral artery, or if a separated fragment of the thrombus entails an embolism of the middle cerebral artery. or anterior cerebral artery.
The symptoms are identical to those of blockage of the trunk of the middle cerebral artery. When the anterior and middle cerebral arteries are simultaneously involved in the pathological process, hemiplegia, hemianesthesia and aphasia or anosognosia are often accompanied by stupor. When the posterior cerebral artery arises from the internal carotid artery (fetal posterior cerebral artery), it can also become blocked through the mechanisms described above, which is accompanied by symptoms of damage to its territory.
Atherosclerosis with thrombosis of the internal septal artery can cause a transient ischemic attack (TIA, microstroke) or stroke (cerebral infarction).
With clinically manifested atherosclerosis with thrombosis of the internal carotid artery, regardless of the cause of cerebral ischemia in its basin, most often only the area supplied by the middle cerebral artery suffers. Cerebral infarction (stroke), caused by low blood flow, is often localized in the distal cortical branches of the middle cerebral artery, leading to the development of transient or gradually increasing weakness in the muscles of the pelvic and shoulder girdles and upper limbs. Sometimes transient episodes of cerebral ischemia are observed, accompanied by dysphasia (impaired understanding or reproduction of speech) or hemiparesis (muscle weakness of half the body) lasting 10-15 minutes, followed by regression of these neurological symptoms. The maximum number of such episodes of transient ischemic attacks (TIA) in patients per day reaches 5-10.
When the dominant hemisphere of the brain is involved in transient ischemic attacks (TIA), transient aphasia or dyscalculia (numeration impairment) can be observed. When the non-dominant hemisphere of the brain is involved in the process, transient neglect of half of the body may occur. With a lesion in the area of the lower division of the middle cerebral artery of the dominant hemisphere, pronounced aphasic disorders with fluent jargon are noted, while the patient’s written and oral speech cannot be understood (Wernicke’s aphasia). Even with arterioarterial emboli, neurological symptoms are often transient due to the fact that emboli can cause incomplete occlusion of the trunk or branches of the middle cerebral artery or undergo lysis (dissolution) and are transported in the distal (above the site of lumen blockage) direction.
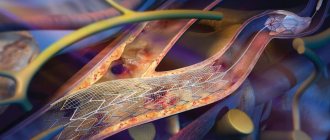
Carotid artery stenting is a minimally invasive procedure that restores proper blood flow to the brain when there is an area of narrowing (stenosis) in one of the carotid arteries. A small metal tube (stent) is passed through the area of stenosis to keep the artery open.
In most cases, it turns out that if neurological symptoms during cerebral ischemia last long enough, but less than 24 hours, then they are caused by arterial embolism. In cases where the neurological symptom of cerebral ischemia is transient (transient) in nature and lasts only a few seconds or minutes, it is usually difficult to distinguish between its embolic and hemodynamic nature.
In addition to the brain, the internal carotid artery supplies blood to the optic nerve and retina through the ophthalmic artery. In approximately 25% of cases of clinically manifested occlusion (blockage of the lumen) of the internal carotid artery, transient blindness occurs occasionally in one eye. In the future, there is a high probability of permanent blindness. Describing such an episode, the patient can tell the doctor about the feeling of a shadow descending and disappearing or crossing the field of vision or about the loss of peripheral parts of the visual fields. There may also be complaints of blurred, blurred vision in the affected eye or the absence of the upper or lower half of the visual field. More often than not, these symptoms last only a few minutes. Less commonly, occlusion (blockage of the lumen) of the ophthalmic artery or central retinal artery is noted simultaneously with a stroke.
Classification and causes of diseases
In some cases, pathologies of the brachiocephalic arteries are provoked by anomalies of the anatomical structure - excessive tortuosity of the vessels or fibromuscular dysplasia. Somewhat more often this occurs against the background of extravasal compression. However, in total, the listed reasons account for no more than 10% of all cases. The remaining 90% of catalysts occur in atherosclerotic lesions.
The causes of disturbances in the activity of the brachiocephalic arteries include:
- Atherosclerosis of the carotid, subclavian or vertebral artery;
- Primary and secondary vasculitis (arteritis);
- Persistent low or high blood pressure (hypo- and hypertension);
- Osteochondrosis of the cervical spine (and associated vascular compression);
- Severe heart pathologies;
- Developmental abnormalities or chronic diseases of the aorta;
- Aneurysms;
- Diabetic angiopathy;
- Vascular malformations;
- Dyscirculatory disorders (including vegetative-vascular dystonia);
- Mechanical injuries to the neck and head.
Atherosclerosis, which is the most common provocateur of diseases, is often caused by third-party endogenous and exogenous factors. These include long-term smoking, mature and old age, hypercholesterolemia, diabetes mellitus, unhealthy lifestyle and poor health in general.
With atherosclerosis of the brachiocephalic arteries, a persistent circulatory disorder in the brain occurs. It varies in intensity and severity, but almost always leads to tragic outcomes. In 80% of cases, such pathologies lead to a major stroke. The importance of timely contact with a cardiologist and vascular surgeon when symptoms are detected cannot be overestimated - sometimes early adequate treatment saves the patient from disability and death.
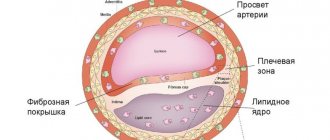
The formation of atherosclerotic plaque in the brachiocephalic arteries is a long process; traditionally it begins at a young age. A neoplasm gradually grows in the wall of a certain vessel, leading to a narrowing of the lumen of the artery, or its complete blockage.
Sometimes specialists diagnose non-stenotic atherosclerosis. This means that the lumen of the vessel is blocked by an atherosclerotic plaque by less than 50%, i.e. the disease does not entail potential critical risks. Without observation and treatment, non-stenotic atherosclerosis transforms into stenotic atherosclerosis, provoking vascular occlusion and serious disruption of the blood supply to the brain.
Common carotid artery thrombosis syndromes
When the common carotid artery is blocked, all the neurological symptoms of internal carotid artery occlusion can be observed. With “pulseless disease” or aortic arch syndrome, occlusion of both common carotid arteries at their exit points is possible.
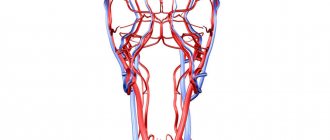
The anatomy of the common carotid and internal carotid arteries provides insight into the mechanism of ischemic stroke.
In the diagnosis of this condition when both common carotid arteries are blocked, the following symptoms are leading:
- absence of pulsation in the carotid and radial arteries
- fainting when rising from a horizontal position
- repeated episodes of loss of consciousness
- headache
- neck pain
- transient blindness (unilateral or bilateral)
- blurred vision during exercise
- early cataracts
- retinal atrophy and pigmentation
- iris atrophy
- leukomas
- peripapillary arteriovenous anastomoses
- optic atrophy
- intermittent weakness of the masticatory muscles
Incomplete aortic arch syndrome is often observed, consisting of various combinations of stenosis and occlusion of the carotid, subclavian and innominate arteries.